Laser therapy: what is it?
Diseases of the heart and blood vessels are treated in the department using different methods. Laser therapy is a highly effective and painless type of treatment that uses laser irradiation as the main active factor.
In medicine, laser therapy in the red and infrared ranges is most widespread. The red ray penetrates tissue depths of several millimeters, while the infrared ray can penetrate to a depth of several tens of millimeters. This irradiation is low-intensity and does not heat the tissue exposed to the laser.
The laser can be used to irradiate pathological areas either in contact with the problem area or at a distance. Intravascular laser therapy is also used.
The high effectiveness of laser therapy is explained by the powerful positive effect of laser radiation on vascular and blood cells.
The use of laser therapy leads to improved blood circulation, elimination of vascular spasms, improvement of their tone and blood flow in them, and relief of inflammatory processes. After laser irradiation sessions, processes in the heart muscle are normalized, and blood microcirculation is significantly improved.
Characteristics of cardiovascular diseases
Coronary heart disease is the most common chronic disease that leads to a sharp decrease in working capacity. When drug treatment does not bring results, some patients are refractory to antianginal drugs. Such patients are treated with non-drug methods, including low-intensity laser therapy, as well as surgery. In the case of surgical intervention, the most common operation is direct myocardial revascularization by autovenous coronary artery bypass grafting (CABG).
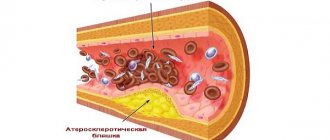
The basis of most diseases of the cardiovascular system is a violation of blood circulation and oxygen consumption by tissues. Low-intensity laser therapy improves microcirculation, saturates tissues with oxygen, normalizes cholesterol levels and lipid peroxidation indicators.
Scientific research results
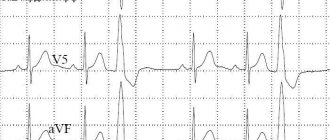
The clinical effect of laser therapy in patients with coronary artery disease is accompanied by anti-ischemic and antiarrhythmic effects, as well as favorable changes in the microcirculation system, an increase in myocardial contractility and an increase in its coronary reserve.
At the Moscow Scientific Center for Cardiovascular Surgery named after. A.N. Bakulev treated 159 patients with ischemic heart disease and arrhythmia using laser therapy. According to the results of the first course of treatment, the frequency of extrasystoles increased by 87.9%.
According to the book by G.V. Babushkina and A.V. Kartelisheva (2000), combined RT, carried out as prophylaxis, stops the progression of coronary atherosclerosis and stabilizes the pathological process, prolonging remission on average. This procedure is 2.5 times more effective compared to traditional therapy. Laser therapy also reduces the number of deaths and the development of acute myocardial infarction by 2 times.
The authors argue that one of the leading links in the therapeutic effect of RT in ischemic heart disease is direct participation in the mechanisms of normalization of the functional state of the left ventricular myocardium. A number of researchers in their works note the analgesic effect of RT. This is explained by stimulation of the formation of endorphins and norepinephrine. The effectiveness of RT for ischemic heart disease is explained by the improvement of central hemodynamics.
According to the results of Holter monitoring, high antianginal and anti-ischemic effectiveness of laser therapy was revealed in patients with stable and unstable angina. When conducting RT sessions, patients with coronary artery disease should strictly adhere to the mode of exposure to the heart: frequency 5 Hz, exposure - no more than 5 minutes, contact, stable.
For patients with coronary artery disease, RT sessions are carried out strictly on the recommendation and under the supervision of a cardiologist. If RT has a favorable effect during treatment, the doctor may reduce the dosage of drugs after the 6th – 8th session.
Treatment regimen for coronary artery disease and angina pectoris
Laser treatment areas: 4th intercostal space to the left of the edge of the sternum, carotid artery, gallbladder projection. Laser procedures should be performed on trigger zones of the shoulder, forearm and direct projection of the heart.
