A stroke is a sudden disruption of cerebral circulation. Just a few years ago, this disease threatened, as a rule, only older people, but in recent years, the accelerated pace of life, a stressful environment and a deteriorating environmental situation have led to the fact that stroke is increasingly affecting young people. Ischemic stroke is considered an extremely dangerous pathology, since one of its consequences is disability and death. Specialists at the Neurology Clinic of the Yusupov Hospital provide timely, high-level medical care, which minimizes the risk of complications.
There are three stages of chronic cerebral ischemia:
- Stage 1 (initial) is characterized by a large number of various complaints of headache, irritability, insomnia, a feeling of “heaviness” in the head, decreased memory for immediate events, fatigue, poor coordination of movements, and instability when walking. These changes are not noticeable to others and patients remain adapted to society. A neurological examination reveals minimal symptoms, a clear neurological deficit has not yet formed, and adequate therapy can reduce or eliminate individual manifestations of the disease.
- Stage 2 (subcompensation) the frequency of complaints about loss of memory and performance, instability, and dizziness increases. A leading clinical syndrome is formed, and a neurological deficit becomes obvious. Cognitive, personality, and emotional-volitional disorders worsen. Adaptation to society and professional skills fade, but the possibility of self-care remains.
- Stage 3 (decompensation) Objective neurological disorders come to the fore. The number of complaints decreases due to decreased criticism of one’s condition. On examination, several well-defined neurological syndromes are noticeable. Cognitive impairments at the advanced stage of chronic cerebral ischemia are very often the leading cause of disability, their everyday adaptation suffers, patients are unable to work, require constant outside care, and vascular dementia develops.
In the clinic of chronic cerebral ischemia, several main neurological syndromes are distinguished. These include cephalgic, vestibulo-atactic, psychopathological, paroxysmal syndrome, pyramidal insufficiency, pseudobulbar syndrome.
Cephalgic syndrome is characterized by pain in various parts of the head. Often there is no connection between headaches and hemodynamic disorders. As chronic cerebral ischemia progresses, headache attacks become less frequent.
Vestibulo-atactic syndrome is one of the most common in patients with chronic cerebral ischemia. It includes vertigo, loss of coordination, instability, and noise in the head. These complaints arise from circulatory failure in the vertebrobasilar system, as well as age-related changes in the vestibular apparatus, ischemia of the vestibulocochlear nerve.
Paroxysmal disorders in chronic cerebral ischemia are varied and include episodes of transient global amnesia, syncope, drop attacks, and epileptic seizures. The severity of such conditions increases as ischemia and concomitant diseases progress.
Mental disorders are often present at all stages of chronic cerebral ischemia. At first, they are of the nature of asthenoneurotic, depressive, and anxiety disorders; at stages II-III, they are joined by cognitive impairment, and dementia occurs.
Symptoms of left-sided ischemic stroke
In accordance with the localization of the brain catastrophe in a particular part of the brain, a stroke can be right-hemisphere or left-hemisphere. The disease develops according to the principle of “reverse symmetry”: with a right hemisphere stroke, paralysis of the left side of the body develops, with a left hemisphere stroke, on the contrary, paralysis of the right side.
The hemispheres of the brain are responsible for different functions. The left is for language and thinking abilities, the right is for creative and emotional. In view of this, with a left hemisphere stroke, the patient experiences a speech disorder, which is manifested by slurred speech, difficulties with the coherent expression of one’s thoughts, and with understanding what is heard. With a right hemisphere stroke, these symptoms are usually absent, and therefore this form of stroke is much more difficult to recognize.
Most often, the main cause of vascular circulation disorders in the brain is blood clots. They arise due to hypertension and lead to blockage of the lumen of the vessel. In addition, pathology can be caused by diseases such as high blood viscosity, rapid clotting, disorders of the heart and blood vessels, metabolism, diabetes mellitus, and slow blood circulation. Very often, ischemic stroke affects those who have had a heart attack, surgery to install a heart valve, or suffer from frequent headaches and migraines.
Make an appointment
The majority of cases (up to 60%) occur in right hemisphere stroke. To diagnose it, it is necessary to take into account that this type of stroke affects the appearance of the left side of the face and the condition of the body. A left-sided stroke is manifested by disruption of the facial muscles on the left side: drooping of the corner of the mouth and the outer corner of the eye. Partial or complete paralysis of the left side of the body occurs. The function of internal organs located on the left side of the body may be impaired.
In addition, left-sided stroke is manifested by other symptoms:
- paralysis of the left eye;
- hearing impairment;
- impaired perception of the left side of the body: the limbs become disobedient, it is difficult to assess the distance from the limbs to objects or the size of the limb;
- the appearance of inexplicable aggression, inappropriate behavior, depression;
- inability to perceive colors.
- change in speech;
- disturbance of mental activity;
- memory loss;
- misunderstanding the meaning of words.
When a part of the brain located in the central part is damaged, as a rule, complete immobility of the limbs occurs. When the lesion is localized in the parietal region, the patient has difficulty perceiving heat, cold, and pain.
After confirming the diagnosis, it is important to provide first aid to the patient competently and promptly. The specialists at the Yusupov Hospital have extensive experience in treating strokes; thanks to their practical skills, it is possible to minimize the severe consequences of this disease.
Basic examinations in patients with chronic cerebral ischemia:
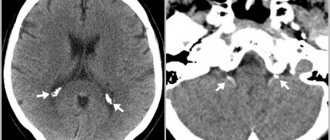
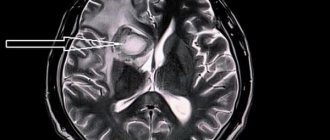
- MRI of the brain, preferably with angiography
- blood pressure and ECG monitoring.
