The term “chronic cor pulmonale” refers to changes in the heart muscle caused by lung diseases. This excludes cases of pathology complicating diseases of the heart and large vessels (mitral stenosis, cardiosclerosis after a heart attack, congenital defects, dilated cardiomyopathy).
In diagnosis, an indispensable condition must be a primary violation of the structure of the lung tissue and its functions. The prevalence of the recorded pathology among the adult population allows us to place it in third place after ischemic and hypertension diseases.
In the International Classification of Diseases (ICD-10), types of chronic pulmonary heart disease are included in the general class of cardiovascular diseases. Codes I26, I27, I28 differ in etiological factors. All cases are united by the gradual formation of overload of the right side of the heart due to the development of high blood pressure in the pulmonary circulation.
Causes
Depending on the causes, the WHO Expert Committee has developed a classification of chronic pulmonary heart disease. Diseases are divided into 3 groups:
- group 1 - diseases associated with impaired passage of air through the alveoli, these can be mechanical obstacles (bronchial asthma), inflammatory lesions (tuberculosis, chronic bronchitis, bronchiectasis, pneumoconiosis), replacement of lung tissue with fibrous tissue (systemic lupus erythematosus, sarcoidosis, eosinophilic infiltration ), a total of 21 nosologies are included;
- group 2 - diseases that impair ventilation of the lungs by affecting the auxiliary mechanisms of breathing (skeletal skeleton of the chest, ribs, muscles), this includes curvature of the spine, adhesions in the pleural cavity, chronic diseases associated with impaired neuromuscular conduction (poliomyelitis) , artificial hypoventilation after surgical interventions on the chest organs;
- group 3 - vascular lesions of the lungs (arteritis, thrombosis and embolism, compression of the main vessels by a tumor, aortic aneurysm and others).
All risk factors for underlying disease accelerate and negatively affect the heart.
Causes of cardiopulmonary failure
Cardiopulmonary failure never occurs without a reason. As a rule, several reasons lead to its development. There are three main groups of causes that can provoke pathology:
1. Bronchopulmonary diseases. According to statistics, they act as a provoking factor in more than 70% of all cases. Among the most common diseases are bronchial asthma, pulmonary tuberculosis, chronic bronchitis and other severe disorders of the respiratory system (for example, cystic fibrosis).
2. Thoradiaphragmatic diseases. They are directly related to pronounced deformation of the chest and limited mobility of the diaphragm. The appearance is caused by severe curvatures of the spinal column (in particular, kyphoscoliosis), ankylosing spondylitis, and restrictions on the expansion of the lungs (pleuritis).
3. Vascular diseases. This group includes diseases that affect lesions of the pulmonary bed. These include sickle cell anemia, pulmonary vasculitis, compression of the pulmonary veins and arteries by neoplasms.
4. Vascular diseases. Often, the development of cardiopulmonary failure is provoked by aneurysms, atherosclerosis and blood clots in the arteries of the lungs.
What happens in the body
In patients of groups 1 and 2, all changes develop due to spasm of small arterioles in the lung tissue as a reaction to insufficient oxygen supply. In group 3, in addition to spasm, there is a narrowing or blockage of the vascular bed. The pathogenesis of the disease is associated with the following mechanisms.
- Alveolar hypoxia (lack of oxygen in the alveoli) - scientists associate vascular spasm in response to hypoxia with disturbances in sympathoadrenal regulation. There is a contraction of vascular muscles, an increase in angiotensin-converting enzyme (ACE), calcium in the blood, and a decrease in relaxation factors of the pulmonary vessels.
- Hypercapnia - an increase in the concentration of carbon dioxide in the blood does not directly affect the vascular wall, but through acidification of the environment and a decrease in the sensitivity of the respiratory center of the brain. This mechanism enhances the production of aldosterone (adrenal hormone), which retains water and sodium ions.
- Changes in the vascular bed of the lungs - compression and emptying of capillaries due to developing fibrous tissue is important. Thickening of the muscular walls of the pulmonary vessels contributes to the narrowing of the lumen and the development of local thrombosis.
- An important role is played by the development of anastomoses (connections) between the bronchial arteries, belonging to the systemic circulation, and the pulmonary vessels.
