Cardiac output is a concept used in medicine that refers to the amount of blood ejected by the heart in one minute. Technically, it is calculated as the product of heart rate and stroke volume.
An increase in heart rate is a compensatory mechanism for increasing oxygen supply to tissues.
Factors that influence systolic volume are the volume of blood pushed by the heart into the aorta during the contraction period, preload, afterload, and contractile function.
Today, there are a number of techniques that allow us to obtain cardiac output measurements in a very efficient and non-invasive way. The Fick technique, which was used previously, has been replaced by more modern methods.
Pulse wave analysis resulted in a continuous and minimally invasive measurement of cardiac output. Other techniques, such as bioremediation, Doppler or echocardiography, allow us to obtain cardiac output measurements in a non-invasive, rapid and reliable manner.
What is sudden cardiac arrest?
When the heart suddenly stops, it stops pumping blood.
Sudden cardiac arrest is not the same as a heart attack. A heart attack occurs when one or more of the arteries supplying blood to your heart becomes clogged or blocked. As a result, the heart muscle may suffer. This can be thought of as a problem with the “heart piping”. Sudden cardiac arrest can occur when the heart begins to beat at a dangerously fast rate. This can be thought of as an "electrical" heart problem. Even if the problem with the cardiac pipeline is corrected by angioplasty, bypass surgery, or some other method, the risk of sudden cardiac arrest still remains.
Causes of sudden cardiac arrest.
If you have heart failure or have had a heart attack, there is a chance that your heart muscles are damaged. In this case, the conduction (electrical) system of the heart may also suffer, creating a risk of sudden cardiac arrest. If this situation applies to you, consult with your doctor about the advisability of using an implantable defibrillator for safety reasons.
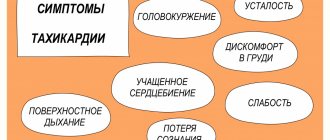
Sudden cardiac arrest has no warning signs.
Some people may experience palpitations or dizziness, which is a warning sign that a dangerous rhythm disorder may be occurring. But in the vast majority of cases, sudden cardiac arrest occurs without warning. There is no drug that is 100% effective in preventing sudden cardiac arrest. The most effective treatment for sudden cardiac arrest is defibrillation. Defibrillation is the application of a high-energy electrical shock to the heart to restore normal heart rhythm. To prevent death, defibrillation must be performed within a few minutes.
An implantable defibrillator is always ready.
Ambulance crews use external defibrillators. A small device implanted under your skin, an implantable cardioverter defibrillator, can also restore your heart's rhythm and save your life. An implantable defibrillator is always ready to help, monitoring your heart function around the clock. If your implantable defibrillator detects an abnormal rhythm, it automatically provides therapy. An implantable defibrillator is always ready to help you. You can consider it an ambulance that is always with you.
Reduced vascular resistance of a blood vessel
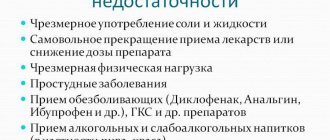
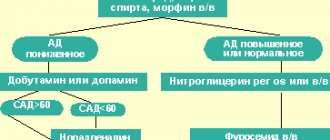
Arteries also have muscles. The more they contract, the smaller the channel through which blood flows, and the greater the tension on the heart muscle. Angiotensin, a naturally occurring hormone, is a very powerful blood vessel constrictor. Drugs that inhibit the formation of angiotensin or block its ability to bind to a blood vessel help relax the vascular muscles and are the basis of the Heart Failure Society of America Guidelines. Examples include captopril (Capoten), enalapril (Vasotec), valsartan (Diovan), and losartan (Cozaar). Because of this relaxation, the heart can pump out more blood per beat, improving EF. The drug combination hydralazine and isosorbide (Bidil) may be effective in patients who are resistant to—or intolerant to—angiotensin inhibitors.
Do I need an implantable defibrillator?
Doctors of several specialties deal with heart problems. A cardiologist treats problems such as high blood pressure, high cholesterol, and clogged arteries. An arrhythmia specialist focuses on problems with the heart's electrical system that affect how your heart beats. This specialist can determine whether you need an implantable defibrillator.
