One of the obvious signs of heart failure is the presence of edema. This disease is characterized by stagnation of fluid in the body, which leads to edematous conditions. The main feature of such conditions is that fluid accumulation can be observed in any part of the body. The localization of edema depends on the nature of the cardiac dysfunction. So, when the left side of the heart is affected, there is an accumulation of fluid in the lungs. This leads to difficulty breathing and shortness of breath. If the right side of the heart is affected, salt accumulates in the body, which delays the outflow of fluid. As a result, swelling of the lower extremities is observed.
Localization Features
The essence of tissue congestion is hypoxia with the development of the nose, which indicates the presence of excess fluid in the body. Depending on the location of the edema, clinical symptoms indicate the severity of heart failure. The worse the heart works, the more local the swelling.
In the initial stage of the disease, tissue swelling is interrupted; in later stages it becomes a solid phenomenon. Swelling of the abs and legs occurs first, then the lower part of the legs, swelling then expands to the arms, face and most severely to the entire body.
The tumor has its own characteristics:
- Pastosity appears in the evening and is associated with prolonged physical stress, which is unbearable for the heart;
- The affected areas become dense, cold and shiny blue;
- swelling is always symmetrical;
- The emphasis on the pasty skin causes depressions under the fingers that overwhelm spontaneous liquefaction;
- The patient's weight increases;
- In compensated edema, it gives way in the morning, in decompensated HF it supports and shows that internal organs such as the liver, peritonis and chest organs are affected.
Diagnostics
It is carried out under the supervision of a cardiologist; depending on the stage of the process, the examination can be carried out in an inpatient or outpatient setting. The issue is resolved at the discretion of specialists.
Approximate list of events:
- Oral questioning of the patient. Allows you to objectify symptoms and create a clear clinical picture. Used as part of routine initial examination.
- Anamnesis collection. Briefly. What illness did the person have when? How long. Lifestyle, family history, and other points are also clarified. Both methods are basic. They are necessary to determine the vector of further actions.
- Auscultation, listening to heart sounds. If insufficiency, and, as a consequence, swelling of the legs occurs against the background of a defect in the cardiac structures, dull irregular tones and splitting are detected.
- Measurement of blood pressure and heart rate. The first indicator is consistently below the norm, because the symptoms of burning contractile function are increasing. Heart rate is first of the tachycardia type, that is, acceleration, then the reverse process.
- Daily monitoring. Usually prescribed as part of a comprehensive diagnosis. Records vital signs for 24 hours. Dynamic observation.
- Electrocardiography. Brings to the surface arrhythmias and possible defects. But decoding requires high-quality training of specialists.
- Echocardiography. Shows deviations of the anatomical plan.
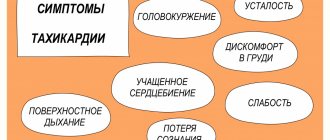
Associated symptoms
In addition to swelling, other symptoms also occur:
- Chest pain radiating to the shoulder or referral area (this symptom may be preceded by swelling);
- Hypertension is caused by stable and congested blood vessels;
- Increased liver volume with pain in the right sublayer;
- weakening of muscles due to constant hypoxia, which can lead to their disappearance;
- Dyeness in heart failure is caused by the filling of blood in the respiratory vessels, stacked in small circulation and deterioration of gas exchange (in the worst case there is pulmonary edema with a lethal effect);
- Abnormal heart rhythm, palpitations;
- acrocyanosis of the unnatural skin palace;
- the ability to perform any physical activity decreases;
- “Finger shins to hands indicate late stage HF with pulmonary failure;
- Dizziness is the result of cerebral hypoxia;
- Impairing cognitive function.
Even one symptom is a reason to see a doctor.
Treatment of cardiac edema in the elderly
At the first signs of edema of the lower extremities, you should consult a cardiologist, since the initial cause of this pathology may be the heart. The doctor will conduct an examination of the body, suggest taking appropriate tests and, based on your clinical picture, prescribe the correct treatment for cardiac edema in older people.
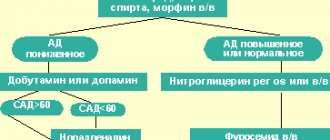
For this pathology, patients can be offered therapy either orally in the form of tablets or intramuscularly/intravenously in the form of injections. The doctor may also prescribe medications for external use.
