Heart pain with gastritis
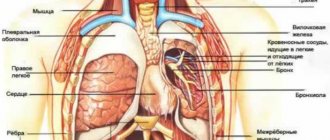
In close proximity to the heart there are such important organs as the stomach and esophagus, lungs, spine, ribs, and sternum. Their diseases can create a pain syndrome that is very similar to heart pain. The most common noncardiac causes of chest pain are diseases of the gastrointestinal tract.
With gastritis and peptic ulcers, referred pain in the heart most often occurs after eating or, on the contrary, on an empty stomach
With gastritis and peptic ulcers, referred pain in the heart most often occurs after eating or, conversely, on an empty stomach. They are stabbing in nature, can last a long time and do not go away after taking heart medications.
Heart pain with gastritis symptoms:
- nausea or sometimes vomiting;
- feeling of heaviness under the left rib;
- sour taste in the mouth, heartburn;
- frequent and severe belching.
Most often, patients suffering from such “heart pain” are sent to see a cardiologist, who, after conducting the necessary tests, can correctly diagnose the disease and refer the patient to a gastroenterologist.
We diagnose and treat acute stomach pain
Representatives of our medical clinic “KDS Clinic” diagnose the presence of diseases in the early stages. You will receive consultation during the initial examination and further treatment. Clinic experts will examine you and receive test results as soon as possible. You can find prices for all types of diagnostics on our official website.
The clinic regularly runs promotions for comprehensive examinations of all body systems. All detailed information is posted on the website of the private medical clinic “KDS Clinic”. We are located in Moscow, at Belozerskaya street 17-G. Be healthy!
Gastritis hurts my heart
Pain in the heart and pain in the abdomen can have a common localization, so it is extremely difficult to find its source. This problem should be addressed by the attending physician. It is enough for the patient to remember the disturbing symptoms and their severity in order to tell a specialist about it. Sometimes it is difficult to distinguish diseases of the gastrointestinal tract from cardiac pathologies.
Sharp pain in the stomach and pain in the heart can occur with gastritis. The patient feels something tingling in the chest area. Discomfort occurs in attacks due to the development of inflammation of the mucous membrane of the stomach or intestines.
Cardialgia can be distinguished from gastritis by the symptoms characteristic of the latter disease:
- nausea;
- bloating;
- heartburn;
- lack of appetite.
After eating, the patient feels as if something is pressing from the inside. The discomfort goes away if you rest a little. The chronic form of gastritis is characterized by astheno-vegetative syndrome. It manifests itself as irritability, headache, weakness and other symptoms.
One of the manifestations of the pathology of gastritis is gastroesophageal reflux; gastric juice entering the esophagus provokes pain in the chest area.
Feeling of a lump in the stomach
Gastritis
11885 21 August
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Feeling of a lump in the stomach: causes of occurrence, what diseases it occurs with, diagnosis and treatment methods.
The feeling of a coma in the stomach is described when one experiences a feeling of heaviness, discomfort and fullness in the stomach, even when it is only slightly filled. Sometimes patients find it difficult to determine the exact location of the coma and point to the lower third of the sternum or solar plexus. In some cases, a feeling of a lump and cramps in the stomach may occur on an empty stomach.
Types of feeling of a coma in the stomach
A feeling of heaviness or coma in the stomach can be an independent symptom, but may be accompanied by other unpleasant sensations. Sometimes it is heartburn, sour belching, bloating, constipation.
In some cases, a feeling of a lump appears when swallowing
, making it difficult for chewed food to pass through.
In addition, patients may complain that food did not enter the stomach, but stopped in the esophagus.
In such patients, vomiting of unchanged food is possible. When describing symptoms, you should pay attention to the time of onset of discomfort - before
or
after eating
.
The patient may feel heaviness in the stomach with pain or heartburn, on an empty stomach or after eating, and night pain also occurs.
