A pathological condition in which a person’s heartbeat rhythm is disturbed is called arrhythmia. Arrhythmia is divided into two types - tachycardia (increased rhythm) and bradycardia (slowed rhythm). It is often difficult for a non-specialist to understand from his own feelings how tachycardia and bradycardia differ.
Tachycardia
During attacks of tachycardia, the heart begins to beat faster than 90 beats per minute. If such a condition occurs as a result of physical activity or stress, then it is not considered a pathology and does not require treatment. But if there are signs of tachycardia that appear at rest, you should consult a cardiologist.
Types of tachycardia: sinus (rhythm disturbance of the sinus node in the right atrium), paroxysmal (rhythm disturbance outside the sinus node) and ectopic (differs from paroxysmal in that it develops very slowly).
Pathological tachycardia is caused by the following factors:
- myocardial damage;
- myocarditis,
- cardiac ischemia;
- birth defects;
- cardiomyopathy;
- complications after drug therapy.
Bradycardia - symptoms and treatment
Since both cardiac and extracardiac diseases can lead to bradycardia, diagnosis is aimed at identifying not only heart diseases.
When talking with the patient, the doctor identifies symptoms that may be associated with bradycardia: fainting, presyncope, episodes of dizziness, shortness of breath and weakness on exercise. The doctor also finds out what medications the patient is taking and what diseases he has suffered.
Standard electrocardiography (ECG) at rest will allow you to evaluate the heart rhythm in the short time during which it is recorded. For clinically significant bradycardia, this is sufficient in situations where disorders accompanied by bradycardia (for example, atrioventricular block or decreased sinus node activity) are constantly recorded.
Another important diagnostic method for assessing heart rhythm throughout the day (and with the advent of multi-day recorders, even for several days) is Holter ECG monitoring. Its diagnostic qualities significantly exceed those of a standard ECG. When performing Holter ECG monitoring:
- estimate the average heart rate during the day, day, night;
- detect significant pauses in the heart rhythm, episodes of sinoatrial and atrioventricular blocks, as well as any cardiac arrhythmias that occur while wearing the ECG recorder;
- compare symptoms and episodes of bradycardia and arrhythmias.
The patient keeps a diary in which he indicates his symptoms and the time of their occurrence, and the doctor, looking at the ECG recording made at these moments, evaluates the connection between the described symptoms and the findings on the ECG. It is this approach that makes it possible to identify the so-called “symptomatic bradycardia,” which is one of the most important indications for installing an electrical pacemaker (pacemaker).
If symptoms presumably associated with bradycardia occur 1-2 times a month, then an external loop recorder is used. The principle of operation of the device is that the recorded data is deleted from memory over time, and the final recording is made only at the moment when the device automatically recognizes the presence of an arrhythmia or the patient himself activates the recording when symptoms occur.
A pharmacological test with atropine will allow one to assess the contribution of the autonomic nervous system to the development of bradycardia in a patient [5].
An electrophysiological study (EPS) in the diagnosis of bradycardia is of less importance, since spontaneously occurring episodes of bradycardia are often diagnosed using Holter ECG monitoring.
non-invasive - using a thin probe-electrode inserted into the esophagus through the nose, electrical stimulation of the heart is performed, and then the time for restoration of spontaneous activity of the sinus node is assessed. This method allows you to assess atrioventricular conduction disturbances.
Invasive EPI involves recording the spontaneous electrical activity of the heart in its various parts and electrical stimulation of the heart through electrodes inserted into the chambers of the heart (atria and ventricles). To do this, you have to pierce the femoral artery or vein and pass the electrode to the heart. However, the diagnosis of bradycardia in most cases does not require invasive EPS. The method is used only when non-invasive methods are not informative and to clarify the issue of implantation of a pacemaker.
In cases where there is reason to believe that blockades develop during physical activity, or there is chronotropic insufficiency of the sinus node (heart rate does not increase with exercise), a stress test under ECG control can be used: the patient walks on a moving treadmill, or pedals a bicycle ergometer, and in parallel, an ECG is recorded, blood pressure is recorded and symptoms are assessed.
Echocardiography is usually performed as part of the examination of almost all cardiac patients and allows one to assess the size of the heart cavities, wall thickness, the condition of the valves and myocardial contractility, and to identify a number of diseases that can lead to bradycardia.
Bradycardia
Bradycardia is a condition in which the heart rate slows to 50–30 beats per minute. A slow pulse is considered normal in athletes and young healthy people (if the person does not experience discomfort, dizziness or fainting).
With a reduced heart rate, a person feels dizzy and weak, and cold sweat appears. Due to slow blood flow, organs do not receive enough oxygen. In some cases, fainting may occur.
