Complexes with this research
Pregnancy planning.
Clinical indicators 6,630 ₽ Composition Examination during pregnancy. 3rd trimester 9,620 ₽ Composition
For those at risk of COVID-19 Diagnosis of diseases that complicate the course of coronavirus infection 4,510 ₽ Composition
IN OTHER COMPLEXES
- Coagulogram RUB 2,020
- Men's check-up No. 1 RUB 18,570
- Women's check-up No. 1 RUB 19,290
- Risk of severe COVID-19 RUB 1,090
- Preventative check-up RUB 11,960
Why do you need to know the INR?
INR analysis is a common research method during the diagnosis of cardiovascular diseases. In addition, bleeding and severe thrombus formation are direct indications for studying all parameters affecting coagulation.
Knowing the INR is very important for the cardiologist who prescribed anticoagulants to the patient, since this allows him to control the correctness of the dose calculation, in order not to harm the patient. This also includes taking warfarin, the dosage of which is determined for each patient individually.
In case of cirrhosis of the liver or other disease of the filtering organ, it is also important to know the INR level, because it is the liver that produces many factors that clot the blood.
A separate group of patients are pregnant women. First of all, this is due to the fact that the entire body system begins to work differently during pregnancy. The level of hormones and enzymes changes, and the volume of blood circulating through a woman’s veins increases. Hence the need to control the functioning of the hematopoietic system. Due to the high level of blood clot formation, the likelihood of complications is high. And if the blood is too thin and there is a lack of platelets, there is a high probability of dangerous bleeding during childbirth.
At the very beginning of labor, each woman in labor is given a catheter in a vein, into which, if necessary, an IV will be placed with a composition that increases the level of blood clotting to prevent large blood losses.
Detailed description of the study
Normal blood clotting is possible by maintaining a balance between the processes of blood clot formation and mechanisms that prevent excessive blood clotting.
Prothrombin is a protein that is produced in the liver and plays an important role in blood clotting. Under its action, blood clots form in case of damage to the vascular wall, and bleeding stops.
Prothrombin time (PTT) is the time in seconds it takes for a blood clot, or thrombus, to form.
Prothrombin index (PTI) is a value equal to the ratio of the PTI of the control sample to the PTI of the test sample, expressed as a percentage. The indicator is also used in conjunction with other tests included in the coagulogram to assess the risk of thrombosis or bleeding.
INR (international normalized ratio) is a calculated value characterizing the ratio of prothrombin time and prothrombin index. This indicator is used to monitor treatment with indirect anticoagulants. These drugs reduce the body's ability to form blood clots by blocking the formation of clotting factors. Patients taking anticoagulants should regularly monitor this indicator to prevent complications of anticoagulant therapy. The frequency of INR testing is determined by the attending physician.
Cardiovascular diseases, liver pathology, diabetes mellitus and some other conditions contribute to an imbalance between the blood coagulation and anticoagulation systems. During pregnancy, there is also some change in PTT, PTI and INR. It is caused by changes in hormonal regulation and related factors and usually refers to physiological conditions.
An increase in PTT may be associated with bleeding, and its reduction increases the risk of thrombosis. To prevent complications associated with thrombosis, drugs are prescribed that reduce the likelihood of vascular clot formation - anticoagulants. At the same time, these medications, if the dose is incorrectly selected, increase the risk of bleeding, which requires specialist supervision.
The results of the analysis reflect the value of all three indicators. Assessment of PTT, PTI and INR will help the doctor assess the state of the blood coagulation system and select treatment.
INR norm
Units are used to express INR. The higher the INR, the less blood contains prothrombin and other factors that affect coagulation. The INR of a healthy person ranges from 0.85 units. up to 1.37 units. At the same time, the patient’s age affects the values of the norms:
- Newborns and children of the first year of life – from 0.9 units. up to 1.25 units
- Children from one to six years old can normally have 0.95-1.1 units.
- In patients aged 12-16 years, the normal INR ranges from one to 1.35 units.
- After 16 years, the value should be within 0.85 units. – 1.3 units.
For those who have already been prescribed anticoagulant therapy, the INR should be between 2.0 units. up to 3.0 units, because drugs that fight the formation of blood clots do not allow the blood to thicken, which also affects the prothrombin index.
If a patient is not taking blood thinning medications, but his INR is higher than normal, this may indicate:
- liver diseases;
- coagulopathies;
- prothrombin deficiency;
- lack of fibrogen;
- vitamin K deficiency;
- taking certain medications that affect blood composition;
A low INR always indicates that a person is at risk. Value below 0.5 units. reports the onset of venous thrombosis.
