What is extrasystole
Extrasystole
is a variant of cardiac arrhythmia, characterized by extraordinary contractions of the entire heart or its individual parts (extrasystoles). It manifests itself as a feeling of a strong heartbeat, a feeling of a sinking heart, anxiety, and lack of air. A decrease in cardiac output during extrasystole entails a decrease in coronary and cerebral blood flow and can lead to the development of angina pectoris and transient cerebrovascular accidents (fainting, paresis, etc.). Increases the risk of developing atrial fibrillation and sudden death.
Mechanism of heart contraction
The function of the regulator of the number of heart contractions is performed by the conduction system of the heart, which consists of the following elements and structures:
- sinoatrial (sinoatrial) node;
- muscle tracts;
- internodal atria;
- atrioventricular node;
- atrioventricular bundle.
The impulse that excites cardiac contraction begins from the sinoatrial node. Then the excitation is transmitted along the internodal pathways of the atria, provoking their depolarization, approaches the atrioventricular node and is transmitted through the atrioventricular bundle to the muscles of the ventricles. At the slightest failure of the impulse strength in any part of the conduction system, episodic or organic disruptions of the heart rhythm (extrasystoles) may occur.
Extrasystole disease
Extrasystoles (extrasystoles) are atypical depolarization and premature contractions of the heart or its individual chambers. As a rule, patients diagnosed with extrasystole experience a short-term freezing of the heart rate, lack of air and an intense cardiac impulse. Such abnormal heartbeats and pauses between contractions provoke an impulse outside the cardiac sinus node.
Differential and etiological diagnosis of extrasystole is difficult in cases where heart rhythm disturbances are a side effect of another cardiovascular disease. When extrasystole occurs, it is imperative to undergo a full diagnosis and evaluate the functional state of the myocardium.
Types of extrasystoles
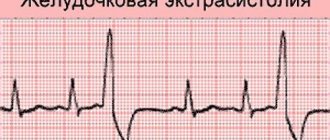
Premature heart contractions (complexes) according to the mechanism of occurrence are: parasystoles and extrasystoles. The differences between the types are clearly visible on daily ECG
.
In cardiology there are:
1. Functional extrasystoles. Diagnosed in people with signs of neurosis or autonomic dysfunction. Such extrasystoles are recorded at rest; during emotional outbursts or after physical activity, atypical complexes cease. With a functional malfunction of the heart rhythm, patients may feel extrasystoles: tremors behind the sternum, hot flashes, anxiety, discomfort and lack of air. In most cases, the development of functional extrasystoles is benign. On ECG
at the same time, gastric monotopic changes are recorded.
2. Organic extrasystoles. Typical for elderly patients. As a rule, organic extrasystoles accompany endocrine disorders, heart disease, and chronic intoxication. Subtle signs of premature heart beats occur after stress or exercise. Such complexes do not prevent patients from leading an active lifestyle. Cardiac contractions of high gradations are organic in 95% of cases. On ECG
at the same time, ventricular, polytopic, atrial, atrioventricular and group extrasystoles are recorded.
Bigeminy
Bigeminy in cardiology refers to a certain type of supraventricular (supraventricular) or ventricular extrasystole. This type of arrhythmia develops due to dysfunction of the autonomic and central nervous system. The main cause of bigeminy is organic changes in the heart muscle. Even small deviations in the myocardium with extracardiac origin and associated factors provoke the appearance of an ectopic focus of excitation.
Ventricular bigeminy is characterized by uniform alternations of a normally occurring contraction with a single ventricular extrasystole, which is a type of allorhythmia. Untimely excitation of the right cardiac ventricle is also recorded. Supraventricular bigeminy is a paired alternation of one rhythmic contraction and one extrasystole.
The diagnosis of “bigeminy” is common in rheumatic heart defects (mitral valve prolapse and aortic stenosis). The disease often accompanies cardiomyopathies, myocarditis and thyrotoxicosis.
Classification of extrasystoles
Depending on the area of localization and ectopic foci of excitation, extrasystoles are distinguished:
- Atrial.
- Ventricular
- Atrioventricular and nodal (atrioventricular).
- Sinoatrial (sinus extrasystole).
Extrasystole can have one or more sources of excitation. The following types of extrasystoles are diagnosed:
- Monotopic - with one focus of development and a stable interval in areas of the cardiogram.
- Polytopic - several centers of occurrence and different intervals of linkage.
- Unstable paroxysmal tachycardia is a series of extrasystoles following each other.
Today, several classification systems for arrhythmias are used in medicine. The most common modified version of the “Lown & Wolf” gradation offers the following classification of ventricular extrasystoles:
- I-class – single extrasystoles with repetition less than 30 units/hour. This arrhythmia is not life-threatening and does not require correction.