Sometimes the sensation of a lump in the stomach occurs
regardless of food intake
.
In such cases, they complain of stomach spasms
, sometimes accompanied by a feeling of a lump in the throat.
What diseases cause a sensation of a lump in the stomach?
Eating more than your usual amount of food
, accompanied by a feeling of fullness and heaviness in the stomach. This condition is not a manifestation of the disease and goes away on its own after some time.
It should be noted that stomach capacity varies depending on eating habits.
People who are small or
have undergone gastric resection
can eat a small portion, otherwise they will not only experience a feeling of heaviness or fullness in the stomach, but also vomiting.
A sensation of coma may occur when consuming foods that cause excess gas.
, as well as
food that is difficult to digest
(salads with mayonnaise, fatty, fried and smoked dishes) and
highly carbonated drinks
.
When eating dry and hastily,
an unpleasant sensation in the epigastric region is caused by poor processing of the food bolus with saliva and insufficient secretion of gastric juice.
However, a feeling of coma or discomfort in the stomach, or more precisely, in the epigastric region, may appear after eating even a small amount of food
.
This condition can be caused by diseases of the gastrointestinal tract or other reasons.
First of all, they assume indigestion, or functional dyspepsia. Its symptoms most often include pain and discomfort immediately after eating, a feeling of heaviness and fullness in the stomach, heartburn, belching, nausea, sometimes vomiting, reflux of stomach contents into the esophagus, bloating and bowel dysfunction.
Dyspepsia can be a symptom of both functional disorders of the gastrointestinal tract and organic diseases.
Functional causes of dyspepsia are often caused by errors in diet and medications.
Iron ions have an irritating effect on the gastric mucosa, which is most pronounced when taking medications based on ferrous iron. Nonsteroidal anti-inflammatory drugs, which are systematically taken for rheumatic and non-rheumatic diseases of the musculoskeletal system, also cause undesirable effects: heaviness and discomfort in the stomach, nausea, vomiting, and dyspeptic disorders.
Neurological disorders
(neuroses, depression), psychological trauma almost always affects the state of the gastrointestinal tract, leading to impaired motility.
Functional dyspepsia is not accompanied by erosive or ulcerative lesions of the stomach; its symptoms disappear when the general state of health is normalized.
One of the common causes of discomfort in the stomach immediately after eating is
gastritis
. It is accompanied by functional and inflammatory processes that have a negative effect on the gastric mucosa. Symptoms of gastritis include heaviness and pain in the stomach, indigestion, nausea, heartburn, sour belching and bloating when eating any food. The inflammatory process leads to atrophy of the mucous membrane and disruption of the glands that secrete gastric juice.
Insufficient gastric juice and weak peristalsis of the stomach and intestines make it difficult to digest food.
Gastritis is often accompanied by dyspepsia. In addition to a feeling of heaviness and aching pain in the epigastric region after eating, poor appetite, weakness, fatigue, and irritability are noted. When pressing on the abdomen, a dull pain appears in the projection of the stomach.
Impaired motor-evacuation functions
upper digestive tract is always accompanied by a feeling of coma or a feeling of heaviness in the stomach. Disorders of esophageal motility are usually caused by incoordination of the esophageal sphincters. Uncoordinated work of the esophageal muscles can lead to a delay in the bolus of food on the way to the stomach, the reflux of food particles into the respiratory tract, and reflux (return of stomach contents into the esophagus). Impaired gastric motility leads to slow emptying, which is accompanied by a feeling of heaviness and fullness even with a small amount of food consumed, pain in the epigastric region, heartburn, nausea and vomiting.
Motility disorders of the esophagus and stomach may be associated with gastroesophageal reflux disease, gastritis, tumors and stenoses (narrowings), metabolic disorders (hyperkalemia, hypercalcemia), postoperative complications of gastrectomy, taking certain medications (opiates, antidepressants, hormones), alcohol and nicotine .