- Oral medications
Treatment of cardiac edema in older people should be selected correctly and with an emphasis on restoring and stabilizing cardiac activity. The following types of medicines are used in the fight against the disease.
To reduce blood pressure (BP) and total peripheral resistance (TPSR), ACE inhibitors are used:
- "Captopril."
- "Ramipril."
- "Lysoreticist."
- "Irumed."
- "Perindopril."
- "Enap".
Drugs for blocking beta-adrenergic receptors - beta-blockers:
- "Nebilet."
- "Bisoprolol."
- "Nebivolol".
- "Coriol."
- "Cardevilol."
Aldosterone receptor antagonists:
- "Eplerenone."
- "Veroshpiron".
- "Spironolactone".
- "Aldactone".
- Glycosides: Digoxin, Korglykon.
- Potassium preparations (for the treatment and prevention of blood pressure abnormalities): “Asparkam”, “Panangin”.
We recommend
“Why blood pressure drops in older people: causes and treatment” Read more
To relieve swelling, the doctor can also prescribe diuretics (orally or by injection):
- "Piretanide".
- "Britomar."
- "Hydrochlorothiazide."
- "Bumetanide".
- "Lasix."
- "Furosemide".
- "Torasemide".
- "Hypothiazide."
- "Triphas"
- Ethacrynic acid.
Sartans, angiotensin receptor blockers:
- "Lorista".
- "Mikardis".
- "Teneten Plus"
If, during the treatment of cardiac edema in elderly people, problems arise with blood viscosity, the specialist has the right to prescribe drugs that help thin it. Never take medications yourself, as this can lead to bleeding and even death. If your blood pressure is high, your doctor will recommend appropriate medications. Do not self-medicate and follow the doctor's orders.
- External means.
To relieve pain symptoms due to cardiac edema, ointments, gels and creams are used that improve blood circulation in the lower extremities and reduce heaviness and pain in the legs.
Means for normalizing blood circulation include the following:
- "Lyoton."
- "Venitan."
- "Menovazin".
- "Troxerutin."
- Heparin ointment.
- "Troxevasin".
Do not forget that self-medication leads to dangerous consequences, so use all medications only after consultation with your supervising doctor.
In addition to external remedies, tablets and injections, it is necessary to do warm, relaxing foot baths and light circular massages. At least two or three times during the day, you need to find time to lie down in a horizontal position, and raise your legs up and place them on a hill (you can put a pillow under them), thereby ensuring the outflow of blood.
One way to relieve heavy legs is to wear special compression stockings or elastic bandages. Remove all tight shoes, which only aggravate the disease. Do special relaxing exercises for the lower extremities. Walk barefoot more often and choose comfortable orthopedic shoes for your feet.
- Traditional medicine.
Cardiac swelling in older people can also be treated with folk remedies, such as decoctions of chamomile, calendula, viburnum, lingonberry, and birch buds.
All these herbs have diuretic properties, thereby cleansing the body and starting metabolic processes. These traditional medicine options are used in the form of a decoction or tincture. They drink them in courses and always with breaks. Over the years, people have passed down recipes for these compounds from generation to generation. Let's give a few examples.
- A decoction of plantain leaves, rose hips, nettle leaves and bearberry. For preparation you will need 10 g of these plants, 500 ml of boiling water. Brew for 5–7 minutes, let steep, strain and drink within 24 hours.
- One of the working diuretics in folk medicine is considered to be a decoction of flax seeds. You need to take 20 g of seeds per 1 liter of water and boil for 10–12 minutes. Then leave for about five minutes, cool, strain and pour a little lemon juice into it. Drink 150 ml every two hours.
- A decoction of hawthorn fruit is also useful for swelling. It is easy to prepare. It is necessary to pour boiling water over the berries for 10–12 minutes, then cool and let it brew in a dark place. You need to drink 100 g of it before meals, after adding a little honey.
- A tincture of parsley inflorescences is very useful. It is necessary to grind the herb, pour boiling water over it, and let it brew for 5-6 hours. Applied by the course.
- For swelling of the lower extremities, it is also useful to take soothing and relaxing baths with herbs such as sage, chamomile, and mint leaves. The duration of one procedure is 30–40 minutes.
