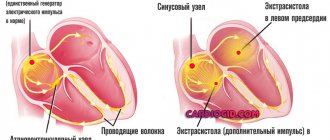
Ventricular extrasystole
Often found in acute myocardial infarction and dyselectrolythemia. Rare extrasystoles can be recorded in 2/3 of healthy people. They are most often not felt or have no clinical significance. Just like atrial, ventricular extrasystoles are divided into functional and organic. Functional extrasystoles are of non-progenic (psychogenic, reflex, dysregulatory, diselectrolyte, dyshormonal) origin. Organic ventricular extrasystoles are recorded in almost all patients in the acute period of myocardial infarction and very often in patients with chronic ischemic heart disease. Other causes of clinically significant extrasystole, including those threatening severe ventricular tachyarrhythmias, are all variants of non-coronarogenic myocardial pathology (myocarditis, all types of cardiomyopathies, severe myocardiostrophies). Ventricular extrasystole is observed in patients with hypertension and complicates the course of acquired and congenital heart defects. The cause of extrasystole can be hemodynamically significant mitral valve prolapse, false chords of the left ventricle (thread-like tendon-muscular formations connecting the apices of the papillary muscles to each other or to the wall of the ventricle, as well as located between different parts of the free ventricle). Ventricular extrasystole follows. It may be associated with digitalis intoxication (in these cases, extrasystole often takes on the character of an allorhythmia). In addition, there may be an arrhythmogenic effect of antiarrhythmic drugs, sympathomimetics, and many other drugs (aminophylline, ephedrine, caffeine, diuretics, glucocorticoids, antidepressants, etc.).
Diagnostics.
There is no atrial P wave before the extrasystolic QRS complex. Ventricular extrasystole occurs under the influence of an impulse emanating from the conduction system of one of the ventricles. The excitation first covers the ventricle in which the extrasystole occurred, and then belatedly spreads to the other ventricle. As a result of this aberrant impulse propagation, the QRS complex widens and becomes deformed. Secondary to the change in depolarization, repolarization also changes - ST–T are discordant with respect to QRS. Extrasystoles emanating from the left ventricle in the chest leads form a blockade of the right leg (since the excitation of the right ventricle is delayed). Accordingly, right ventricular extrasystoles have the morphology of left bundle branch block due to delayed depolarization of the left ventricle. More accurate topical diagnosis of ventricular extrasystoles is quite complex and is based on vector analysis of the extrasystolic complex. If extrasystoles occur closer to the apex of the heart, then the resemblance to a blockade of one of the bundle branches decreases. Septal extrasystoles can form a complex similar to the supraventricular one with a QRS width of less than 0.12 s, and the onset of the QRS is deformed like a delta wave. Identical coupling intervals indicate that there is a single source of their occurrence (monotopic extrasystole). For monotopic ventricular extrasystoles, fluctuations in coupling intervals within 0.08 s are possible. Significant differences in coupling intervals are characteristic of different sources of their formation - bifocal, polyfocal (polytopic) extrasystoles. The shape of ventricular extrasystolic complexes in the same lead can be the same (monomorphic extrasystoles) or different (polymorphic extrasystoles). Polymorphic extrasystoles may indicate the existence of different sources of ectopia. But polymorphism of extrasystoles can also be observed with a single source of their occurrence, which is associated with the peculiarities of the functional state of the ventricular conduction system. If there are significant differences in the coupling intervals and the same shape of the extrasystoles, you should think about parasystole. In some cases, ventricular extrasystoles acquire an ordered character (allorhythmia), in which extrasystoles occur in a certain sequence after excitations of the main rhythm (bi-, tri-, quadrigeminy). Ventricular extrasystoles are characterized by an extended post-extrasystolic interval and a complete compensatory pause. It is possible that ventricular extrasystoles are located between two contractions of sinus rhythm (interpolated extrasystoles). It is possible to note some features of the morphology of ventricular extrasystoles, depending on their genesis. Ventricular extrasystoles in practically healthy people are usually high-amplitude (more than 20 mm), the QRS width does not exceed 0.12 s, the ST segment is discordant to the QRS, the T wave is asymmetrical. Pathological extrasystoles are often low-voltage QRS is jagged and does not resemble the shape of a bundle branch block, ST is closer to the isoline with a symmetrical T wave.
Treatment.
Antiarrhythmic drugs - amiodarone, membrane-stabilizing class IB, Magnerot.
Classification and differences between species, stages
The gradation and danger to health and life during ventricular extrasystole is determined according to the Lown classification. The following classes of PVCs are distinguished:
- 0 – complete absence of ventricular extrasystoles;
- 1 – single contractions caused by an impulse from the same source;
- 2 – the impulse is also monomorphic, but their number is more than 30 per hour;
- 3 – extrasystoles from different foci;
- 4 – divided into two types: A – paired extrasystoles, B – group extrasystoles, which are also called short runs of ventricular tachycardia;
- 5 – PVC, in which the ventricular complex “overlaps” the T wave of the previous cycle. Such extrasystole is the most dangerous and can lead to arrhythmia, which significantly affects hemodynamics, causes shock and death.
Based on the time of occurrence, three types are distinguished:
- early - ventricular contractions occur during the passage of an impulse through the atria;
- interpolated ventricular extrasystoles - simultaneously with contraction of the upper chambers of the heart;
- late - occurring during diastole.
Ordered ventricular extrasystoles are called allorhythmia . When a cardiac arrhythmia (CHD) such as ventricular extrasystole occurs after each normal complex, they speak of bigeminy , when after two normal complexes, they speak of trigeminy and so on.