Peristalsis worsens with a sedentary lifestyle and with age.
Stomach cancer can also cause symptoms such as a feeling of heaviness or a lump in the stomach. Moreover, depending on the location of the tumor, its manifestations vary. If the tumor is located closer to the esophagus, problems with swallowing food occur. This is accompanied by increased salivation, nausea, vomiting, and pain in the epigastric region. When the tumor is localized in the lower parts of the stomach, closer to the duodenum, a prolonged feeling of heaviness after eating and bloating is characteristic. When burping, a putrid odor may be felt.
Which doctors should you contact if you feel a lump in your stomach?
If there is a constant feeling of a lump in the stomach or a feeling of heaviness, it is necessary to contact or to make a preliminary diagnosis. The gastroenterologist may also refer the patient to an oncologist. A consultation may also be required.
Diagnosis and examination if you feel a lump in the stomach
First of all, clinical blood and stool tests are necessary for differential diagnosis.
Gastritis affects the heart
Chest pain is a fairly common symptom that can occur not only with cardiovascular pathologies, but also with any other abnormalities that manifest themselves in different systems of the body. The muscles of the stomach are no exception, which, with certain disorders, may well cause heart pain.
With gastritis, the gastric mucosa becomes significantly inflamed, causing acute pain, which intensifies significantly when eating spicy, salty or fatty foods. However, such pain is not always localized in the abdominal cavity; sometimes it appears in the chest on the left.
Such attacks of pain occur periodically and are somewhat different from characteristic pain in the heart. You can determine what exactly hurts with gastritis - the heart or the stomach, using the accompanying symptoms of abdominal pathology, such as attacks of severe nausea, vomiting, after eating, a feeling of heaviness in the stomach, intestinal upset, bloating, appetite during gastritis is significantly reduced or disappears completely.
Such symptoms can be caused not only by eating the wrong food, but also by a feeling of hunger. It should be noted that prolonged ignoring of such symptoms will necessarily lead the patient to noticeable weight loss.
Diagnosis of acute cutting pain in the stomach
If you are concerned about the above symptoms, we advise you to go to the clinic and undergo diagnostic tests. Diagnosis of acute pain in the stomach is as follows:
- Consultation with a gastroenterologist. Highly qualified doctors at the private medical clinic “KDS Clinic” will help you find out about your health status and diagnose the disease as soon as possible. After the doctor conducts an initial examination and palpation of the stomach, he will determine the nature, frequency and intensity of pain. It can be aching, cutting, dull and sharp. The diagnosis depends on the nature of the pain.
- Taking tests. Patients undergo a general analysis of blood, urine, and stool. Patients then undergo diagnostic examinations. The examination method depends on the patient's condition.
- Endoscopy. The examination method is the most accurate and allows you to diagnose stomach diseases
To diagnose the complete condition of the body and find out about the presence of other diseases, patients are referred for ultrasound diagnostics. You will undergo an ultrasound examination of the abdominal organs. In some cases, examinations are performed using contrast fluid.
Such procedures include computed tomography and magnetic resonance imaging. Computed tomography and magnetic resonance imaging are the most accurate examinations in modern medicine. You will be able to see changes in the body, learn about neoplasms and disorders.
In addition to acute pain, patients experience:
- sharp pain in the stomach;
- dull pain in the stomach;
- aching pain in the stomach.
Sharp pain in the stomach appears due to the production of gastric juice and irritation of the damaged gastric mucosa. Sometimes the disease develops into gastritis and duodenal ulcer.
Dull pain in the stomach occurs with chronic gastritis. The pain is nagging in nature and occurs after eating. When dull pain occurs, patients are diagnosed with duodenitis. Duodenitis is inflammation of the duodenal mucosa. Pathology manifests itself in all age categories. Acute and chronic duodenitis are classified.
Aching pain in the stomach occurs when bacteria appear in the body. These include infectious diseases. Aching pain is affected by an incorrectly formulated diet, consumption of harmful foods, and chronic gastritis. Pains of this nature appear during the day and at night.