You should use traditional medicine only in consultation with your doctor, do not allow amateur activities!
We recommend
“Low blood pressure in older people: causes, symptoms and treatment” Read more
When treating cardiac edema in older people, you need to seek help from a competent and qualified specialist who will tell you how to combine pharmaceutical and home medications so as not to cause harm or aggravate the pathology.
- Diet.
To maintain the water-salt balance in the body, it is advisable to first eliminate salt from the diet. It is also recommended to remove dishes high in spices, pepper and sugar from your menu. Tea, coffee and other drinks are diuretics; they wash away beneficial substances, so you should not get carried away with them. You need to drink plain water so as not to upset the balance in the body and not strain the heart muscle.
There are certain recommendations for nutrition: food should be steamed or stewed in its own juice with the addition of liquid, and do not overuse salted, smoked, fried and pickled foods. It is necessary to eat foods containing potassium, for example, nuts, dried apricots, almonds, peas.
With this pathology, you need to eat according to diet No. 10 (table No. 10), intended for people with heart disease. This diet involves a balanced five-course menu with reduced salt consumption. The serving size for women is 200 g, for men – 300 g. By eating according to diet menu No. 10, you can improve blood circulation, reduce cholesterol, increase the body’s performance, and improve metabolic processes.
The diet is allowed to include dairy and seafood, greens, eggs (no more than one per day), vegetable, dairy and fruit soups, almost all types of cereals, gray and black bread, whole grain bread. It is advisable to eat vegetables boiled or stewed, but very rarely raw. It is prohibited to consume pickled and pickled foods, legumes, pasta, salted vegetables, strong tea, mushrooms, salted cheeses, and pork.
Difference between renal and cardiac pastosity
Heart failure applies to all internal organs, but renal edema is considered the most dangerous and should be distinguished from heart failure:
- Edema of the legs, cubes, lower extremities, arms, face and body is characterized by upward spread. In the case of renal pathology, the location of the swelling is posterior: starting from the face and gradually going down to the legs.
- Heart swelling occurs in the evening with physical fatigue; renal edema, on the contrary, occurs in the morning and is replaced by the evening.
- In the case of the title, the skin is cold and in the case of the kidneys there is swelling.
- If the finger is compressed with swelling, the hole is painful and closes after a long time, while in the case of renal edema it is painless and the hole disappears almost immediately.
- Needle swelling is almost always accompanied by pain in the lower back, and Christmas swelling is pain behind the bridge.
But, of course, only laboratory and instrumental diagnostic tests - OAC, OAB, biochemistry, ECG, physical exercise and ultrasound tests - will give an accurate answer.
Features of therapy
Treatment for swelling in heart failure is to eliminate their causes. It is quite difficult to treat such a disease, but it is possible to overcome it. If you are able to stop the progression of heart failure, the patient's condition will return to normal. At the initial stage, it helps to reduce swelling through rest, weight massage and cold wraps. Then more radical therapeutic methods are used.
First of all, diuretics are used to remove excess fluid from the body. They can be synthetic drugs: furosemide, diacarb, Triampur, spironolactone, diuretics or natural Veroshpiron: a decoction of birch buds, cherry stems, flowers, cornflower, dandelion, parsley. The choice of treatment method depends on the stage of heart failure and the severity of clinical symptoms.
Swelling in the legs with heart failure, they can be controlled by cardiac glycosides: Celanid, digoxin, Corglicon. It improves myocardial contractility, stopping congestion and helping to remove excess water from the body.
RLO is also used: Valsacor, Mycardis, which lowers blood pressure, which reduces the release of fluid into the tissue and prevents pastozie. Effective potassium and magnesium preparations: Panangin, Asparkam, which restore heart rhythm, regulate vascular blood flow, restore the transmission of nerve impulses to the muscles.
Beta-adrenoblokery: Concor, Betaloc, nebilet, Corvitol are necessary for correcting heart rhythm, improving nutrition and oxygen supply to important internal organs.
Angioprotectors: Detralex, Troxevasin, diosmin, Escusan, Antistax strengthens the walls of blood vessels, normalizes regional blood flow, the cellular composition of the blood is stabilized, reduce pastowatość.