- The pressure in the systemic circle is higher than in the lungs, so the redistribution goes towards the pulmonary vascular bed, which further increases the pressure in it.
- In response to hypoxia, blood cells that carry hemoglobin and erythrocytes change. Their number increases simultaneously with platelets. Favorable conditions for thrombus formation are created and blood viscosity increases.
All taken together leads to increased load on the right ventricle, hypertrophy, and then failure of the right heart. An enlarged right atrioventricular orifice contributes to insufficient closure of the tricuspid valve.
Clinical course
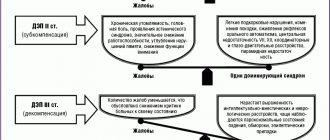
Soviet pulmonologists B. Votchal and N. Palev proposed a clinical description of the stages of development of the pulmonary heart:
- in the initial (preclinical) stage - there are no symptoms of hypertension in the pulmonary circulation, hypertension is possible temporarily with an exacerbation of pulmonary disease;
- in the second stage - there is right ventricular hypertrophy, but all signs are compensated; instrumental examination reveals stable pulmonary hypertension;
- third stage - accompanied by decompensation (pulmonary heart failure), there are symptoms of right ventricular overload.
Diagnosis of pathology
The diagnosis of cardiopulmonary failure is established based on the results of a comprehensive examination. During the initial examination, the doctor collects anamnesis (listens about symptoms, chronic pathologies in the patient and immediate family), performs a visual examination (possible swelling of the feet and legs), conducts a physical examination and standard measures (measuring blood pressure, listening to breathing using a phonendoscope). Upon palpation, a cardiac impulse is detected, and upon percussion, an expansion of the boundaries of the region of the muscular organ, which is partially covered by the lungs, is detected.
Among the laboratory diagnostic methods for making a diagnosis, an analysis of the gas composition of arterial blood is required. If there are problems, patients experience a decrease in P02 and SAO2 P02, and an increase in PC02. Additionally, a general blood test is prescribed to detect an infectious process in the body (by increasing the level of leukocytes). The most informative ways to detect cardiopulmonary failure are instrumental diagnostic methods. Depending on the symptoms, the patient may be prescribed:
- study of respiratory function (external respiration function). With the help of this examination, it is possible to establish the nature and severity of pulmonary ventilation impairment;
- electrocardiography (ECG). This is an accessible method that does not require additional preparation from the patient. The essence of electrocardiography is to record the electrical potentials of a muscle organ, which makes it possible to detect changes in rhythm and electrolyte deficiency. If the disease occurs in an acute form, it is possible to detect signs of overload in the right parts of the muscular organ. If the disease is chronic, it is possible to detect markers (both direct and indirect) of right ventricular hypertrophy;
- echocardiography (EchoCG). It is often prescribed in addition to an ECG, since the information content of this examination regarding cardiopulmonary failure is very high. This is the main non-invasive method with which it is possible to assess intracardiac hemodynamics, determine the size of the cavities of the muscular organ and the degree of pulmonary hypertension. EchoCG allows you to detect a number of possible disturbances in the functioning of the heart, differentiate it from heart disease and other pathologies;
- chest x-ray. This is a simple technique with which it is possible to assess the condition of the respiratory system (detect damage to the internal organ and notice signs of pulmonary hypertension);
- transbronchial lung biopsy. These methods are rarely resorted to, in particularly advanced clinical cases. A puncture biopsy of the lung is performed under ultrasound or X-ray guidance using a local anesthetic.
Clinical manifestations
At the early stage of the disease, the manifestations of chronic pulmonary heart disease do not differ from the typical symptoms of major pulmonary diseases. They intensify with exacerbation and are treatable.
Shortness of breath is a consequence of oxygen deficiency, but it also accompanies inflammation of the lung tissue, emphysema. The intensity does not always correspond to the degree of hypoxia.
Changes in the phalanges occur due to impaired nutrition of the periosteum
Tachycardia is a nonspecific symptom; the heart rate increases in various diseases that are associated with an activated sympathetic nervous system and increased release of adrenaline.
Chest pain is not similar to angina. They are believed to be caused by insufficiency of the coronary vessels, which have to feed the thickened muscle of the right ventricle. Spasm of the arteries of the heart and intoxication of the myocardium with inflammatory products are also important.