Gastritis or heart
One of the manifestations of the pathology of gastritis is gastroesophageal reflux - gastric juice entering the esophagus provokes pain in the chest area. The heart is located in the sternum cavity adjacent to the stomach. Such attacks are often mistaken for a stroke, although hospitalization is necessary for reflux in the same way as for a stroke.
After vomiting, you feel a little better, however, discomfort, a gray tint of the tongue, and a rapid pulse will help determine that gastritis is in acute form. A decrease in pressure during the rapid development of an attack provokes an increase in heart rate and pulse.
If you are worried about heartburn, discomfort in the abdominal cavity associated with eating or during prolonged fasting, it may be pain associated with pathology of the gastrointestinal tract. However, if a symptom such as a burning sensation (often interpreted as heartburn) appears, while walking quickly, or climbing stairs, which is in no way related to food and passes quickly, you need to consult a cardiologist.
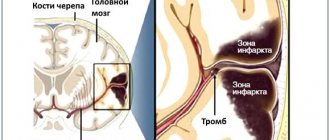
The cause of pain in the heart can be diseases of the gastrointestinal tract
Pain in the esophagus
General information
The esophagus is part of the alimentary canal.
It is a hollow muscular tube flattened in the anteroposterior direction, through which food from the pharynx enters the stomach. The esophagus of an adult has a length of 25-30 cm. It is a continuation of the pharynx, begins in the neck at the level of the VI-VII cervical vertebra, then passes through the chest cavity in the mediastinum and ends in the abdominal cavity at the level of the X-XI thoracic vertebrae, emptying into the stomach. Accordingly, the areas of occurrence in the esophagus are distinguished: cervical, thoracic and abdominal parts.
The lumen of the esophagus is not uniform; along its length it is customary to distinguish three narrowings. The first of them is located at the junction of the pharynx with the esophagus, the second at the intersection of the esophagus with the left main bronchus, and the third at the passage through the diaphragm. In the upper part of the esophagus there is the upper esophageal sphincter, in the lower part, respectively, the lower esophageal sphincter, which play the role of valves that ensure the passage of food through the digestive tract in only one direction and prevent the entry of aggressive stomach contents into the esophagus, pharynx, and oral cavity. The wall of the esophagus is made of:
- mucous membrane;
- submucosa;
- muscular and adventitial membranes.
The muscular lining of the esophagus consists of two layers: the outer longitudinal and the inner circular. In the upper part of the esophagus, the muscular layer is formed by striated muscle fibers. At approximately the level of one third of the esophagus (counting from the top), striated muscle fibers are gradually replaced by smooth muscle fibers. In the lower part, the muscular layer consists only of smooth muscle tissue.
The mucous membrane is covered with stratified squamous epithelium; in its thickness there are mucous glands that open into the lumen of the organ. Pain in the esophagus is perceived as a feeling of discomfort in the chest and may be accompanied by dysphagia and regurgitation.
Characteristics of pain in the esophagus
In diseases of the esophagus, pain is usually localized behind the sternum, radiates to the back, to the right and left of the sternum, is associated with eating and is accompanied by difficulty swallowing. More often the pain is caused by damage to the esophagus:
- perforation;
- burns with concentrated solutions of caustic alkalis or strong acids;
- neuromuscular diseases (cardia achalasia, esophagospasm, diverticulum);
- tumors;
- inflammatory and peptic changes (esophagitis, peptic ulcer of the esophagus, hiatal hernia, peptic strictures).
Causes of pain in the esophagus
Pain in the esophagus may be a consequence of reflux esophagitis. This is an inflammatory process in the distal part of the esophagus, caused by the action of gastric juice, bile and intestinal contents on the mucous membrane of the organ during gastroesophageal reflux and accompanied by the appearance of characteristic symptoms (heartburn, retrosternal pain, dysphagia).