The use of gradations for the treatment of extrasystole
Indicating the degree of arrhythmia in the formulation of the diagnosis is very important. The treatment tactics chosen by the doctor will depend on this.
Thus, the presence of extrasystoles of the first gradation in a patient indicates the functional nature of the resulting abnormal contractions. About 60-70% of people experience a similar phenomenon, and this is considered the absolute norm. The only thing required is to periodically check the ECG. However, if you have any symptoms of cardiovascular pathologies, you should undergo additional examination, as this may be one of the first signs of the disease.
If the second gradation is detected without hemodynamic disturbances, non-drug treatment is indicated: auto-training, psychotherapy, avoidance of risk factors. If there are accompanying symptoms or the appearance of polymorphic foci is noticed (third gradation), an appropriate course of antiarrhythmic drugs is required.
Finally, the fourth, fifth, as well as third degree refractory to conservative therapy, especially with hemodynamic disorders, require surgical treatment. In this case, surgical interventions such as catheter radiofrequency ablation or pacemaker implantation may be indicated.
This classification is also used to make a forecast. Ventricular extrasystole of grade 3-5 according to Lown is considered threatening. These are the so-called malignant arrhythmias. They are characterized by a high risk of sudden death. In this case, the patient should be transferred to the intensive care unit.
The location of the lesions also matters. The prognosis is less favorable in the presence of left ventricular arrhythmias.
Compensatory pause
You may have noticed that after atrial and ventricular extrasystoles there is usually a pause before the next normal sinus complex. The pause after a ventricular extrasystole is usually (but not always) longer than after an atrial extrasystole. A complete compensatory pause means that the interval between the normal QRS complex immediately before and immediately after the ventricular premature beat is equal to two PR intervals (see Fig. 16-7). A complete compensatory pause is more typical for ventricular than for atrial extrasystoles. Sometimes a ventricular extrasystole occurs almost exactly between two normal contractions. In such cases, they talk about insertion (interpolated) extrasystole.
Treatment of the disease
The treatment of ventricular extrasystole is based on timely treatment of the disease, against the background of which a heart rhythm disturbance develops.
In the case of benign extrasystole, there is usually no organic damage to the myocardium and the course is often asymptomatic. With this variant of the disease, treatment is not prescribed. Antiarrhythmic drugs can be prescribed if the attacks are subjectively poorly tolerated by the patient.
With a potentially malignant course that occurs against the background of some organic pathology of the heart, moderate-frequent or frequent ES occurs. Sometimes “jogs” of ventricular tachycardia occur (group ventricular extrasystoles). In this case, there is a risk of sudden cardiac death. To reduce the likelihood of death and stop the manifestations of the disease, treatment is mandatory.
Malignant extrasystole of ventricular origin implies the presence of life-threatening symptoms in addition to the main manifestations of the disease. These include loss of consciousness and cardiac arrest. Due to the very high risk of cardiac death, complex therapy is prescribed.
- Extrasystole of the heart causes and symptoms treatment
Any frequent, sudden ventricular extrasystole, regardless of its history, is an emergency indication for the administration of antiarrhythmic drugs and hospitalization.
When selecting drugs, an individual approach to determining the dosage and studying all kinds of tests is necessary to exclude contraindications to taking antiarrhythmics. The dose of medicinal substances is gradually increased until a stable effect appears. Abrupt withdrawal of the drug is unacceptable. The adequacy of treatment is assessed using Holter monitoring.
Almost all antiarrhythmic drugs have proarrhythmic side effects - they can cause arrhythmia. To reduce the likelihood of complications, all antiarrhythmics (Etatsizin, Propanorm, Sotalol, Amiodarone) are prescribed with beta blockers (Propranolol, Metoprolol, Bisoprolol). The dosage of the latter should be minimal.
For patients suffering from myocarditis or a history of myocardial infarction, it is advisable to use Amiodarone or Cordarone as antiarrhythmic drugs. Other drugs from this group in this case can provoke arrhythmia. To increase blood circulation and improve the properties of the myocardium in order to prevent ventricular extrasystoles, the following are additionally prescribed:
- antiplatelet agents (Cardiomagnyl, Aspirin);
- ACE inhibitors (Enalapril, Perindopril);
- nitrates with prolonged action (Kardiket, Nitrolong);
- calcium channel blockers (Diltiazem, Verapamil);
- complex vitamins and substances that improve myocardial metabolism (Panangin, Magnevit, Actovegin).
Extrasystole against the background of other heart diseases: the role of classification
It is worth noting that the above prognostic signs are correct only in the absence of concomitant diseases, such as myocarditis, valve defects or coronary heart disease. Often they themselves are the causes of abnormal heart contractions.
Extrasystoles of the 3rd, 4th, 5th gradations can lead to significant hemodynamic disturbances. Cardiac output decreases, blood supply to the coronary vessels and brain deteriorates. All this forms a vicious circle, which contributes to the further progression of IHD. Also, the presence of this pathology is an indication for a significant change in treatment tactics.
In general, the presence of ischemic disease (especially previous myocardial infarction) significantly worsens the prognosis for a patient even with arrhythmias of grade 2-3 according to Lown.
conclusions
Ventricular extrasystole is a common heart disease in which myocardial automatism is disrupted. If individual extraordinary contractions are functional in nature and can be present in healthy people, an increase in frequency and the appearance of several foci indicates an organic type of lesion.
For the purposes of differential diagnosis, prognosis and choice of treatment, a simple and effective Lown classification was proposed, which has been successfully used since 1975 to this day.