- general blood test, general urinalysis, biochemical blood test, coagulogram, blood lipid spectrum.
- fundus examination
- examination by an otoneurologist
- neuropsychological study.
- CDK BCS, TKDG, ECHO-KG
- examination by a psychotherapist to identify anxiety-depressive conditions and cognitive deficits).
Treatment and prevention of chronic cerebral ischemia should be aimed at correcting the current vascular disease. The focus is on antihypertensive therapy, prevention of thrombosis, and lowering blood cholesterol levels. Also an important component of treatment is the correction of concomitant diseases (diabetes mellitus, heart rhythm disturbances, heart failure, obesity), sleep disorders and anxiety-depressive disorders. Vascular therapy, neuroprotection, and improvement of neurometabolism play a significant role. A comprehensive treatment is recommended, including non-drug methods of influence: psychotherapy, exercise therapy, massage, physiotherapeutic treatment.
The First Neurology clinic presents a variety of hardware techniques that help improve cerebral circulation, such as mesodiencephalic modulation (MDM therapy), brain micropolarization, and electrosleep. Using the modern CEFALY neurostimulation technique, the intensity of headaches decreases, memory and concentration improve.
Contraindications to magnetic resonance imaging
There are few contraindications to magnetic resonance imaging, but they do exist. These include:
- The presence of an implant in the body (including a pacemaker).
- Excessive mobility of the patient, for example, if he is intoxicated. During an MRI, the subject must lie still.
- Foreign objects in the body (during the examination they may move and damage blood vessels).
Relative contraindications include illness, children under 7 years of age, metal prosthetic joints outside the range of electromagnetic waves, blood diseases (in this case contrast cannot be used), severe claustrophobia (the patient’s condition may sharply worsen in a closed space).
Our specialists
Tarasova Svetlana Vitalievna
Expert No. 1 in the treatment of headaches and migraines. Head of the Center for the Treatment of Pain and Multiple Sclerosis.
Somnologist.
Epileptologist. Botulinum therapist. The doctor is a neurologist of the highest category. Physiotherapist. Doctor of Medical Sciences.
Experience: 23 years.Derevianko Leonid Sergeevich
Head of the Center for Diagnostics and Treatment of Sleep Disorders.
The doctor is a neurologist of the highest category. Vertebrologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 23 years.
Palagin Maxim Anatolievich
The doctor is a neurologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 6 years.
Romanova Tatyana Alexandrovna
Pediatric neurologist. Experience: 24 years.
Temina Lyudmila Borisovna
Pediatric neurologist of the highest category. Candidate of Medical Sciences.
Experience: 46 years.
Zhuravleva Nadezhda Vladimirovna
Head of the center for diagnosis and treatment of myasthenia gravis.
The doctor is a neurologist of the highest category. Physiotherapist. Experience: 16 years.
Mizonov Sergey Vladimirovich
The doctor is a neurologist. Chiropractor. Osteopath. Physiotherapist. Experience: 8 years.
Bezgina Elena Vladimirovna
The doctor is a neurologist of the highest category. Botulinum therapist. Physiotherapist. Experience: 24 years.
Drozdova Lyubov Vladimirovna
The doctor is a neurologist. Vertebroneurologist. Ozone therapist. Physiotherapist. Experience: 17 years.
Read also
Swelling of the legs
Causes of Swelling in the Legs The legs are common sites for swelling due to the effect of gravity on the fluids in the human body.
However, fluid retention is not the only cause of leg swelling. Injuries… Read more
Transient ischemic attack (TIA)
What it is? Why is this happening? Is this condition dangerous? What to do if doctors make such a diagnosis? These questions are always asked by patients who come to see a neurologist. According to classification...
More details
Hemorrhagic stroke
Hemorrhagic stroke is a type of acute cerebrovascular accident, which is characterized by the effusion of blood into the brain substance with the development of neurological deficit, often leading...
More details
Atherosclerosis
What is atherosclerosis Atherosclerosis is a narrowing of the arteries caused by the formation of plaque. As a person gets older, fat and cholesterol can accumulate in the arteries and form plaque. Accumulation…
More details
Encephalopathy
These can range from minor abnormalities in brain function to serious neurological disorders that require urgent treatment. Encephalopathy can be congenital or acquired. Congenital...
More details
Gliosis: causes and mechanisms of development
Glial tissue is one of three types of brain tissue (along with neuronal and ependymal), which is essentially connective tissue; normally it makes up about 40% of the brain volume.
Its function is to preserve the very structure of the brain, ensure the supply of nutrients to the main cells of the brain - neurons, as well as physically protect neurons and give them a certain position. As neurons die from natural or pathological causes, they are replaced by glial tissue. Gliosis is the pathological proliferation of glial tissue, the appearance of large single or multiple foci of connective tissue (they look like scars) in the structures of the brain. Gliosis cells, although they replace dead neuron cells, cannot fully perform their functions, therefore, as a result of a lack of mechanisms for transmitting nerve impulses, neurological symptoms develop. The appearance of gliosis foci leads to disruption of the normal functioning of the brain - the patient’s attention and memory weaken, mental processes are disrupted, speech and movements become uncertain.
Such disorders are inevitable as a result of the natural aging of the body, but there are cases of premature pathological growth of glial foci in the brain structures of young and middle-aged people. In extremely rare cases, a person may experience congenital replacement of neurons with glial cells.
The nature of the occurrence of gliosis changes in the brain can be different. Brain diseases such as epilepsy, encephalitis, multiple sclerosis can lead to accelerated death of neurons and proliferation of connective tissue; vascular disorders, hypertension, anemia, trauma and cerebral edema can also cause gliosis. Provoking factors are: heredity, old age, excessive consumption of fatty foods and poor lifestyle in general.