Pain in the esophagus is observed with its injuries, which are divided into internal (closed) from the mucous membrane and external (open), with penetrating wounds of the neck and chest.
Injuries to the esophagus from the inside are also possible when foreign bodies enter it. Bedsores of the esophageal wall occur when probes are in it for a long time, from the pressure of the cuff of an endotracheal or tracheostomy tube.
Perforation of the esophageal wall can occur due to various diseases:
- tumors;
- peptic ulcer;
- chemical burns.
When malignant tumors , damage to the esophagus occurs due to tumor disintegration.
The first symptom of esophageal perforation is a sharp pain behind the sternum , which tends to increase, intensifying with the following reflex actions of the body:
- cough;
- swallowing;
- deep breath.
With spontaneous rupture of the esophagus, unbearable pain occurs most often during vomiting , is localized at the xiphoid process, and radiates to the epigastric region, back, and left shoulder. Subcutaneous emphysema (above the collarbone and on the neck) and sometimes bloody vomiting .
Esophageal rupture
Blunt injuries to the neck, chest and abdomen can lead to malnutrition and necrosis of the esophageal wall as a result of compression between the sternum and vertebral bodies. In this case, damage to neighboring organs is often noted. Direct trauma to the esophagus can occur during operations on the mediastinal and pulmonary organs.
Experts also observe cases of spontaneous rupture of the esophagus. Factors predisposing to spontaneous rupture of the esophagus are:
- alcohol intoxication;
- binge eating;
- vomiting during gagging movements;
- abdominal muscle tension;
- contraction of the diaphragm and muscular lining of the stomach.
As a result of a significant increase in pressure in the esophagus, a longitudinal or transverse rupture of its wall occurs, most often directly above the diaphragm (posterior left in 95%, right in 5% of cases). A rupture of the esophagus occurs when trying to restrain vomiting or when there is a lack of coordination in the work of the above sphincters as a result of severe alcohol intoxication or diseases of the central nervous system.
The rupture most often takes the form of a linear wound and can spread to the stomach. With spontaneous ruptures of the esophagus, pain occurs suddenly (usually during vomiting) in the area of the xiphoid process, and can radiate to the epigastric region, back, or left shoulder. Bloody vomiting, mediastinal and subcutaneous emphysema are noted, shock develops, and body temperature rises.
Foreign bodies in the esophagus
Most often, meat, fish and bird bones, pins, coins, buttons, needles, paper clips, and less often pieces of wood, glass, dentures, nails, badges and other objects are retained in the esophagus. The reasons for foreign bodies entering the esophagus are different:
- negligence in the cooking process, when foreign objects may get into food products;
- hasty eating, inattention while eating;
- insufficient chewing of food;
- the habit of workers of some professions (shoemakers, tailors, carpenters) to hold needles and nails in their mouths while working;
- deliberate ingestion of foreign objects by mentally ill people.
When a foreign body is swallowed into the esophagus, the pain is localized behind the sternum, intensifies with swallowing, and increased salivation occurs. Subsequently dysphagia purulent mediastinitis may subsequently develop Retention of a foreign body in the esophagus threatens complications even after a long period - from several months to several years.
Burns of the esophagus
Burns of the esophagus occur either from accidental ingestion of caustic substances or from a suicide attempt. Most often, burns of the esophagus are observed with concentrated solutions of alkalis and acids, less often with phenol, iodine, sublimate and other chemicals. Patients experience severe pain in the esophagus, epigastric region, oral cavity and pharynx. With peptic esophagitis, pain in the esophagus can occur both during swallowing saliva and during the passage of food through the esophagus. Pain is localized in the following parts of the body:
- behind the sternum or under the xiphoid process;
- radiates to the back of the interscapular space, up the esophagus, into the neck, jaw, left half of the chest;
It often resembles coronary pain, differing from it in the lack of connection with physical activity, more often in dependence on the intake and nature of food, the position of the patient’s body, as well as the lack of effect from nitroglycerin.