The course of treatment consists of 7-15 sessions, one per day or every other day. The number of sessions is directly related to the severity of the patient’s condition and the functional class of angina: FC I-II – 10-15 sessions, FC III-IV – 7-10 sessions. Repeated courses - the second and third - are recommended to be carried out 3-4 weeks after the end of the previous one.
A preventive course for ischemic heart disease is recommended to be carried out 2-4 times a year. The use of laser therapy in the treatment of cardiac patients gives a positive therapeutic effect.
Diseases of the heart and blood vessels treated with laser
The laser therapy method is intensively and purposefully used in cardiology, as it has a wide range of effects on blood vessels and the heart.
In our department, laser therapy is used for the following vascular and cardiac pathologies:
- Coronary heart disease (acute, chronic)
- Angina pectoris
- Vegetative-vascular dystonia
- Hypertonic disease
- Atherosclerosis
- Arrhythmias
- Peripheral vascular diseases
Only a department specialist can prescribe laser irradiation. To determine exactly how much laser exposure is required for your specific case, the department uses special technology that can measure certain parameters of red blood cells.
In case of IHD in the chronic or acute stage, the effect of laser irradiation is multicomponent. Thanks to laser therapy, the ischemic area decreases and the heart’s resistance to hypoxia increases. Laser irradiation relieves heart pain and normalizes arrhythmias. The dosage of antianginal drugs after a laser course can be reduced. Attacks of angina become less frequent, and sometimes stop completely, the speed of blood circulation increases, as does the contractility of the heart, which leads to the restoration of the functions of the heart muscle.
Drug treatment for hypertension mostly removes the external manifestations of the disease, without eliminating its cause. After laser therapy sessions, the blood carries and binds oxygen much better, so much more of it enters the heart and brain than usual. The use of a laser to treat hypertension significantly improves the patient’s condition: headaches appear less frequently or disappear, dizziness and discomfort in the heart area may also cease. Blood pressure indicators change significantly for the better, which makes it possible to reduce the number of antihypertensive drugs.
In the case of atherosclerosis, laser irradiation normalizes blood clotting, which can prevent the formation of blood clots in blood vessels. The laser also affects smooth vascular muscles, so blood flow increases, more oxygen enters the tissues, all metabolic processes are normalized, ischemia is reduced, heart pain goes away, and damaged vessels are restored. Atherosclerotic processes leading to vascular damage are inhibited.
Non-invasive low-intensity laser therapy is effective for angina pectoris: it produces an antianginal effect, after the procedures the doses of special medications are usually reduced.
Laser therapy is an excellent way to prevent strokes and heart attacks.
The vessels are cleansed of cholesterol deposits, strength and elasticity return to them, and blood flow is normalized.
High technologies in the treatment of cardiac arrhythmias
Republican Scientific and Practical Center "Cardiology"
D. Goncharik, leading researcher at the laboratory of cardiac arrhythmias, candidate of medical sciences, associate professor
Irregular or fast beating of the heart is called arrhythmia. There are many different types of arrhythmias - from the usually harmless atrial extrasystoles to the truly life-threatening paroxysms of rapid ventricular tachycardia. An episode of acute rapid heartbeat is called paroxysm. Many arrhythmias can respond well to treatment with medications or disappear with rest (vacation), reducing alcohol consumption, caffeine, and quitting smoking.
*****
However, in some patients, arrhythmias occur so frequently that they interfere with normal life or cannot be treated with medications. In such cases, modern cardiology has a wide arsenal of highly effective minimally invasive and surgical treatment methods. “Minimally invasive” means that elimination of arrhythmia is achieved using special catheters that are inserted into the heart through the vessels of the legs, without cutting the chest, and the patient is conscious only under local anesthesia, without experiencing pain.
This procedure is called ablation, a complex, high-tech heart surgery. On average it takes several hours. Such minimally invasive operations are the most effective method of treating heart rhythm disorders, as they allow patients to completely get rid of arrhythmia.
First, several catheters are inserted into the patient through the veins and/or artery of the thigh under local anesthesia - thin wires that make it possible to record an electrocardiogram of the heart directly from the inside. This is necessary to correctly establish the diagnosis and further treatment tactics. The doctor can control the movement of the catheter tip inside the patient's body using a special device. Such intracardiac cardiograms, recorded from several points, make it possible to most accurately diagnose arrhythmia and determine its source.