Treatment of edema syndrome in chronic heart failure
For citation. Efremova Yu.E. Treatment of edematous syndrome in chronic heart failure // Breast Cancer. 2015. No. 27. pp. 1622–1624.
According to the European Society of Cardiology guidelines, heart failure is defined as a consequence of disturbances in cardiac structure and function that result in the inability of the heart to deliver oxygen at a rate comparable to the metabolic needs of the tissues, despite normal filling pressures [1]. Chronic heart failure (CHF) is a syndrome that results from various causes of myocardial damage. The main causes of CHF are coronary heart disease and arterial hypertension (AH), less often - cardiomyopathy, valvular heart disease, pericardial disease, etc. The prevalence of CHF in the age group of 25–54 years is 1%, in the group of 65–74 years – 4– 5%, about 10% – in people over 75 years of age. Compared to 20 years ago, there is evidence of a 4-fold increase in hospitalizations for CHF. This is partly explained by an increase in average life expectancy [2]. According to the results of the Russian epidemiological study EPOCHA-CHF, the prevalence of CHF in Russia averages 7.9%, including clinically significant - 4.5%, increasing from 0.3% in the age group from 20 to 29 years to 70 % in people over 90 years of age [3]. Having heart failure increases the risk of death by 4 times. Treatment of patients with CHF is a difficult task in modern medicine, since heart failure is only a syndrome that can develop as a complication of many diseases of the cardiovascular system. Therapy for a patient with CHF should first of all include treatment of the underlying disease. The main goal of treatment of CHF is to reduce mortality, as well as [2]: – reduction of clinical symptoms of CHF; – reduction in the incidence of major complications; – maintaining or improving the patient’s quality of life; – improvement of left ventricular function; – increased exercise tolerance; – reducing the need for hospitalization; – prevention of side effects of therapy. Drug treatment of CHF includes a large number of drugs, the most common of which are angiotensin-converting enzyme inhibitors (ACE inhibitors); angiotensin II receptor blockers; diuretics; β-blockers and mineralocorticoid receptor antagonists (aldosterone antagonists). The use of a specific drug in the treatment of CHF is aimed at solving specific problems. Let us consider in more detail the treatment of edema syndrome in CHF using diuretic therapy. Peripheral edema in heart failure is a consequence of fluid retention caused by reduced renal blood flow and neurohormonal changes. They predominantly develop on the lower extremities. With significant fluid retention, ascites and/or hydrothorax may be present. Diuretics are used to treat edema syndrome. Drugs of this class are indicated for all patients with clinical symptoms of CHF associated with excessive retention of sodium and water in the body [4]. Diuretics are used for the symptomatic treatment of CHF. They prevent fluid retention in the body, increase the excretion of salt and water, which leads to a decrease in congestion. Against the background of their use, the total peripheral vascular resistance decreases, the pre- and afterload decreases, and therefore the dilatation of the left ventricle decreases. There are 5 classes of diuretics (Table 1) that act on different parts of the loop of Henle. In the initial stages of CHF, the use of thiazide diuretics is possible. In severe CHF, a combination of loop and thiazide diuretics is possible, which leads to an increased diuretic effect. In case of severe edema syndrome and/or decompensation of CHF, it is advisable to administer diuretics parenterally. The loop diuretics furosemide and torsemide are the most commonly used diuretics for CHF.