Hiatal hernia
With a hiatal hernia, when gastroesophageal reflux , pain in the esophagus can mimic angina . In patients, often without physical or nervous stress, often after a heavy meal, in a horizontal position, pain appears behind the sternum, sometimes intense, often with typical radiation to the left arm. With large hernias, pain can radiate to the spine. The pain is not relieved by nitroglycerin, but becomes less intense when the patient is in an upright position. Attacks of pain may be accompanied by shortness of breath.
Neuromuscular diseases of the esophagus
Sometimes spontaneous pain occurs in the esophagus in the form of a “pain crisis.” With achalasia cardia, a pain crisis occurs in the early period of the disease, often at night, without an immediate cause. The pain is intense, radiating to the back, up the esophagus, neck, jaw, and lasts from several minutes to several hours.
The crisis occurs 1-3 times a month. Some patients with achalasia cardia experience pain when trying to swallow food. In these cases, the passage of food through the cardia leads to short-term, sometimes quite severe, usually cutting pain in the area of the xiphoid process spreading upward beyond the sternum, a feeling of fullness of the esophagus , then the pain disappears, and the patient continues eating.
Esophageal carcinoma
With esophageal cancer, a pain crisis occurs in advanced stages when the tumor into the surrounding tissue. The pain is usually not associated with swallowing, is more pronounced at night, is localized behind the sternum or at the xiphoid process, and can radiate to the
- back;
- neck;
- left half of the chest.
Attacks of severe pain in the lower retrosternal region can be caused by retrograde prolapse of the gastric mucosa into the esophagus. If this pain is not associated with eating and is not accompanied by dysphagia, it is difficult to distinguish from angina at rest. Frequently recurring chest pain, reminiscent in localization and radiation of the pain of angina pectoris, can be caused by esophagospasm (esophageal dyskinesia).
In many patients, it is possible to determine the connection between pain and dysphagia . In some cases, esophagospasm occurs outside of meals, against the background of emotional or physical stress. It is difficult to distinguish esophageal dyskinesia from an attack of angina, especially since taking nitroglycerin, due to its relaxing effect on smooth muscles, has a positive effect in both cases.
If you have pain in the esophagus, you should immediately seek help from a gastroenterologist. In case of injuries, you may need to consult a traumatologist and surgeon. Pain in the esophagus can be accompanied by serious complications throughout the body, so treatment of the disease should be taken responsibly.
Can gastritis radiate to the heart?
A strong heartbeat manifests itself as a feeling of disruption in the functioning of the heart; it seems that the heart is almost “jumping out” of the chest or freezing. Attacks may be accompanied by weakness, discomfort in the heart, and fainting. Such symptoms may indicate tachycardia, angina, or heart failure.
If you have at least one of these symptoms, it is important to immediately consult a doctor and undergo tests to determine an accurate diagnosis. Palpitations can occur during intense physical activity, as a result of a person's emotional arousal, or due to overeating.
The cause of pain in the heart can be diseases of the gastrointestinal tract. Most often, discomfort occurs during and after eating and is accompanied by attacks of nausea. This is due to an increase in acidity levels, which contributes to chest heaviness. Consult a doctor, because we may be talking about gastritis or an ulcer, as well as a hernia in the diaphragm.
Heart disease can cause digestive system upset. If gastrointestinal pathologies, such as gastritis, are not treated for a long time, it is worth visiting a cardiologist for consultation. Shortness of breath should also be an alarm signal: it usually goes away at rest. If shortness of breath against the background of pain in the sternum does not go away even with rest, but increases, again, you must urgently call an ambulance.