Typically, candidates for implantable defibrillators have one or more of the following risk factors:
- Heart failure;
- (a heart condition in which the heart's ability to pump blood is reduced);
- Previous myocardial infarction;
- One of the family members had sudden cardiac arrest;
- Low ejection fraction.
What is ejection fraction?
Ejection fraction is a measure of the percentage of blood that is ejected from the heart into the aorta during each contraction. Typically, at rest, a healthy heart, when contracting, throws out 50-70% of the blood in it. Many people with heart failure have an ejection fraction of less than 40%. A lower than normal ejection fraction means that your heart is not pumping efficiently and cannot meet your body's need for an efficient blood supply.
Why is it important to know your ejection fraction?
Your ejection fraction is one measure your doctor can use to recognize heart failure and assess your risk of sudden cardiac arrest. The latest medical research shows that people who have not had or have had sudden cardiac arrest with an ejection fraction of less than 40% are at greater risk of dangerously accelerated heart rates and sudden cardiac arrest.
How is ejection fraction measured?
Typically, a simple and painless method called echocardiography, or “cardiac ultrasound,” is used to determine ejection fraction. This method, which uses ultrasound to evaluate cardiac function, is widespread and can be performed in most medical institutions.
Relaxation of the heart muscle
In response to decreased EF, the body releases substances such as adrenaline, which increase the speed and force of ventricular contraction. While temporary effective, chronic elevations of these compounds cause the heart muscle to strengthen and reduce its movement. Beta blockers are drugs that counteract these actions, reducing tension in the heart wall and improving the ability to contract. Three of these are recommended: carvedilol (Coreg), metoprolol succinate (Toprol XL), and bisoprolol (Zebeta). Beta blockers are most often used in combination with angiotensin inhibitors.
What is an implantable defibrillator?
An implantable defibrillator is a device similar to a pacemaker (artificial pacemaker) that has been used since the early 90s. It is small in size - no larger than a pager - and is implanted under the skin of the upper chest. The device contains a battery and a microcomputer necessary to correct your rhythm. An implantable defibrillator is connected to the heart by thin, insulated wires called electrodes. If the device detects that your heart rhythm is abnormal, it sends electrical signals to restore it. Most implantable defibrillators last 5-7 years before needing to be replaced.
How does an implantable defibrillator work?
Depending on the programmed mode, the implantable defibrillator may initially send low-energy, painless electrical signals to restore rhythm. If they do not work, a stronger shock is sent. People describe this discharge as a sudden feeling of discomfort, sometimes even painful, but quickly passing. Often everything ends before you understand what actually happened. Another positive thing is that an implantable defibrillator protects you constantly, 24 hours a day.
What happens during the implantation procedure?
Typically, the implantation procedure is performed quickly, safely, and usually under local anesthesia. It does not require open heart surgery, and most patients return home within 24 hours. The following section is a general description of what happens during the implantation procedure. Your case may be different, you can discuss all the details with your doctor.
During implantation.
Typically, patients are sedated before the procedure and do not feel any pain. Your doctor will make a small incision in your upper chest and place electrodes through a vein into your heart. The doctor will then connect the electrodes to the implantable defibrillator and program the device. Next, an implantable defibrillator will be placed under the skin and the incision will be sutured. The doctor will check to see if the implantable defibrillator is working properly.
After the procedure.
After implantation of the device, the patient usually spends the night in the ward and can return home in the morning. You may feel a small bump under the skin where the device is located; this area may be sensitive. It is usually recommended to limit movement of the arm on the implanted side for 2-6 weeks. You can obtain more detailed care instructions from your doctor. However, you can expect a quick return to your previous activities after surgery. If you have any questions, please ask your doctor or nurse.
Starting life with an implantable defibrillator: the first six weeks.