Technique and frequency of analysis
The INR level is determined in blood from a peripheral vein. The sampling is done with a disposable, sterile syringe. Before the injection, the skin is treated with an antiseptic solution. A tourniquet is applied to the forearm, and the nurse carefully draws blood into a syringe. Next, the blood is sent to the laboratory for analysis.
For patients taking anticoagulants or antiplatelet agents, the test is done once every two to three weeks. The frequency is selected individually, depending on the severity of the disease and its duration. Patients with a well-chosen treatment regimen can undergo analysis once a month.
Diet while taking warfarin. Vitamin K content
Warfarin is absorbed in the stomach and jejunum, so changes in the intestinal microflora that produce vitamin K may affect the effect of the drug. The activity of warfarin can also be affected by the food the patient eats. The diet when taking warfarin should take into account those foods that contain large amounts of vitamin K, which can weaken the effect of warfarin, and the lack of vitamin K in the diet can enhance the effect of the drug. Therefore, if you are prescribed warfarin, try to eat a balanced diet and try not to change your diet dramatically so as not to change the amount of vitamin K you get from food.
| Vitamin K content in foods (µg/100 g) | |
| Beef liver | 93 |
| Cheese | 35 |
| Butter | 30 |
| Egg | 11 |
| Soybean oil | 193 |
| Broccoli | 175 |
| Cabbage | 125 |
| Salad | 129 |
| Watercress | 200 |
| Head lettuce | 120 |
| Spinach | 415 |
| Cauliflower | 80 |
| Green tomatoes | 80 |
| Beans | 45 |
| Cucumbers, zucchini | 30 |
| Potato | 16 |
| Green tea | 712 |
| Note: daily requirement of vitamin K is 0.03-1.5 mcg/kg/day (up to 105 mcg/day) | |
Warfarin and alcohol
Alcohol is not recommended during warfarin treatment.
You can indulge in a glass of wine once or twice a week. Exceeding this norm may lead to increased effects of the drug and, as a result, possible bleeding. Illnesses that affect appetite and digestion (vomiting, diarrhea) can also reduce or increase the effect of warfarin, so tell your doctor about any changes in how you feel.
Be sure to tell us about all the medications you are taking or have taken shortly before starting warfarin treatment, as well as new prescriptions if you are already taking warfarin therapy. Many drugs can increase or decrease the effect of warfarin on blood clotting. Keep all prescriptions and write down the names of medications you take. The table shows the most commonly prescribed drugs that can affect the effectiveness of warfarin.
How to take medications correctly
Indications for the purpose of the study
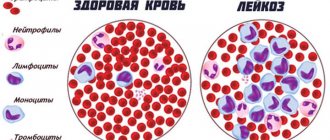
Coagulogram (hemostasiogram) is a comprehensive hematological study aimed at assessing the state of the hemostasis system (blood clotting), or blood clotting indicators. The hemostasis system includes blood cells (platelets) and specific substances (clotting factors) dissolved in blood plasma and contained in platelets. When the integrity of the vessel wall is violated, the coagulation system is activated and a blood clot is formed, preventing blood loss.
Some time after the bleeding stops, fibrinolysis begins - the process of dissolving the blood clot after restoring the damaged vessel wall to resume blood flow.
Indications for a coagulogram are conditions accompanied by increased bleeding or, conversely, increased thrombus formation.
Increased bleeding leads to hemorrhagic syndrome. It is manifested by the formation of hematomas, pinpoint hemorrhages under the skin (petechiae), bleeding of the mucous membranes (nosebleeds, bleeding from the gums), the appearance of blood in the stool, urine, prolonged menstrual bleeding, as well as possible hemorrhages in the internal organs and body cavities. The most dangerous manifestation of hemorrhagic syndrome is hemorrhage in the brain - hemorrhagic stroke, which can lead to rapid impairment of brain function, including death. A hereditary disease associated with blood clotting disorders (decreased or absent clotting factors) is called hemophilia.
The opposite situation - thrombosis - is the formation of blood clots (thrombi) inside blood vessels, preventing the free flow of blood.
People with obesity, diabetes mellitus, heart rhythm disturbances (the most significant of which are atrial fibrillation and flutter), low physical activity, and patients after major operations (for example, joint replacement, heart valve replacement, emergency operations, etc.) are at risk of increased thrombosis. , with varicose veins, previous myocardial infarctions, strokes, and various autoimmune diseases.
Thrombosis in a certain area of the vascular bed is accompanied by an acute or gradual disruption of the blood supply to any organ with disruption of its functions and subsequent tissue necrosis.