Bradycardia occurs sinus and with heart block. It develops against the background of the following diseases:
- sclerotic changes in the myocardium;
- meningitis;
- brain tumor;
- hypothyroidism;
- liver damage;
- typhoid fever.
Bradycardia also develops with nicotine, lead poisoning or as a result of drug treatment with glycosides.
Diagnostics
Patients with detected bradycardia are recommended to consult a cardiologist.
An electrocardiographic study for bradycardia allows you to record a rare heart rate, the presence of sinoatrial or atrioventricular block. If, at the time of ECG registration, episodes of bradycardia are not detected, 24-hour ECG monitoring is resorted to.
For the organic form of bradycardia, an ultrasound of the heart is performed. Ultrasound echocardiography determines a decrease in ejection fraction of less than 45%, an increase in heart size, sclerotic and degenerative changes in the myocardium. Using load bicycle ergometry, the increase in heart rate in connection with a given physical load is assessed.
Diagnosis of tachycardia and bradycardia
When visiting a therapist, the doctor will prescribe a number of tests. The main type of diagnosis of arrhythmia is an ECG. There are many ECG signs to identify one or another type of arrhythmia. After the doctor determines what type of arrhythmia is developing in the patient, he will prescribe the optimal treatment.
The Medicenter clinic network employs qualified cardiologists and has modern equipment installed. With us you can undergo a comprehensive examination, establish or confirm your diagnosis and receive treatment recommendations.
Features of heart block
The blockade is associated with a slowdown or cessation of the passage of electrical impulses through the structures of the heart muscle. The root cause may be any myocardial damage, congenital heart disease, atherosclerosis, overdose of certain drugs, dysfunction of the thyroid gland, menopause, etc. The blockade is of the following types:
- depending on the course - transient (passing) or intermittent (arising and disappearing many times during ECG recording), progressive or constant;
- depending on the location - sinoauricular, intraatrial, interatrial, atrioventricular, intraventricular (bundle branch block, conduction disturbance in the myocardium).
Symptoms of heart block, the treatment of which is often necessary, include periodic loss of pulse, fainting, and convulsions.
Symptoms of bradycardia
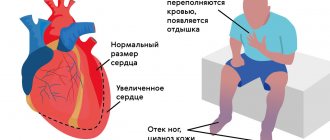
Manifestations of bradycardia are caused by a lack of blood supply to vital organs: the brain, heart and lungs. Bradycardia can manifest itself (Fig. 4):
- decrease in blood pressure;
- presyncope and loss of consciousness;
- dizziness, headache;
- rapid fatigue;
- chest pain;
- shortness of breath and poor tolerance to any physical activity;
- pale skin.
Figure 4. Symptoms of bradycardia. Source: MedPortal
Treatment of bradycardia
It makes sense to treat bradycardia only when there are hemodynamic disturbances associated with it. For example, for excessive weakness and dizziness, ephedrine, caffeine, isadrin, belladonna, eleutherococcus, and so on are prescribed. Moreover, the drugs are prescribed strictly in individual dosages prescribed by the doctor. In case of acute bradycardia, it is necessary to urgently hospitalize the patient and carry out treatment in a hospital under the supervision of a doctor. In particularly difficult cases, cardiac pacing is performed. Moreover, if the sinus node is weak or even only if suspected, any antiarrhythmic drugs are contraindicated. Only after implantation of a permanent pacemaker can antiarrhythmic medications be prescribed. If bradycardia is a complication of another disease, it is first necessary to eliminate the root cause if possible.
Prevention
- Elimination of cardiac pathology.
- Exclusion of extracardiac factors of arrhythmia or blockade (intoxication, autonomic dysfunction, stress, etc.).
- Limit intake of caffeine-containing products and alcohol.
We will help make a diagnosis at an early stage of the development of blockade, tachycardia or other disorders and provide timely treatment for cardiac arrhythmia. Further observation will allow maintaining a good quality of life. For questions regarding the treatment of cardiac arrhythmia in Moscow, please contact us by dialing the number +7.
Diagnosis of bradycardia
Only a doctor can differentiate physiological or pathological bradycardia. To do this, he uses several diagnostic methods.
Auscultation
A simple diagnostic method is to listen to the heart using a phonendoscope. Auscultation of the heart allows not only to determine a rare rhythm, but also to suspect certain diseases of the cardiovascular system.
Electrocardiography
ECG is a method of instrumental diagnostics of the heart, which records not only heart rate, but also helps to diagnose cardiac causes of bradycardia (myocardial ischemia and infarction, sinus node pathology, AV block). This is important for effective therapy. In some cases, daily ECG monitoring is necessary - a Holter study.
