Heart examination
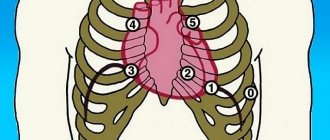
There are 4 points of cardiac auscultation:
- Mitral valve area.
- Aortic valve area.
- Pulmonary valve area.
- Tricuspid valve area.
The heart examination has the following algorithm:
- definition and changes of I, II tones;
- assessment of III and IV tones;
- noise detection;
- listening to three-part rhythms.
Normally, during auscultation of the heart at four points, the doctor hears two abrupt sounds. They are called the first systolic sound, as well as the second diastolic sound. In the presence of pathologies, clicks are heard and rhythm disturbances are observed. If additional sounds of III and IV are heard, which create a gallop rhythm, it means that the myocardium is significantly weakened. This way you can diagnose hypertension, decompensated heart defects, myocarditis and other pathologies.
Auscultation of the lungs in children
Auscultation of the lungs in children is an important diagnostic method that allows us to identify pathology of the respiratory system in young patients. The examination technology coincides with the principle of the procedure in adults.
Features of lung auscultation in children:
- The need to use smaller membranes or funnels;
- Poor development of the chest muscles, which leads to a significant increase in breathing sounds. This type of breathing is called puerile;
- The need for more careful control of the temperature of the phonendoscope applied to the child’s skin. Children react negatively to the touch of a membrane or funnel that is too cold.
The sequence of points and the principles of the procedure described above are relevant for small patients. Using auscultation, the presence and nature of wheezing, the localization of the inflammatory process, and the progression of organic or functional changes in the bronchopulmonary system are recorded.
Important! When using auscultation in children, the doctor always remembers that young patients are rarely distinguished by patience. Therefore, experienced pediatricians carry out diagnostics quickly, trying to turn the examination into a game.
Sometimes, for high-quality auscultation in a restless child, the doctor needs 2-3 attempts. Otherwise, the information obtained remains unreliable and may affect the choice of treatment method.
Lung examination
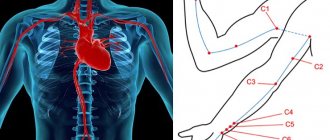
Auscultation of the lungs allows you to determine the type of breathing, detect additional noises and understand when they occur (during inhalation or exhalation). The doctor applies a stethoscope to symmetrical points on the left and right sides of the chest to conduct a comparative diagnosis.
Auscultation of the lungs provides the following algorithm of actions:
- listening from the front in the area of the collarbones with gradual movement down, and then from the back in a similar sequence;
- determination of vesicular and bronchial breathing by listening to points above the larynx and trachea;
- detection of additional sounds in the airways, alveoli or pleura.
When auscultating the points of the lungs, the patient sits or stands. To increase the area of interscapular space for listening, he crosses his arms over his chest. This makes noise detection more efficient. For the most informative auscultation of the lungs (listening for wheezing and clicking), the doctor asks the patient to place his hands behind his head, thereby increasing the area of the axillary zones.
Norilsk Interdistrict Children's Hospital
Adverse breath sounds
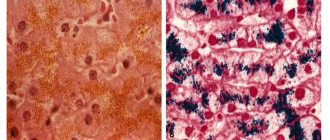
The greatest difficulties in assessing the auscultatory picture arise with the appearance of fine wheezing and crepitus.
Fine bubbling rales
They occur in the presence of liquid exudate in the lumen of the small bronchi. These wheezes are perceived as small crackling sounds and are heard from the very beginning of inspiration. Their sonority depends on the airiness of the tissues surrounding the bronchi. With inflammatory infiltration (pneumonia), the alveoli are filled with exudate, the lung tissue is compacted and the conduction of all sounds is good. Therefore, loud crackling sounds are heard against the background of bronchial breathing.
It must be remembered that bronchial breathing is laryngotracheal breathing, carried out without significant changes along the bronchi and through airless tissue to the surface of the chest wall, where the funnel of the stethoscope (or phonendoscope) is located.
If the airiness of the tissue surrounding the bronchi is preserved (for example, with bronchitis), in the presence of liquid exudate (this is rare for bronchitis), silent wheezing is heard.
Crepitus
Fig.1. Normal breath. Smooth expansion of lung tissue. The size of the arrows indicates the degree of reduction in intrathoracic pressure.
Fig.2. At the beginning and middle of inspiration, the acini do not disintegrate. A sharp expansion of the structural unit of the lung (bronchiole, acinus) at the end of inspiration, when the intrathoracic pressure becomes very low in order to resist the surrounding obstacle (gray area in the figure). The rest is in the text.
Unlike moist rales, crepitus occurs at the height of inspiration. There is no liquid exudate in the small bronchi. Straightening the acini and bronchioles is difficult because they are surrounded by dense tissue due to interstitial edema (left heart failure) or inflammation (bronchiolitis, fibrosing alveolitis, initial pneumonic exudation). For straightening of these structures to occur, a significant decrease in intrathoracic pressure is necessary. When it reaches the required level, they quickly straighten, giving a short vibration, heard as a click. The mass of these clicks is at the height of inspiration and is heard as crepitus.