After the doctor determines the point in the heart that is responsible for the arrhythmia, it can be eliminated using a special ablation catheter. An ablation catheter differs from other catheters inserted into the heart in that its tip can heat up to 45 - 60 C and “cauterize” the source of the arrhythmia.
All ablations have some risks, although they are usually not particularly dangerous. Fortunately, complications occur in only about 1% of patients. The most common types of arrhythmias that can be successfully treated with catheter ablation in a single procedure are atrioventricular nodal and some other atrial tachycardias, atrial flutter and fibrillation, WPW, and some types of ventricular tachycardias. Unfortunately, not all types of arrhythmias can be successfully eliminated using modern treatment methods, but science and technology do not stand still and new technologies are being introduced every year.
*****
One of the most common types of tachycardia (fast heartbeat) in young people is atrioventricular nodal paroxysmal tachycardia. With such an arry inside the atrioventricular node (connection). To prevent repeated paroxysms of tachycardia, prophylactic administration of special medications may be required. However, most patients do not want to take medications for a long time: they stop taking them or take them irregularly, so attacks of arrhythmia recur. Lasting recovery of patients suffering from such tachycardia can be achieved by cauterization (ablation). To do this, it is necessary to cauterize a small area in the atria in the area of the AV junction and thus break the ring along which the arrhythmia “runs.” After this, it completely disappears and the patient feels like a completely healthy person.
Another arrhythmia that often requires calling an ambulance is arrhythmia in patients with Wolff-Parkinson-White syndrome (or WPW syndrome). WPW syndrome is a congenital defect—an additional abnormal conduction pathway (besides the normal atrioventricular junction) through which impulses can also travel from the atria to the ventricles and vice versa, causing severe cardiac arrhythmias. Some of these arrhythmias can be truly life-threatening.
Patients with WPW syndrome often require special medications to prevent heart rhythm disturbances. It should be noted that although medications can usually provide some control of arrhythmia attacks, complete resolution of symptoms cannot be achieved with medications alone. Therefore, many doctors recommend catheter ablation as the best treatment method.
It is often difficult to localize this additional pathway, but modern computer equipment can significantly increase the efficiency of operations.
One of the most common cardiac arrhythmias in middle-aged and elderly people is atrial fibrillation. In atrial fibrillation (AF), the upper chambers (atria) of the heart contract chaotically and uncoordinatedly (fibrillate) at a rate of approximately 400 times per minute. This chaotic heart rhythm has an adverse effect on the heart, which ultimately leads to the formation of heart failure.
In most cases, patients experience palpitations, dizziness, shortness of breath and fatigue. For some, atrial fibrillation is completely asymptomatic. The tricky thing about atrial fibrillation is that it can cause strokes.
A new episode of arrhythmia is called paroxysm. When AF paroxysm persists for a long time, blood clots (thrombi) can form in the atria, which travel through the bloodstream into the arteries and cause their blockage. The area of tissue that does not receive oxygenated blood dies. The most dangerous is the entry of blood clots into the arteries of the brain, which is accompanied by a stroke. To prevent strokes, patients must take blood thinners such as aspirin or warfarin.
Restoring the rhythm in a patient with atrial fibrillation can be achieved with pills or intravenous medications, or with an electrical shock (electrical shock therapy).
It is extremely important not to delay restoring the rhythm, because if paroxysm persists for a long time, this can be difficult. For example, if a patient's paroxysmal AF persists for more than 48 hours, clots may form in the heart. Before restoring the rhythm, the doctor must make sure that the patient does not have thrombi (blood clots) in the cavities of the heart. For this purpose, transesophageal echocardiography (ultrasound of the heart using a probe similar to a gastric tube) is performed or the drug warfarin is prescribed for 3 to 4 weeks immediately before the cardioversion procedure to thin the blood.