Torsemide has been used in clinical practice since the 1980s. For edema syndrome, this drug is prescribed 5 mg in the morning after meals; if necessary, the dose is increased to 20 mg 1 time/day. Compared with furosemide, torasemide is characterized by higher bioavailability, which does not decrease with edematous syndrome, has less effect on the plasma concentration of potassium and magnesium, acts longer and has anti-aldosterone properties (blockade of aldosterone receptors on the membranes of epithelial cells of the renal tubules and decreased secretion of aldosterone in the adrenal glands) . The pleiotropic properties of torasemide include the ability of this drug to inhibit the synthesis and deposition of type 1 collagen in the myocardium in patients with CHF. In addition, unlike patients receiving furosemide, patients in the torasemide group had a decrease in the serum concentration of the C-terminal propeptide of type 1 procollagen (a marker of myocardial fibrosis) [6]. Torsemide reduces mortality, as well as the frequency and duration of hospitalizations for CHF. In addition, it leads to increased exercise tolerance, improves the functional class (FC) of CHF (according to NYHA) and the quality of life of patients. In the TORIC study among 1377 patients with CHF, torasemide led to a significant reduction in cardiovascular mortality compared with furosemide [7]. This study analyzed the results of a 9-month comparative treatment with torasemide at a daily dose of 10 mg and furosemide 40 mg in patients with CHF. In the group of patients receiving torsemide therapy, the FC of circulatory failure improved significantly more often and cardiovascular and overall mortality significantly decreased. Recently, slow-release torasemide has appeared on the Russian drug market - Britomar
®. The drug provides gradual release of the active substance. Due to this, fluctuations in the concentration of the drug in the blood are reduced compared to the usual form. Britomar® is a tablet based on a hydrophilic matrix of guar gum, which is a natural water-soluble polymer obtained from the seeds of a plant of the legume family. In the pharmaceutical industry, guar gum is widely used to create sustained-release dosage forms. In the gastrointestinal tract it forms a kind of sponge, which provides a slow release of the drug. The drug substance is released over a longer period of time, due to which diuresis begins approximately 1 hour after taking the drug, reaching a maximum after 3–6 hours, the effect lasts from 8 to 10 hours. Slow release of the drug allows for additional clinical benefits in the treatment of edema syndrome in CHF. Torsemide, when used long-term, does not cause changes in blood potassium levels, does not have a noticeable effect on calcium and magnesium levels, glycemic and lipid profiles [8]. The drug does not interact with anticoagulants (warfarin), cardiac glycosides or organic nitrates, other drugs most often used in the treatment of CHF, such as β-blockers, ACE inhibitors, angiotensin II receptor blockers and mineralocorticoid receptor antagonists. Long-acting torasemide has been studied in a number of studies in comparison with other diuretics. Thus, in a Russian single-center, randomized, open-label study, the comparative effectiveness of long-acting torasemide and furosemide was studied in patients with class II–III CHF, edematous syndrome, and elevated levels of natriuretic peptides [9]. The study included 40 patients with CHF of ischemic etiology with a left ventricular ejection fraction of less than 40%, divided by randomization into 2 equal groups: the 1st received long-acting torasemide (Britomar®), the 2nd received furosemide. In both groups, during treatment, a significant improvement in exercise tolerance, an improvement in the quality of life of patients, and a decrease in the concentration of natriuretic hormones were observed. In the torasemide sustained-release group, a trend towards a more significant improvement in quality of life (p=0.052) and a significantly more significant decrease in NT-pro-brain natriuretic peptide levels (p<0.01) were identified. This may be due to the fact that extended-release torasemide has a slow onset of action, does not lead to the development of urinary urgency, and has a longer duration of action compared to the standard-release dosage form [9]. This study also examined data on the effect of diuretic treatment regimens on the electrolyte profile of patients. Potassium and sodium concentrations were determined at baseline, 2, 4 and 12 weeks. treatment. There were no cases of changes in the electrolyte profile compared to normal values in the torasemide extended-release group. In the furosemide group, 3 (15%) patients experienced a decrease in potassium levels below normal limits (3.5 mmol/l), in 1 case requiring dose adjustment of aldosterone antagonists and intravenous infusion of potassium salts. Undoubtedly, reducing the frequency of hypokalemia also has an impact on both the well-being of patients and the frequency of potential complications of therapy. While taking long-acting torasemide, the phenomenon of increased post-diuretic sodium reabsorption can be avoided. The absence of a rapid increase in the volume of excreted urine does not cause a sharp change in the volume of circulating blood, and therefore does not potentiate the excessive synthesis of A-II and norepinephrine, which lead to a decrease in the glomerular filtration rate and deterioration of renal function. The benefits of extended-release torasemide compared with standard-release torsemide have been demonstrated in a number of studies. In a study by MJ Barbanoj et al. a comparative assessment of bioavailability and bioequivalence was carried out and the pharmacokinetics and pharmacodynamics of torasemide sustained and standard release were assessed [11]. Two doses of extended-release torsemide were compared with similar dosages of torasemide. 