Simple “unsticking” of the alveoli, if it exists, cannot produce such loud sounds.
It should be emphasized once again that this sharp straightening of relatively large structures, compared to the alveoli, occurs at the height of inspiration, which distinguishes crepitus from fine-bubble moist rales, which begin to be heard at the beginning of inspiration.
Depending on the cause of compaction of the interstitium of the lungs (congestive interstitial edema, inflammatory infiltration in the initial stage of pneumonia, inflammatory process with fibrosis), which interferes with the straightening of the alveoli, crepitus has a different sound and duration during the course of the disease:
- in cardiac and other seriously ill patients, after lying for a long time, during the first deep breaths, crepitus is heard over the lower lobes, which disappears after several breaths; Auscultation in such patients should begin from the subscapular areas
- persistence of crepitus in patients who have suffered myocardial infarction is one of the independent factors of poor prognosis
- with pneumonia, crepitus lasts for hours
- with fibosis alveolitis, it resembles cellophane crackling and can be heard for many weeks
Intermittent breathing sounds.
Saccaded breathing (not caused by pathology of the nervous and muscular systems) is most often associated with the presence of viscous effusion in the lumen of the bronchi
Fig.3. Saccaded breathing in bronchitis with thick exudate. As you inhale, the lobular bronchi gradually expand and become patent.
Pulmocardial or cardiopulmonary breathing is heard at the borders of relative cardiac dullness and posteriorly in the interscapular and subscapular regions on the left. It is caused by changes in heart size during systole and diastole. Often such breathing is heard during intensive heart work in patients with low hemoglobin, in pregnant women in late stages, with large heart sizes of any etiology with preserved ejection fraction. Sometimes in pregnant women this breathing is heard quite far from the heart.
Abdominal examination
There are 9 points of auscultation of the abdomen:
- 3 epigastric (2 - right and left subcostal zones, 1 - epigastric);
- 3 mesogastric (2 - right and left lateral flanks, 1 - umbilical zone);
- 3 hypogastric (2 - right and left iliac regions, 1 - suprapubic).
During the examination, the patient lies on his back, with his arms and legs extended straight. The doctor is on the right and applies the stethoscope to symmetrical areas of the abdomen in the direction from left to right. Normally, periodic peristalsis is heard. Its pathological strengthening is one of the signs of intestinal obstruction, and its weakening indicates intestinal atony or general peritonitis.
Through points in the abdominal cavity, the renal, iliac, and femoral arteries can be examined. The presence of systolic murmur indicates congenital or acquired narrowing of blood vessels, which is most often observed in atherosclerosis.
What is lung auscultation?
Auscultation is a method based on listening to changes in sounds that occur during the functioning of internal organs and systems. In the case of respiratory dysfunction, the doctor assesses the nature of the functioning of the lungs and bronchi.
A technique for studying breathing in a similar way was developed during the time of Hippocrates (IV-III centuries BC). To diagnose respiratory pathology, the doctor, during a standard examination of the patient, put his ear to the chest and listened for any extraneous or altered sounds.
The described method is called direct auscultation. In modern medicine, in 99% of cases an indirect version of the technique is used. Doctors use special instruments to auscultate the lungs - phonendoscopes (stethoscopes).
The device consists of a membrane and/or funnel that fits tightly against the area of the body being examined. The latter is connected by tubes (sound ducts) with rigid arms ending in ear olives. Due to the concentration of sound from the focus being studied, the doctor clearly hears what is happening under the membrane.
Auscultation of the lungs should be performed in all patients suffering from some form of respiratory pathology. The diagnostic method is simple, does not require the use of additional equipment and remains the basis for the initial assessment of the patient’s lung condition.
For what diseases
Over two thousand years of history of listening to the lungs, doctors have accumulated experience in diagnosing various diseases “by ear”. At medical universities, young doctors are taught how to recognize this or that pathology using a phonendoscope.
Diseases that are diagnosed using auscultation:
- Acute or chronic bronchitis;
- Pneumonia. Pneumonia is a serious pathology that changes the function of the relevant organs. Auscultation of the lungs during pneumonia is a method used additionally to monitor the quality of therapy;
- Bronchial asthma;
- Hydro- or pneumothorax - accumulation of fluid or air in the pleural cavity;
- Acute pulmonary edema is stagnation of blood in the tissues of the corresponding organ.
Using the described technique, tuberculosis or lung cancer can be suspected. However, these diagnoses cannot be established without the use of auxiliary methods.
Important! Auscultation is the primary diagnostic method, allowing the doctor to get a general picture of pulmonary dysfunction. To clarify the cause of the symptoms characteristic of a particular case, additional procedures are required. Otherwise, important details that affect the patient's outcome may be missed.
What you need to know and possible consequences
Auscultation of the lungs is the generally accepted standard for diagnosing diseases of the respiratory system. The procedure is safe for the patient. During the examination, the person does not feel any discomfort except for the touch of a cool phonendoscope. The duration of the examination depends on the severity of the pathology. On average, a doctor needs 2-5 minutes to fully carry out the corresponding procedure.
Undesirable consequences of auscultation are a myth. It is extremely difficult to harm a patient using the appropriate technique.