Although electrical cardioversion can restore normal heart rhythm in approximately 90% of patients, unfortunately, in a significant proportion of patients, the rhythm is re-disturbed within a year for various reasons. If AF recurs repeatedly, the doctor decides whether it is advisable to restore the rhythm again in a particular situation or whether it makes sense to transfer AF to a permanent (chronic) form.
Some patients cannot maintain rhythm with medication. There are modern surgical and minimally invasive treatment methods for them.
*****
The labyrinth type surgery is performed under general anesthesia while the heart is stopped. The right and left atria are cut with a scalpel and then stitched together. In this way, it is possible to form a normal “path” for the propagation of a normal rhythm from the atria to the ventricles. However, this operation is complex and requires cutting into the chest.
Physicians with experience in treating cardiac arrhythmias are constantly developing new methods to identify the sources of arrhythmia without cutting into the chest (mapping) or cauterizing the sources of atrial fibrillation so that AFib disappears once and for all.
The mapping and cauterization procedure has been in use since the late 1990s, with new variations being introduced every year. During the ablation procedure, doctors use special catheters to eliminate the sources of arrhythmia in the atria, and if there are too many such areas, they “isolate” them from healthy heart tissue by drawing circular ablation lines. This is a rather complex and lengthy procedure, lasting several hours. Sometimes it is carried out in several stages. The advantage of this invasive operation is that it is performed under local anesthesia; the patient is conscious, there is no need to cut the chest.
Currently, the best results are achieved using a special catheter navigation system inside the heart cavity (CARTO system), which allows you to control the catheter that cauterizes arrhythmia inside the heart cavities with an accuracy of 1 mm. This catheter allows you to build a map of arrhythmia.
The procedure is more effective for patients with frequent short paroxysms of AF; the effectiveness against long-standing AF is significantly lower.
The AF ablation procedure is not without risks. About 2 to 3% of patients experience serious complications such as blood leaking into the heart (tamponade), strokes, nerve damage, narrowing of the pulmonary veins, or a hole forming between the atria and esophagus (atrioesophageal fistula). Many of these complications are treatable but require the patient to remain in the clinic for an extended period of time.
Therefore, to decide on the advisability of a procedure, the doctor weighs the potential benefits and possible risks for a particular patient, choosing the optimal solution for the given case at the time.
*****
Atrial flutter is often an arrhythmia related to atrial fibrillation, in which the atria contract at a high rate of up to 200 to 300 beats per minute, and this rapid rhythm is conducted to the ventricles and causes them to contract at a rate of 100 to 150 beats per minute. This leads to rapid disruption of the normal pumping function of the heart. Treatment of atrial flutter with medications is usually ineffective.
The best treatment for atrial flutter is ablation (cauterization), which produces positive results in approximately 90% of patients.
Excessively fast heartbeats that originate from the heart's ventricles are called ventricular tachycardia (VT). This arrhythmia often poses a serious threat to the patient's life, often leads to loss of consciousness and requires the use of special medications, the use of invasive (catheter ablation) or even surgical treatments.
Typically, severe ventricular tachycardia is treated by sewing a special device under the skin - an implantable cardioverter-defibrillator (ICD), which allows you to interrupt severe attacks of arrhythmia using an electrical discharge from the inside.
Some forms of ventricular tachycardia are less life-threatening and occur in people with nearly normal heart function. Although these forms of the disease can be treated with medications, a permanent cure can be achieved with the help of an ablation procedure and save the patient from repeated breakdowns once and for all. Sophisticated computer systems make it possible to create a map of cardiac excitation during such tachycardia, which makes it possible to identify its source.
Often, a paroxysm of ventricular tachycardia develops into an even more severe arrhythmia - ventricular fibrillation (VF), in which the heart contracts uncoordinatedly at such a high speed that it is unable to pump blood, and this is tantamount to cardiac arrest. With ventricular fibrillation, a person always loses consciousness.
There are many causes of VT and VF, but most often it occurs due to disruption of the blood supply to the heart muscle due to narrowing of the coronary arteries or the presence of scars in the heart muscle. The most effective means of stopping repeated paroxysms of ventricular fibrillation (rhythm restoration) are implantable cardioverter defibrillators (ICDs).