20 healthy volunteers (2 groups, 10 people each) took part in the study. As a result, sustained release torasemide showed a significantly longer tmax compared to that of torsemide. The amount of torasemide detected in urine 24 hours after administration was higher in the sustained-release torasemide group at both dosages. Urine volume and urinary electrolyte excretion were lower in the sustained-release torasemide group during the first hour after dosing, but natriuresis was significantly greater in this group. Thus, although both forms showed similar systemic distribution (AUC), sustained-release torasemide had a lower absorption rate (smaller C (max) and prolonged t (max)). In a pilot study by G.P. Arutyunova et al. a comparison of sustained release torasemide with standard release torasemide was also carried out [12]. This open, randomized, comparative clinical trial in parallel groups included patients with FC I–II CHF (NYHA) and grade II–III essential hypertension. Using the random number method, patients were divided into 2 treatment groups - treatment with Britomar and standard release torsemide. The treatment period lasted 40 days. As a result, it was shown that the total natriuresis on the 1st day of administration of Britomar and torasemide standard release was greater in the second group, however, it is important that in the Britomar group a smooth natriuresis was observed during the day without peaks, in contrast to the standard form of torasemide, when prescribed which causes a peak increase in natriuresis at 3 hours and a sharp decrease already at 6 hours with a further progressive decrease. It was also shown that natriuresis following a single dose of a loop diuretic lasted only a few hours, and after 5-6 hours, urinary sodium excretion approached a level comparable to that with placebo, i.e., from 6 to 24 hours, even torsemide is ineffective , and its cumulative natriuresis is comparable to that of hydrochlorothiazide precisely due to the presence of an antinatriuretic period. A beneficial effect of Britomar on central hemodynamic parameters was demonstrated, which the authors associate with the absence of rebound sodium retention when using this diuretic, and therefore an increase in the rigidity of the vascular wall. Thus, sustained-release torasemide, due to its pharmacodynamics and pharmacokinetics, is a highly effective drug in the treatment of edema syndrome in CHF and can improve the quality of life of patients and the tolerability of therapy.
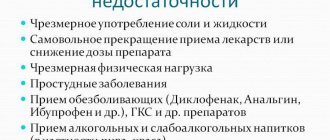
Additional events
Leg swelling due to heart failure can be alleviated
- reduce salt intake to 5 g/day;
- a balanced diet, drinking water up to 1.5 liters of liquid per day, including the first and third courses, medicinal tea, milk;
- as far as possible, protein foods should be included in the daily diet instead of carbohydrates and fats;
- in order to normalize your weight;
- Participation in physical activity should be limited, with the exception of heavy physical labor.
Is it possible to stop the syndrome for a long time?
Unfortunately, the answer is clearly no, not heart failure, not even mild. Mild CH can be controlled and its progression stopped by following all the doctor's instructions. If the extension of the process is stopped, the papillary tumor will also disappear. In this case, it will be necessary to use drug therapy for life, abandoning periodic preventive treatment in health resorts.
Late-stage SNA is difficult to stop, as well as any accompanying symptoms, including swelling. This depends on the ability of the heart muscle to compensate. Even surgical interventions that are performed only to preserve vital functions are not able to completely eliminate negative symptoms and are rather used to maintain the functionality of the cardiovascular system: valve replacement, pacemaker implantation, coronary bypass surgery, stenting.
This fact once again demonstrates the need for a responsible approach to one’s own health and to consult a doctor at the first negative symptoms.
Causes of edema in cancer
The development of edema occurs as a result of an imbalance in the release of plasma cells into the tissue from the bloodstream.
Normally, the liquid should be completely absorbed by the venous capillaries, only in a “waste form”. Only 1/10 of the plasma should remain in the intercellular space, leaving a little later into the lymphatic channel. Malignant processes occurring in the body cause an imbalance. Vascular structures become “clogged” with cancer cells, and lymphatic vessels stop “pumping” lymph. This mechanism is typical mainly for cervical cancer, when metastases have already spread to the pelvic and inguinal lymph nodes. A similar process occurs after surgery on the mammary gland for lymphedema (lymphostasis with complete removal of the lymph nodes of the armpits).
Swelling due to cancer also occurs in the case of an inoperable tumor, if there is an enlargement of regional lymph nodes due to metastasis. They stop functioning properly, squeezing large vessels. This condition is often aggravated by a bleeding disorder.