- Class II – single extrasystoles with repetition over 30 units/hour. Minor deviations from the normal heart rate do not lead to serious consequences.
- Class III – polymorphic extrasystoles. Cardiac complexes of various shapes with a large number of episodes require therapeutic correction.
- IVa-class - paired extrasystoles following each other. High grade class with pathological consequences.
- IVv-class – volley extrasystoles (3-5 in a row). High grade class with irreversible consequences, posing a danger to life.
- V-class – early extrasystoles (R, T). A high grade class that leads to cardiac arrest.
Forecast
Prognostic data varies.
Favorable factors:
- No impairment of myocardial contractility.
- Normal conduction of structures and bundles of His.
- Adequate response of the body to treatment.
- Early initiation of therapy.
In general, the forecast can be formulated this way. Single pathological contractions are eliminated in 100% of cases, risks are determined at 2-5%. Multiple are characterized by the likelihood of fatal complications described above in 25-30% of situations. Prospects: 3-5 years from the onset of the first symptoms.
Causes of extrasystole
Extrasystoles are the most common subtype of arrhythmia, which periodically occurs in 65% of absolutely healthy people. With a normal heart rhythm there should be about 200 ventricular and 200 supraventricular extrasystoles per day. At moments of failure, up to tens of thousands of extrasystoles are recorded.
The nature of extrasystole can be organic (there are cardiac pathologies) or neurogenic (functional). Functional extrasystole develops when:
- Stress.
- Neuroses.
- Taking medications.
- Cervical osteochondrosis.
- Neurocirculatory dystonia.
- Intense physical activity.
- Abuse of nicotine, alcohol, caffeine-containing drinks.
An episodic increase in the number of daily extrasystoles does not pose a danger to healthy people; such surges in medicine are called “cosmetic arrhythmias.” Heart rhythm disturbances must be monitored and corrected in patients with organic heart pathologies.
Causes of organic extrasystole:
- Cardiosclerosis.
- Heart defects.
- Myocardial infarction.
- Inflammatory process.
- Cardiac ischemia.
- Ion metabolism disorders.
- Circulatory failure.
- Systemic diseases involving the heart.
The mechanism of pathology development
First you need to turn to the basics of physiology and anatomy. The heart is a muscular organ. Its cells, the so-called cardiomyocytes, are capable of spontaneous excitation.
Therefore, cardiac structures are disposed to work fully without external stimulation. The speed of contractions is partly regulated by the brain and, to a lesser extent, by hormonal substances.
The generation of an electrical impulse takes place in a special cluster of cytological units: the sinus node. This is a normal natural phenomenon.
If there are lesions in the heart itself or other systems, it is possible that a signal can be generated in other, atypical places.
The most common location of extrasystoles is the atria (exactly the location described). Unlike other types of problems, this one is not so lethal, although the degree of danger should be determined by the nature of the process.
Frequent supraventricular extrasystoles develop in response to stimulation of cardiac structures from the outside or as a result of defects, congenital and acquired. The longer the duration of the pathological process, the higher the likelihood of fatal complications.
Symptoms of extrasystole
The difficulty in diagnosing extrasystole lies in the absence of a characteristic, pronounced clinical picture. Symptoms depend on the state of the vegetative-vascular and cardiac systems, the age of the patient, the reactivity of the body and the form of the disease. In 70% of patients, arrhythmia is detected during a routine examination.
In case of serious pathologies, vegetative-vascular dystonia and heart diseases, extrasystole is manifested by the following symptoms:
- Heart pain.
- Anxious state.
- Strong heart beats.
- Increased sweating.
- Thrusts to the chest.
- Freezing of heart rate.
- Feeling of lack of air.
- Paleness of the skin.
Frequent heart contractions of a group or early nature provoke a decrease in cardiac output and a slowdown in cerebral, coronary and renal circulation. In patients with cerebral atherosclerosis, the following occurs:
- Aphasia.
- Paresis.
- Fainting.
- Dizziness.
In coronary heart disease, extrasystoles cause angina attacks.
Forecasts for patients with extrasystole
The duration and effectiveness of therapy, as well as the normal functioning of the patient after undergoing treatment, largely depend on ventricular dysfunction and the degree of pathology of the heart muscle. The most dangerous are considered to be extrasystoles provoked by myocarditis, cardiomyopathy, and acute myocardial infarction. Against the background of pronounced morphological abnormalities of the myocardium, cardiac complexes turn into ventricular or atrial fibrillation.
The course of supraventricular extrasystoles complicated by other diseases leads to the appearance of atrial fibrillation. The development of ventricular extrasystoles is dangerous due to persistent tachycardia and sudden cardiac arrest.
In healthy patients with no congenital or developed diseases of the cardiovascular system, extrasystole does not significantly affect the state of health, activity and lifestyle.