An ICD is an implantable device (similar to a pacemaker) that monitors the heart's rhythm. Unlike a pacemaker (which prevents the heart from beating too slowly), an ICD can also detect and interrupt excessively fast heartbeats - ventricular tachycardia, as well as ventricular fibrillation. If a severe arrhythmia occurs, the cardioverter-defibrillator commands the restoration of the normal rhythm (using a series of rapid electrical impulses or an electrical discharge from the inside). Information about each episode can be downloaded using the programmer and can be read from the ICD memory without cutting the skin. The clinic of the Republican Scientific and Practical Center "Cardiology" has sufficient experience in treating such patients.
In general, the lives of patients with ICDs are almost no different from the lives of other people. Although ICDs successfully treat VT and VF but do not prevent them, patients should avoid situations where they might lose consciousness in a life-threatening situation, such as during unaccompanied swimming, etc. If the patient is touched by another person at the time of the shock, You may feel a slight, momentary tingling sensation, but it poses absolutely no danger. Modern ICDs last for four to six years before the generator needs to be replaced.
Electrical system of the heart
The heart has its own electrical (conducting) system, consisting of an electrical impulse generator - the main pacemaker (sinus node) - and conduction pathways (atrioventricular junction, His bundle and its branches) connecting the entire electrical circuit. The main pacemaker (sinus node), located in the right atrium, generates regular electrical impulses at a certain frequency, like a metronome. In response to each impulse, the heart contracts in a strict sequence - first the atria, then normally through a single connection (atrioventricular, in which its short-term delay occurs), the impulse passes to the ventricles, spreading through the system of fibers, causing the ventricles to contract synchronously.
Bradycardia and pacing
At rest, our heart beats at approximately 50 to 90 beats per minute, although athletes and patients taking certain medications, such as beta blockers, may contract slower. Heart rate increases during exercise, and the maximum varies greatly among individuals.
A slow heartbeat (bradycardia) may cause no symptoms or may cause dizziness, blurred vision, shortness of breath, or fatigue. Bradycardia can occur due to problems with the main pacemaker of the heart (sick sinus syndrome) or a delay in the impulse at the atrioventricular junction (heart block).
Patients with high-grade heart block and sick sinus syndrome usually have a pacemaker fitted.
Pacemakers
A pacemaker is an implanted device that monitors a person's heartbeat and prevents the heart from beating too slowly.
It consists of a “pulse generator” (the pacemaker itself) to which one or two wires (electrodes) are attached. Typically, the pacemaker is placed under the skin or in the muscle just below the collarbone. Almost all modern pacemakers work “on demand”, that is, they turn on only when necessary - when the heartbeat is too slow to set the correct rhythm. The rest of the time, the device only monitors the patient’s own heart rhythm without interfering with its work.
There are many different types of pacemakers available today. Belarusian clinics have all the necessary types. There are physiological pacemakers: they can recognize when the patient is sleeping or, conversely, doing hard work. In response to exercise (fast walking or running), the stimulator increases the heart rate, and at night, on the contrary, it works even slower than during the day at rest.
The service life of modern pacemakers under standard conditions is approximately 7 - 10 years, but can be much longer for a particular patient. The expiration date of the pacemaker battery can be easily predicted during the next scheduled check of the pacemaker.
The pacemaker imposes almost no restrictions on the patient's daily life. Household appliances and mobile phones do not interfere with the operation of the device, although you should not store a mobile phone in a pocket near a pacemaker.
Heart failure
With severe damage to the heart by various diseases, its pumping function gradually decreases. When the pumping function is significantly reduced, the heart is unable to pump the required amount of blood, which is called heart failure.
Most cases of heart failure are caused by the fact that the main pumping chamber of the heart (the left ventricle) cannot contract with sufficient force, but usually the right and left ventricles continue to contract synchronously (almost simultaneously).