Increased fatigue and weakness occur when the shock capacity of the heart decreases. Peripheral tissues of various organs, including the brain, lack blood supply.
Heaviness in the legs, swelling - in addition to myocardial weakness, an increase in the permeability of the vascular wall plays a role. Swelling occurs on the feet and legs. They intensify in the evening and subside during the night. In the third stage, they spread to the thighs.
The feeling of heaviness and pain in the right hypochondrium is caused by an enlarged liver and stretching of its capsule. In a severe form of the disease, ascites simultaneously appears and the abdomen “grows” rapidly. This symptom is more pronounced in elderly patients with concomitant atherosclerosis of the abdominal arteries.
A cough with a small amount of sputum is more associated with the underlying pathology of the lungs.
Manifestations of encephalopathy - chronic lack of oxygen and excess carbon dioxide cause pathological disorders in the brain, disrupt vascular permeability, and promote edema. Patients have 2 possible symptoms:
- increased excitability, aggressive behavior, euphoria, development of psychosis;
- lethargy, lethargy, indifference, drowsiness during the day, insomnia at night.
In severe cases, seizures occur with loss of consciousness or dizziness, cold sweat and decreased blood pressure.
Publications in the media
Acute cor pulmonale (ACP) is a clinical syndrome of acute right ventricular failure caused by sudden pulmonary hypertension due to pulmonary vascular obstruction. A classic example is TELA. Acute cor pulmonale develops over minutes, hours or days.
Etiology • PE • Embolism of fat, gas, tumor • Pulmonary vein thrombosis • Valvular pneumothorax, pneumomediastinum • Pulmonary infarction • Lobar or total pneumonia • Severe attack of bronchial asthma, status asthmaticus • Cancerous lymphangitis of the lungs • Hypoventilation of central and peripheral origin (botulism, poliomyelitis, myasthenia gravis) • Arteritis of the pulmonary artery • Resection of the lung • Massive atelectasis of the lung • Multiple fractures of the ribs, fracture of the sternum (floating chest) • Rapid accumulation of fluid in the pleural cavity (hemothorax, exudative pleurisy, massive infusion of fluid through a subclavian catheter mistakenly inserted into the pleural cavity ).
Risk factors • Thrombophlebitis of the deep veins of the lower extremities • Postoperative or postpartum period • Bronchopulmonary pathology.
Pathogenesis • Acute development of pulmonary hypertension (with massive pulmonary embolism, the right ventricle loses completely or reduces the ability to pump blood into the pulmonary circulation, and therefore acute right ventricular failure develops) • Severe bronchoconstriction • Development of pulmonary-cardiac, pulmonary-vascular and pulmonary-pulmonary coronary reflexes - a sharp decrease in blood pressure, deterioration of coronary blood flow • Acute respiratory failure • See also Secondary pulmonary hypertension.
Clinical manifestations are a sudden deterioration in the patient’s condition within a few minutes or hours (less often days) against the background of complete well-being or a stable course of the underlying disease. Sometimes it develops at lightning speed.
• Severe shortness of breath, feeling of suffocation, fear of death, severe cyanosis, acrocyanosis.
• Pain syndrome: chest pain, with pulmonary embolism - pain in the side associated with breathing (often in combination with hemoptysis). Sharp pain in the right hypochondrium may appear due to an enlarged liver with the rapid development of right ventricular failure.
• Swelling of the neck veins also due to the development of acute right ventricular failure.
• Decrease in blood pressure down to a collaptoid state and tachycardia 100–160 per minute due to decreased cardiac output.
• Auscultation of the lungs - signs of the pathological process that caused ALS: weakening, absence of respiratory sounds or bronchial breathing, dry and/or moist rales, pleural friction noise.
• Auscultation of the heart - accent of the second tone over the pulmonary artery, increased cardiac impulse, often arrhythmia (atrial and ventricular extrasystole, atrial fibrillation), sometimes systolic murmur of tricuspid valve insufficiency, gallop rhythm.
• Sometimes there is a discrepancy between the severity of the patient’s condition and the normal results of percussion and auscultation of the lungs.
Laboratory data • Hypoxia (decreased paO2) • Hyperventilation (determined by a drop in paCO2) • Moderate acute respiratory alkalosis (low paCO2 and elevated pH values).