Our gastroenterologist, clinical pharmacologist Anna Eduardovna Babich answers
It can be immediately noted that chronic gastritis cannot currently be diagnosed only based on the results of a survey and examination of the patient. Many diseases begin with a pain syndrome. Even survey gastroscopy is sometimes not enough; a biopsy is necessary during the study, which, by the way, is a completely painless maneuver when performing gastroscopy.
The fundamental fact that needs to be proven during the examination is the presence of inflammation.
Abdominal pain is not always associated with inflammation; sometimes it is a functional disorder that does not require the use of complex medications.
It is important to exclude inflammation of the stomach, since it is the first step leading to ulcers and atrophy, which can “degenerate” into stomach cancer.
Symptoms of stomach disease, so-called gastric dyspepsia, without inflammation, are observed only in 5-10% of patients with chronic gastritis. But they are also painful for a person to bear, but can be easily relieved with certain medications.
Symptoms of gastric dyspepsia include:
pain and heaviness in the upper abdomen;
feeling of early satiety;
pain in the upper abdomen (epigastric region) on an empty stomach and after eating;
night pain in the epigastrium;
decreased appetite;
nausea;
vomit.
The trouble is that these very symptoms can also be markers of serious diseases of the gastrointestinal tract, which is why gastroenterologists are often forced to prescribe extensive additional examination (blood test, stool test, ultrasound, gastroscopy, etc.).
Patients with diabetes need to be especially wary, given the presence of visceral neuropathy (pathology of the processes of nerve cells of internal organs due to disruption of their energy metabolism in diabetes). Diabetics are characterized by a decrease or absence of perception of typical gastrointestinal symptoms; pathologies of their nerve fibers sometimes lead to the absence of pain even during a heart attack.
It is necessary to urgently visit a doctor, primarily a surgeon, if vomiting blood occurs, vomiting with dark contents – “vomiting coffee grounds”, if there is black stool (to exclude bleeding from erosions or ulcers).
Dark stools can occur not only with bleeding, but also with certain dietary habits, or with the use of a number of common medications, for example, bismuth preparations.
In a number of clinical situations, even in the absence of symptoms from the intestines and stomach, consultation with a gastroenterologist is necessary as planned:
- With vitamin B12 deficiency (a sign of autoimmune (atrophic) gastritis caused by problems in the immune system, in which one’s own antibodies cause the death of stomach cells);
- When infected with the microbe H. pylori, which is the main cause of chronic gastritis, ulcers, and stomach cancer;
- “Therapeutic” patients who often use non-steroidal anti-inflammatory drugs for the treatment of pain (headaches, joint pain, etc.), as well as as antipyretics, must remember their damaging effect on the mucous membranes of the upper gastrointestinal tract and the ability to cause not only inflammation, but also erosive and ulcerative lesions of the stomach and duodenum. The gastroenterologist recommends stomach-protective drugs.
It is imperative to carry out therapy for chronic gastritis, to fight not only with the help of diet, but also with the help of medications selected for the patient by a gastroenterologist. Based on the laboratory and instrumental data of a particular patient, the doctor prescribes an individual treatment regimen. This is extremely important, since even low-intensity pain of inflammatory origin in the stomach can lead to the launch of the long-known Correia cascade, i.e. damage to the stomach is the beginning of the degeneration of the cells of this organ and the development of not only erosions, but also stomach cancer.
One of the symptoms of a number of diseases, including stomach cancer, is a change in the perception of taste (dysgeusia), the appearance of an aversion to meat or other foods, and rapid weight loss that is not related to the patient’s plans to lose weight. A rapid decrease in body weight can be a symptom of gastrointestinal oncology, and also occur with helminthic, parasitic infestations, indicate exocrine pancreatic insufficiency and other diseases.
Finding out what exactly is behind even low-intensity, rare pain in each patient is the main task of a gastroenterologist, who necessarily involves the laboratory capabilities of the institution, as well as, in some cases, the equipment and experience of endoscopists. Only a correct diagnosis will allow the patient to be treated correctly and the future prognosis of the disease to be explained to him.