Phonocardiography
Phonocardiography (PCG) is a method of hardware diagnostics of sound phenomena that are created during the work of the heart. The study is carried out in conjunction with an ECG. At the same time, the heart sounds that are created during the operation of the valves, as well as additional noise, are assessed.
To diagnose the causes of bradycardia, the doctor may also prescribe:
- EchoCG - ultrasound examination of the heart;
- blood test for markers of damage to the heart muscle (troponins, creatine kinase);
- study of inflammation indicators (C-reactive protein, rheumatic tests, markers of collagenosis);
- blood test for thyroid function indicators (TSH, T4, T3);
- study of blood electrolytes (potassium, magnesium, calcium, sodium);
- biochemical blood test (glucose, bilirubin, cholesterol, creatinine, etc.).
Consequences and complications
In the absence of timely treatment, arrhythmias and heart block provoke attacks of angina, pulmonary edema, and thromboembolism. Acute heart failure and even cardiac arrest are possible. According to statistics, in 10-15% of cases, blockades and other types of arrhythmia lead to death. Pathological tachycardia can provoke myocardial infarction. Complete atrioventricular block or asystole can provoke loss of consciousness, which is associated with a decrease in blood supply to the brain. Every sixth case of thromboembolic complications of atrial fibrillation leads to stroke. For arrhythmias caused by different causes, treatment is selected individually.
Disturbances of atrioventricular and intraventricular conduction
Heart block
- slowing down or interrupting the conduction of an impulse through a certain area of the conduction system of the heart. In some cases, the disorder leads to a lack of bioelectrical activity and cessation of heart function.
Atrioventricular block (AV block)
- disruption of the conduction of impulses from the atria to the ventricles. AV blockades can be congenital or acquired, transient or permanent. The causes of acquired AV blocks and symptoms are in many ways similar to SSSS.
There are three degrees of AV block:
- 1st degree - each impulse is carried out from the atria to the ventricles, but more slowly. As a rule, it is asymptomatic and is detected during electrocardiography or 24-hour ECG monitoring. A diagnostic sign is a prolongation of the PQ interval of more than 200 ms on the ECG;
- 2nd degree - the conduction of impulses from the atria to the ventricles is periodically interrupted. Divided into types 1 and 2. Symptoms may occur: episodes of weakness, darkening of the eyes, dizziness. In cases of advanced AV block of the 2nd stage, when several impulses in a row do not reach the ventricles, fainting may occur. ECG sign - periodic loss of the ventricular QRS complex;
- 3rd degree - complete absence of conduction of impulses from the atria to the ventricles. In this situation, the atria and ventricles contract each in its own rhythm. On the ECG, P waves and ventricular QRS complexes are not related to each other; the frequency of the atrial rhythm is more frequent than the ventricular one. Depending on the level of blockade, proximal and distal types can be distinguished. Proximal type AV block at the level of the AV node and His bundle is characterized by a high frequency of escape rhythm (usually up to 40 per minute) with narrow or slightly widened QRS. Distal AV block at the level of the His bundle branches is always characterized by widened QRS complexes with a frequency of less than 40-35 per minute. Complete AV block leads to disruption of the blood supply to vital organs, the development of heart failure, and an increased risk of sudden cardiac arrest.
In case of first degree AV block, asymptomatic 2nd degree AV block of type 1, a wait-and-see approach is used with regular diagnostics and treatment of the underlying disease. For AV block of the 3rd degree, 2nd degree of the 2nd type, symptomatic AV block, the main method of treatment is the installation of a pacemaker.
Causes of bradycardia
There are two groups of reasons: factors not related to heart disease (extracardiac) and factors directly related to pathologies of the cardiovascular system (cardiac).
Extracardiac factors
- persistent lack of thyroid hormones (hypothyroidism);
- stomach and duodenal ulcers;
- cerebral hemorrhage;
- head injuries (bruises and swelling);
- rheumatic fever and other systemic connective tissue diseases;
- toxoplasmosis, diphtheria and other infectious diseases;
- prolonged abstinence from food;
- neurocircular dystonia;
- neuroses accompanied by autonomic dysfunction;
- general hypothermia;
- lead poisoning, nicotine;
- reduced body temperature.
Cardiac causes
- myocarditis (inflammation of the myocardium);
- congenital anomalies of the cardiac conduction system;
- cardiosclerosis;
- myocardial dystrophy;
- IBS.
Separately, bradycardia caused by taking medications is distinguished:
- beta blockers;
- cardiac glycosides;
- antiarrhythmic drugs;
- ivabradine.