Special studies
• X-ray examination of the chest cavity •• Signs of pneumothorax, the presence of fluid in the pleural cavity, total pneumonia, atelectasis •• Even with massive embolism, X-ray changes in the lungs may be absent •• Angiography of the pulmonary vessels - determining the localization of a blood clot if emergency embolectomy is necessary.
• ECG (especially informative in dynamics) •• Signs of ALS can be mistaken for MI of the posteroinferior wall of the left ventricle ••• Wide and deep Q wave and negative T wave in standard leads II, III, aVF, V1–V2, increased amplitude of the R wave in leads V1–3, ST segment depression in standard and chest leads ••• Signs of overload or hypertrophy of the right heart: deviation of the EOS to the right, deep S wave in standard lead I, V5–V6, high R in aVR, shift of the transition zone to the left , P pulmonale, partial or complete blockade of the right branch of the His bundle •• Rhythm disturbances (extrasystoles, atrial fibrillation).
Differential diagnosis is acute right ventricular failure in right ventricular myocardial infarction.
TREATMENT etiological; symptomatic is aimed at correcting hypoxia and acidosis, controlling hypervolemia and correcting right ventricular failure.
• Oxygen therapy. The initial stages of treatment for ALS should include the use of oxygen and improving the ventilation ability of the patient's lungs by correcting the underlying pulmonary disease. Since many patients are sensitive to oxygen, it is necessary to avoid the use of high concentrations and maintain saturation at 90%.
• Diuresis. Fluid retention is common and may impair pulmonary gas exchange and increase pulmonary vascular resistance. Improving oxygenation and limiting salt may be sufficient, but diuretics are often necessary.
• Phlebotomy provides a short-term effect and may be useful when Ht levels are above 55–60%.
• Cardiac glycosides do not have a good effect in the absence of left ventricular failure.
• Vasodilators are widely used, especially in cases mediated by occlusive vascular lesions or pulmonary fibrosis. However, the effectiveness of the drugs is questioned.
Abbreviation • ALC—acute cor pulmonale.
ICD-10 • I26.0 Pulmonary embolism with mention of acute cor pulmonale
Diagnostics
In people with chronic cor pulmonale, the diagnosis can be suspected by their appearance: in the compensation stage, dilated skin vessels appear in the cheek area (blush) and on the conjunctiva (“rabbit eyes”). Cyanosis is found on the lips, tip of the tongue, nose, and ears.
When examining the fingers, changes in the nail phalanges are visible: they become flat and widened (“drumsticks”). Unlike heart failure, the arms and legs remain warm to the touch.
Swollen veins in the neck indicate the formation of stagnation at the level of the veins of the systemic circulation, more pronounced at the height of inspiration
When auscultating the heart, the doctor hears:
- characteristic changes in tones above the pulmonary artery;
- in the stage of decompensation - a murmur indicating insufficiency of the right atrioventricular valve;
- a lot of different types of wheezing in the lungs against the background of altered breathing.
The x-ray reveals a typical bulging of the contours of the pulmonary artery, an enhanced tissue pattern, and an expansion of the zone of lymphatic vessels. This indicates an increase in pressure in the pulmonary circle. In the decompensation stage, the heart shadow expands to the right.
Echocardiography assesses the strength of the right ventricle, the degree of dilatation, and overload. Due to increased pressure, the wall of the interventricular septum bends to the left.
Respiratory functions are measured with special devices, and the spirogram is deciphered by a doctor in the functional diagnostics office.
The study of pressure in the pulmonary artery is carried out in complex diagnostic cases. A reliable sign of hypertension in the pulmonary circle is considered to be a resting pressure of 25 mm Hg. Art. and higher, and with load - over 35.
First aid for pulmonary edema
Unlike the chronic form, the acute form of the pathology requires immediate assistance during an attack. A person is not able to help himself, so he needs help from the outside. First of all, you should call an emergency team. While waiting for her, the person should be seated on a chair and given a Nitroglycerin tablet. If the attack occurs indoors, be sure to open all windows to provide fresh air flow.
If a person gets worse, cardiopulmonary resuscitation methods are required. To do this, rhythmically press on the chest area or do 30 presses and mouth-to-mouth breathing (alternating these actions). The main goals of these measures are to normalize blood circulation and restore respiratory function. If you lack the skills, you can simply massage the sternum.