Resynchronizing pacemaker
As heart failure increases, the right and left ventricles begin to contract at the same time - the contraction of the left ventricle or part of it is greatly delayed in relation to the right ventricle. Asynchronous contraction further reduces the efficiency of the heart's pumping function. To treat such patients, special stimulants are used. The goal of cardiac resynchronization therapy (CRT) is to stimulate the ventricles so that they contract simultaneously, thereby improving the pumping function of the heart.
In general, the implantation procedure is similar to the procedure for implanting a conventional pacemaker. The only difference is that an additional electrode is inserted to set the correct rhythm to the left ventricle and synchronize the work of the right and left ventricles.
Currently, implantation of pacemakers, including physiological ones, is performed in all regional centers of Belarus. Implantation of more complex devices - resynchronizing pacemakers and cardioverter-defibrillators - is carried out in the republic.
It is important!
Attacks of dizziness and loss of consciousness
Approximately 30 - 50% of people experience fainting or blackout at some point in their lives. Fainting occurs for a variety of reasons, but the immediate common cause is usually a sudden drop in blood pressure, which in turn leads to a short-term reduction in blood flow and oxygen delivery to the brain.
Usually, but not always, a person immediately before losing consciousness feels lightheaded or dizzy, and also complains of darkening of the eyes and ringing in the ears. In addition, nausea, vomiting, sweating, and rapid or slow heartbeat may occur.
Fainting among people of all ages is so common that many do not immediately perceive it as a serious threat to life and may seek professional help from a doctor only after a series of fainting spells, which is a mistake.
The most common type of fainting is due to improper reflex interaction between the cardiovascular and nervous systems, as a result of which the cardiovascular system selects a heart rate and degree of relaxation of the body’s blood vessels that is inadequate to the current situation. In addition to the so-called functional, or “reflex” forms of fainting, patients may also lose consciousness due to organic heart diseases: excessively fast or slow heartbeat, dysfunction of the heart muscle or heart valves, as well as diseases of the nervous system and overdose of drugs that lower blood pressure. Differential diagnosis usually requires an electrocardiogram, as well as an ultrasound scan of the heart or “echocardiogram”, etc.
Doctors may recommend that patients who complain of recurrent “reflex” fainting avoid certain situations that lead to fainting (for example, standing up on a crowded train in hot weather), wear medicated compression stockings, prescribe certain medications, and in some cases, get a pacemaker. if such fainting is accompanied by an excessive slowing of the heart rate.
To diagnose disease of the heart muscle and/or heart valves, certain non-invasive tests are available, such as 24-hour continuous recording of heart rate and rhythm using an ECG (Holter ECG monitoring). In some cases, invasive tests may be required, such as coronary angiography (cardiac catheterization) and/or specialized tests of the heart's electrical system, known as an electrophysiological study, or EPS.
In patients suffering from organic heart muscle disease, fainting often occurs due to an excessively fast heartbeat. In such a situation, the heart simply does not have time to emit the amount of blood necessary to ensure normal functioning of the brain, and the doctor may raise the question of a special heart operation to eliminate or cauterize the source of such arrhythmia. In some cases, it may be decided to implant a special device under the skin, similar to a pacemaker, which will restore excessively fast heartbeats using an electrical current discharge from the inside (ICD).
The main thing is that if fainting occurs, you should not wait for it to recur many times (since the second or third may already be the last), but quickly seek help from a specialist.
General multicomponent effect of laser therapy
In general, the effect on the heart and blood vessels when using laser irradiation consists of the following improvements:
- Relieving spasms
- Expansion and strengthening of blood vessels
- Improving blood microcirculation
- Reducing blood viscosity and increasing coagulability (the risk of blood clots is reduced, and microthrombi are resolved)
- Increased hematopoiesis
- Normalizes heart rate and reduces the likelihood of arrhythmias
- Increased cardiac contractile function
- Reduction in blood cholesterol, normalization of many blood parameters
- Increasing the bactericidal properties of bloodReducing ischemic zones
- Improving oxygen metabolism
- Increased oxygen content in tissues
Indications and contraindications for laser therapy
Indications for the procedure are as follows: vegetative-vascular dystonia, neurocirculatory dystonia, hypertension, ischemia, angina pectoris class I-IV, cardiomyopathy, post-infarction condition, myocarditis, myocardial dystrophy, arrhythmia, consequences of cerebrovascular accident, vertebrobasilar insufficiency, discirculatory encephalopathy, atherosclerosis of the lower extremity vessels, obliterating endarteritis , venous insufficiency, varicose veins of the lower extremities, hemorrhoids, Raynaud's syndrome.