In addition to the above conditions, a coagulogram is performed before operations to assess the risk of bleeding, when prescribing certain medications, and also necessarily in case of liver diseases, since most of the proteins of the blood coagulation system are synthesized in this organ.
Methods for diagnosing the state of the blood coagulation system
The main way to check the condition of the bloodstream is a coagulogram. One of its most significant indicators is the level of prothrombin, or coagulation factor II. It is produced in the liver under the influence of vitamin K.
The level of prothrombin in the blood cannot be calculated directly. Its amount is calculated indirectly through the following coagulogram indicators:
- prothrombin time;
- prothrombin index;
- prothrombin level according to Quick;
- INR.
The prothrombin index and INR are most widely used in modern medicine, as they are the most informative.
When is the test prescribed?
Determining the INR level, like any other analysis, has strict indications for its use. Only a doctor can write a referral. The need to take a blood test for INR arises in the following situations:
- before surgery to carry out the necessary preoperative preparation (the norm is from 0.85 to 1.25);
- when taking anticoagulants and antiplatelet agents (the norm is from 2 to 3);
- in the treatment of pulmonary embolism (norm - from 2 to 3);
- for the purpose of preventing thrombosis in heart defects (the norm is from 2 to 3);
- patients after aortic or mitral valve replacement (the norm is from 2 to 3);
- prevention of thrombus formation in deep veins after surgery (the norm is from 2 to 3).
Principles of preparation
Preparing for a blood test for INR is not much different from that for other blood tests.
Blood sampling must be done in the morning, on an empty stomach. Before diagnosis, refrain from eating any food for at least 8 hours. You can only drink regular water without gas. But you should not extend your fast for more than 14 hours. This can cause a deterioration in general health, even to the point of fainting.
Avoid alcohol at least one day before the examination. It is also advisable to limit the intake of fatty and heavy foods at this time. If the patient smokes, an hour before the examination it is necessary to stop smoking.
If the patient is taking any medications, he should consult a doctor. He will explain whether it is worth conducting the study at all or whether it is necessary to stop the drug for a while.
If a blood test for INR is performed to diagnose a coagulation pathology, it should be performed before starting drug therapy. Taking medications may distort the results of the examination.
Immediately before the analysis, if the nurse sees the patient’s anxiety, she should tell him in detail about the examination and reassure him.
Who do doctors prescribe “indirect” anticoagulants (warfarin)?
Patients who need treatment and prevention of thrombosis and embolism of blood vessels, including: – heart rhythm disturbances (atrial fibrillation); – heart valve diseases;
– presence of prosthetic heart valves or blood vessels, incl. in combination with aspirin (acetylsalicylic acid); – acute venous thrombosis (phlebothrombosis) and pulmonary embolism (in combination with heparin); – recurrent venous thrombosis; – repeated pulmonary embolism; – thrombosis of peripheral, coronary and cerebral arteries; – postoperative thrombosis; – myocardial infarction, complicated by the development of an aneurysm and intracardiac thrombus; – during surgical or thrombolytic treatment of thrombosis; – when performing electrical cardioversion of atrial fibrillation (as an additional therapy); – congenital diseases accompanied by pathological thrombosis (thrombophilia).
Do I need to prepare for an INR test?
First of all, you need to remember that blood to determine the INR value is taken from a vein. A prerequisite is on an empty stomach. This means that you cannot eat or drink sugary water 6-8 hours before. At the same time, you should not fast for more than 10 hours before donating blood, as this will distort the data.
The day before the test, you do not need to do heavy physical work. If the patient jogs in the morning every day, before going to the laboratory, you will have to abandon the activity and reschedule it for the evening. Since jogging will affect the speed of blood flow, blood oxygen saturation and its composition.
Any daily medication intake should also be taken into account - the evening dose on the eve of sampling should be taken no later than 17:00. And triple the appointment must be rescheduled, and you need to take the medicine/get an injection after donating blood.
It is recommended to approach the building of the medical institution 15 minutes before the appointed time in order to have time to put your outerwear in the cloakroom, take your time, find an office and calm down before the procedure. Even slight anxiety associated with the fear of being late can affect the composition of the blood.
We must not forget that taking oral contraceptives significantly distorts the actual state of the coagulation systems due to the elements included in the composition that prevent the formation of blood clots. Therefore, an INR test should be scheduled on the fourth day after completing a three-week course of birth control pills. In other words, the test can be taken closer to the end of the week during which withdrawal bleeding occurs. If this is difficult, you must tell the laboratory assistant the name of the drug you are taking so that he takes its effect into account when calculating the result.