Functional classes
During the examination, it is necessary to establish the functional class of manifestations of cor pulmonale.
- Class 1 - the main symptoms are diseases of the bronchi and lungs, hypertension in the pulmonary circle is detected only with instrumental examination and stress tests;
- Class 2 - in addition to the listed symptoms, there is respiratory failure due to narrowing of the bronchi;
- Class 3 - respiratory failure is severe, followed by cardiac failure. Constant shortness of breath, tachycardia, dilatation of the neck veins, cyanosis. Studies reveal persistent hypertension in the pulmonary circulation;
- Class 4 - decompensation, all clinical manifestations are pronounced, there are congestion, respiratory and heart failure of the third degree.
Doppler examination allows you to quantify the pressure in the pulmonary artery, measure the reverse flow of blood (regurgitation) from the right ventricle into the atrium
Treatment
Treatment of chronic pulmonary heart disease should begin with the prevention of exacerbations of respiratory diseases, especially colds and flu, with the timely use of antiviral and antibacterial treatment.
Mode Changes
Patients are advised to limit physical activity. Do not visit mountainous areas, since in high altitude conditions even a healthy person experiences oxygen deficiency. And in patients with pulmonary diseases, a reflex vascular spasm occurs and the degree of tissue hypoxia deepens.
Women should be aware of the negative effects of birth control pills.
It is necessary to stop smoking and even staying in a smoky room.
Directions of therapy
All treatment methods are aimed at eliminating or weakening the existing mechanisms of pathology, these include:
- treatment of the underlying pulmonary disease and compensation of lost respiratory function;
- decreased vascular resistance in the pulmonary circulation and unloading of the right ventricle;
- restoration of normal blood composition, antithrombotic therapy.
Oxygen treatment
Oxygen is supplied in a humidified form through a mask, cannulas in the nasal passages, and some clinics use oxygen tents with special air saturation conditions. For a therapeutic effect on chronic pulmonary heart disease, the oxygen level in the inhaled air must be at least 60%.
Therapy is carried out for an hour up to 5 times a day and more often.
Oxygen supply can reduce all symptoms of the disease caused by hypoxia
How to lower pulmonary artery pressure
To reduce pressure in the pulmonary artery, medications of different groups are used:
- calcium antagonists (possible swelling and redness of the face, headache, feeling of heat, decreased blood pressure);
- α-adrenergic blockers - dilate blood vessels, reduce the ability of platelets to stick together (the side effects are the same, increased irritability and weakness are possible);
- inhaled nitric oxide (has no side effects);
- diuretics - medications with a diuretic effect unload the general bloodstream, facilitate the work of the heart (control of the potassium content in the blood is required);
- group of prostaglandins - selectively act on small blood vessels (side effects such as nasal congestion, increased cough, increased blood pressure, headache).
The drugs Heparin and Pentoxifylline are necessary to improve blood flow and antithrombotic action.
In case of severe heart failure, cardiac glycosides are prescribed very carefully.
Patients with symptoms of decompensation are treated in a hospital. Observation and clinical examination are carried out by a local therapist and pulmonologist.
Forecast
The mortality rate of patients from chronic pulmonary heart disease remains high: 45% of patients survive in the decompensation stage for about two years. Even with intensive therapy, their life expectancy is no more than four years. Lung transplantation gives 60% of patients survival over the next two years.
The disease is very difficult to treat. Any person has the opportunity to rid himself of bad habits and take care of his health in a timely manner. The appearance of cough, shortness of breath and other symptoms requires immediate medical attention.
Disease prevention
In order to prevent pathology, all risk factors that can provoke it should be eliminated. If any negative symptoms appear, it is important to consult a doctor in order to promptly diagnose and treat lung or heart disease. Also, experts recommend leading a healthy lifestyle (not smoking or drinking alcohol), engaging in moderate physical activity and eating right. The diet should be balanced with a predominance of fresh vegetables and fruits.
In order to prevent the development of acute cor pulmonale, patients diagnosed with varicose veins and atrial fibrillation are prescribed indirect anticoagulants. If there are blood clots in the veins, a vena cava filter is often installed. It is a small device that is installed into the lumen of the inferior vena cava. With its help, detached blood clots do not enter parts of the heart muscle and the pulmonary artery system.