Contraindications are common to physiotherapeutic factors: blood diseases with bleeding syndrome, severe thrombocytopenia, deep vein thrombosis, menstruation, severe hypotension, the presence of an implanted pacemaker and pacemaker.
Academician E.M. made a great contribution to the development of low-intensity laser technologies in medicine. Meshalkin, who first introduced the technique of intravenous laser irradiation of blood into the complex treatment of patients with coronary heart disease in 1980. Currently, experts give preference to supravenous laser blood irradiation - NLBI, which gives a pronounced clinical effect in complex therapy for patients with cardiovascular insufficiency.
Contraindications to laser irradiation
The innovative laser method for treating blood vessels and the heart also has its contraindications. These include:
- Pregnancy.
- Chronic diseases of internal organs, if they are exacerbated.
- Certain blood diseases.
- Malignant neoplasms.
- Benign progressive formations.
- Active tuberculosis.
- Thrombophlebitis.
- Some blood diseases.
- Individual intolerance to light therapy.
- Anemia with a hemoglobin value less than 80 is a temporary contraindication.
How a laser therapy session is performed
- The doctor will ask you to sit or lie down.
- The area that will be exposed to radiation must be free of clothing.
- Laser therapy will be performed either remotely (at a distance from the skin from ½ meter to a meter) or contact (the light guide is pressed to the skin, the penetration depth of the azure waves is much greater).
- The department also practices intravascular laser therapy, in which a needle equipped with a disposable light guide is inserted into a vein. Often used for ischemic heart disease.
- There are usually no discomforts during laser procedures.
- The doctor monitors the laser radiation parameters and your condition during the session.
The specialists of the department select all radiation characteristics individually for each specific case. You will be prescribed treatment tactics, determine the localization of the effect, the number of procedures, and the duration of the session.
Laser therapy, a high-tech method of treating lesions of the heart and blood vessels, has been successfully used in our department for a long time. If you have chronic damage to the heart or blood vessels, our experts recommend laser therapy sessions once or twice a year. The therapeutic effect of the technique is extremely high.
What is NLOC and how does it work?
The NLBI technique is simple and accessible. It is also characterized by non-invasiveness, sterility, painlessness, lack of damaging effects on the blood and vessel walls, and no need for disposable infusion systems or light guides.
NLBI activates the circulatory and microcirculation systems, stimulates hematopoiesis, improves the rheological properties of blood and lipid peroxidation, helps reduce cholesterol in the blood, saturates cells and tissues with oxygen, corrects immunity, has an analgesic, anti-inflammatory, and anti-edematous effect. Under the influence of laser radiation, blood viscosity decreases, bleeding and coagulation time lengthens, fibrinogen content, prothrombin index, plasma tolerance to heparin decrease, the level of endogenous heparin increases, and the fibrinolytic activity of the blood increases.
The NLBI technique is an effective means of preventing and treating a wide range of diseases. It can be prescribed as an independent method or as an addition to the main laser therapy treatment program. NLBI is performed on one pair of symmetrical veins. Preference is given to the pair located closest to the source of pathology or problem area.
The impact parameters for NLBI are as follows:
- As an independent method: frequency 5 or 50 Hz, exposure 5-10 minutes for each vein, contact technique (with slight compression), stable. 1st course of treatment: 8 sessions, 1 session per day. If necessary, the second and third courses of NLBI are carried out, the interval between courses is 1-3 months.
- As an addition to the main program: frequency 5 or 50 Hz, exposure 1-5 minutes for each vein, contact technique (with slight compression), stable. The course of treatment is 10 sessions, 1 session per day or for the entire course of the main program.
The number of sessions and courses is determined by the attending physician, based on the effectiveness of the results.