It's time to start living a full life again. We hope it will be filled with hope and confidence. Of course, until healing occurs, you may experience some discomfort. Also, in order not to cause displacement of the electrodes, you may have to slightly limit the movements of your left hand. Typically these restrictions are recommended for 2-6 weeks. Your doctor will tell you in more detail what movements and strains you should avoid. If you have questions about what you can or cannot do before you recover, don't hesitate to ask your doctor or nurse. Your family and friends will be interested in hearing about your implantable defibrillator. You may want to show the implantation site and talk about the operation. Tell everyone how glad you are to feel recovered from your illness. Now is the time to tell your friends and family about what you are planning to do soon. Choose one of your favorite activities and make plans, think about how you will do it again. Believing in yourself and doing enjoyable, enjoyable things makes a big contribution to the healing process.
Living with Success: Achieving the Confidence You Need.
A new device for your heart will help you feel calm and confident. It is always on alert, constantly taking care of your heart 24 hours a day. If your implantable defibrillator detects a rhythm disorder, it sends an electrical impulse to restore it. You can imagine that this is an ambulance that is always nearby. And very soon you will feel the contribution of these positive effects in your everyday life. Remember that you will still need to continue taking your medications and have your device checked periodically by your cardiologist and electrophysiologist (heart rhythm specialist). Either way, your life is in your hands, so enjoy it. Keep making plans. Tell everyone how good you feel, what you have achieved thanks to this, and what you are going to do. For a high quality of life, identify what you enjoy doing and return to an active lifestyle. Always remember that if you have questions about any special activities, such as driving or returning to work, you should consult your doctor.
What happens after the shock: Have a plan.
If your implantable defibrillator detects an abnormal rhythm in your heart, it will automatically deliver therapy—a high-energy shock. Patients who have undergone such therapy describe this discharge as a sudden feeling of discomfort, sometimes even painful, but quickly passing. It also means that the implantable defibrillator has done its job and may have saved your life. Your doctor will give you specific instructions about what to do after the shock. Together with them, develop an action plan that suits you. This plan may include what you will immediately need to do and some of your favorite activities that you can continue to do after the discharge. Keep the plan in a convenient place so you can refer to it. Also, be sure to tell your loved ones and those who care about you about this plan so that they can understand how to help you. It is important to understand that what you were doing during the discharge did not cause it. Typically, you will be able to continue enjoying your favorite activities. Talk with your doctor about when you can return to your activities and whether any changes need to be made. Although the discharge may make you feel temporarily uneasy, it is important to return to your daily activities and focus on the things you love.
You create your own life.
Life is made up of moments, so the more pleasure we get from them, the more fruitful our life becomes. An implantable defibrillator can help you enjoy life more so you can look forward to the future that means so much to you. These can be simple, “earthly” joys, such as walks in the park, working in the garden, or communicating with your loved ones. The important thing is that these moments often make life richer, so hurry up to enjoy them.
Muscle pump
The movement of blood through the veins is ensured by a number of factors: the work of the heart, the valve apparatus of the veins, the “muscle pump”, etc. The veins of the upper and lower extremities are equipped with valves, and the deep veins are surrounded by muscles. With physical
When under load, the muscles act like pumps, putting pressure on the veins from the outside. The more frequent and active the movements, for example when walking, the more effective the “pumping action” of the muscles. True, muscle contraction, pinching blood vessels, impedes blood flow. But if the contractions are intermittent, then the decrease in blood flow during the contraction phase is effectively compensated by oxygen bound to myoglobin. Therefore, during rhythmic exercise that occurs when running, skiing, or cycling, the blood supply to the muscles of the limbs increases significantly. Contraction of the abdominal muscles forces a significant amount of blood out of the vessels of the liver, intestines and spleen, increasing blood flow to the heart and thereby affecting cardiac output.
When muscles contract, the veins in them are compressed, which immediately leads to an increase in blood flow to the right ventricle (muscle pump). An increase in the outflow of venous blood from the muscles of the lower extremities promotes rapid filling of the heart and, in addition, increases the perfusion pressure in the lower extremities by reducing the pressure in the veins of the leg and foot.
Activation of the muscle pump is accompanied by changes in the post-capillary vessels (mainly veins) of the systemic circulation.
Physical exercise causes a reflex increase in the tension of the walls of the venous vessels in both working and non-working limbs. This tension is maintained throughout the load and is proportional to its severity.