If you experience similar symptoms, consult your doctor
. It is easier to prevent a disease than to deal with the consequences.
Signs
With supraventricular extrasystole there are often no complaints. In some cases, the disease causes the following symptoms:
- lack of air, shortness of breath;
- interruptions in the work of the heart: a feeling of “reversals” of the heart or beats out of rhythm;
- dizziness;
- general weakness.
In children, supraventricular extrasystole most often occurs without any symptoms. Complaints usually come from older children. The child may experience weakness, irritability, fatigue, dizziness, and a feeling of heart failure.
Diagnosis of extrasystole
A preliminary diagnosis of “extrasystole” is made by a specialist based on an initial examination and collection of an anamnesis of the disease: genetic predispositions, already diagnosed pathologies and patient complaints.
To confirm the diagnosis and select a therapeutic regimen, the patient is prescribed:
- ECG
. - Bicycle ergometry
. - Load test.
- ECG-Holter (24-hour monitoring)
. - Ultrasound of the heart
(if necessary). - MRI (if necessary).
Based on the diagnostics performed, the cardiologist clearly sees the foci of occurrence and the type of extrasystoles (atrioventricular, ventricular or atrial).
Treatment of extrasystole
Is it necessary to treat extrasystole?
A single heart rhythm disturbance can be caused by a rush of adrenaline or excessive caffeine consumption. Functional extrasystole, which occurs occasionally and does not cause discomfort to the patient, does not require treatment. For women, the physiological norm is cases of extrasystole a few days before menstruation and during ovulation.
Patients with vegetative-vascular dystonia may have a discomforting manifestation of extrasystoles. If abnormal heart rhythm is difficult to tolerate, it is necessary to reduce intense exercise, give up stimulants, be less nervous and include foods rich in magnesium in the diet.
With existing heart defects, cardiomyopathy
, coronary disease and other types of arrhythmia, extrasystoles aggravate the course of the disease, entail fibrillation of the ventricles or atria of the heart and are dangerous to the patient’s life. In such cases, a comprehensive scheme of therapeutic effects on the cardiovascular system of the body is required.
A sinking heart may be a sign of an overactive thyroid gland (hyperthyroidism). Excessive production of thyroid hormones poisons the circulatory system and the entire body, the heart muscle also reacts to the irritant.
Treatment of extrasystoles
Extrasystoles over 200 units/day should be alarming; systemic excess of the norm requires therapeutic correction. The treatment method for heart rhythm disturbances depends on the state of the cardiovascular system, etiology, severity of symptoms and side pathologies.
Stages of treatment:
- The normal functioning of the gastrointestinal tract and endocrine system is controlled.
- Foods rich in magnesium are added to the diet: lettuce, nuts, persimmons, dried apricots, raisins, prunes, cereals, bananas, apples, seaweed, beans.
- The load is adjusted: preference is given to walking at a moderate pace, swimming, and cycling.
- For patients with sleep and performance problems due to heart fluctuations, the cardiologist may prescribe tranquilizers or sedatives.
Complications and dangers of extrasystole
The danger of frequent group extrasystoles lies in their degeneration. Ventricular oscillations are transformed into paroxysmal tachycardia and ventricular fibrillation, and atrial oscillations, during dilatation, are transformed into atrial flutter or atrial fibrillation. Undiagnosed extrasystoles in time lead to chronic failure of the renal, coronary and cerebral circulation.
Algorithm of action in case of a sudden attack of arrhythmia:
- Provide access to fresh air, loosen tight clothing.
- Relax, calm down, take a horizontal position.
- In a stressful situation, take valerian, motherwort or Corvalol. For patients with frequent attacks of anxiety and fear, a neurologist can prescribe Persen, Gidozepam.
- If the condition worsens, you must call emergency help.
Kinds
Variants of supraventricular extrasystoles, taking into account the most important characteristics, are shown in the table:
| Type of extrasystoles | What does it mean |
| Atrial | Arise from the atria |
| Atrioventricular | Arise from the septum between the ventricles and atria |
| Monotopic | One source of impulses |
| Polytopic | Two or more sources of impulses |
| Early | Coincides with atrial contraction |
| Late | Coincides with ventricular contractions |
| Single | Frequency less than 5 times per minute |
| Multiple | More than 5 times per minute |
| Group | Several extrasystoles in a row |
Prevention of heart rhythm disturbances
The basic rules of prevention are:
- Therapy of concomitant pathologies of the cardiovascular, circulatory, endocrine and nervous systems.
- Do not self-medicate and do not take strong tranquilizers, hormones, or sedatives.
- Conduct control diagnostics in a timely manner.
The disease of extrasystole is characterized by relapses, therefore, after completing the course of therapy, you should regularly undergo control diagnostics of the heart rhythm.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.