Causes
Pregnancy is a risk factor for heart rhythm disturbances. There are explanations for this:
- Hormonal changes. The natural increase in progesterone and estrogen has a proarrhythmic effect on myocardial tissue.
- Increase in circulating blood volume by 20-30%. This leads to stretching of the atria, and the rhythm is disrupted.
- Physiological increase in heart rate. On average, heart rate increases by 15-20 beats per minute compared to the initial data. Against the background of natural tachycardia, cardiac output increases and arrhythmia develops.
Heart rhythm disturbances are detected in 10-12% of all pregnant women (according to some authors - up to 20%). The prevalence of pathology among expectant mothers is higher than among women outside the gestational period. Arrhythmia may be newly identified or formed before conception. Often the exact cause cannot be determined.
It is important to understand: not all heart rhythm disturbances in pregnant women are associated with organic damage to the myocardium. In practice, we often see that failure of the heart is caused by various conditions, including endocrine pathology, diseases of the nervous system, etc. The medical literature indicates that up to 45% of gestational arrhythmias are of functional origin and occur even in healthy women.
The following causes of arrhythmia are distinguished:
- functional states: consumption of certain products (tea, coffee), smoking, stress, physical activity;
- organic damage to the heart muscle: ischemic heart disease, heart defects, myocarditis, pericarditis, neoplasms;
- autoimmune diseases;
- bronchial asthma, bronchitis;
- cerebrovascular accident;
- pathology of the thyroid gland, adrenal glands;
- intoxication with alcohol, drugs.
Arrhythmia in pregnant women often develops when carrying a large fetus, multiple pregnancy, and polyhydramnios.
During pregnancy, both mother and fetus may experience a variety of rhythm disturbances. They represent a serious medical problem for a number of reasons. Firstly, arrhythmias themselves can pose a threat to the health and life of a pregnant woman and fetus. Secondly, the frequency of arrhythmias during pregnancy increases, which is due to significant physiological changes in the mother’s body [1]. Thirdly, these changes affect the pharmacokinetic parameters of drugs, and, consequently, their blood concentrations, effectiveness and safety. Finally, antiarrhythmic drugs can have adverse effects on the fetus, including teratogenicity.
In general, the management of arrhythmias during pregnancy does not differ significantly from that in non-pregnant women [2]. However, if arrhythmia develops in a pregnant woman, it is necessary to weigh its severity, the threat to the health of the mother and fetus, and the risk of undesirable effects of drug therapy. Doctors of different specialties - cardiologists, obstetricians and pediatricians - should decide on the choice of treatment for a pregnant woman. The type of therapeutic intervention is determined, first of all, by hemodynamic disorders in the mother and fetus. Women without structural heart defects and with minor clinical symptoms of arrhythmias (for example, atrial and ventricular premature beats) should not be prescribed drug therapy, but they should exclude possible precipitating factors such as smoking, coffee and alcohol. In cases where the arrhythmia is well tolerated, non-pharmacological treatments can be used.
Non-pharmacological treatments for arrhythmias
Non-pharmacological treatments include observation, rest and stimulation of the vagal reflexes, for example by carotid sinus massage [3]. There is successful experience of using electrocardioversion in pregnant women [4,5]. During cardioversion, arrhythmias in the fetus have been observed in rare cases, so it is recommended to perform it under the control of its cardiac activity [6]. However, the likelihood of developing arrhythmias in the fetus is quite small, firstly, due to the high threshold of fibrillation and, secondly, due to the fact that the uterus is located outside the shock vector zone and therefore receives a relatively small electrical stimulus [7].
In contrast, there is little experience with implanting defibrillators in pregnant women. Available data do not suggest that the use of defibrillators is associated with a high risk of complications [4]. Implantation of a defibrillator may be an option for women with life-threatening arrhythmias who are planning repeat pregnancies and in whom the use of toxic drugs is undesirable [7].
In the event of cardiac arrest in a pregnant woman, resuscitation measures do not differ from those in non-pregnant women, but the possibility of compression of the aorta and inferior vena cava by the uterus should be taken into account. Resuscitation measures are recommended to be carried out with the woman lying on her side or by manually moving the uterus to the head end and to the left. If the pregnancy is more than 25 weeks, a caesarean section should be performed immediately [7].
General principles for choosing antiarrhythmic drugs during pregnancy
If it is necessary to prescribe antiarrhythmic drugs, the choice of a specific drug should be based on currently available information about its therapeutic effectiveness and safety, taking into account the age of the fetus (gestational age). In this case, the safety of the drug should be taken into account not only for the fetus, but also for the mother. Moreover, when deciding whether to prescribe drug therapy, one must be guided by the following principle: a woman, regardless of pregnancy, should always receive optimal treatment [8]. When there are no alternatives, a drug that can help the mother is prescribed, regardless of its toxicity and potential harm to the fetus. However, to prevent adverse effects in the fetus as much as possible, careful monitoring of treatment is necessary. In cases where there is a choice, preference should be given to the most studied drugs that have proven to be safe for the fetus when widely used in medical practice. In general, the amount of information on the safety of individual drugs is proportional to the time they are on the global pharmaceutical market.
Most antiarrhythmic drugs are relatively safe during pregnancy, but all can cause adverse effects on the mother and fetus. There are serious exceptions to this rule. Treatment of pregnant women should begin with the minimum recommended dose, followed by its correction based on clinical symptoms, electrophysiological parameters and monitoring data of drug concentrations in the blood [8]. During pregnancy, the need for further drug therapy should be regularly assessed. One of the most important side effects of antiarrhythmic drugs in the mother is the proarrhythmic effect, which can be caused by almost all class II and III drugs [7].
Knowledge of the physiological changes that occur during pregnancy in the mother’s body is necessary, first of all, from the point of view of adjusting the doses of antiarrhythmic drugs*. Particular attention should be paid to the increase in intravascular volume (approximately 40-50%), which may necessitate an increase in the loading dose of the drug to achieve adequate therapeutic blood concentrations. In addition, it entails a decrease in protein levels in the blood plasma and a drop in the total concentration of the drug in the blood, although the concentration of the unbound active fraction may be normal. Therefore, monitoring antiarrhythmic drug concentrations in pregnant women is a less reliable means of monitoring therapy than clinical and electrophysiological response.
Sometimes antiarrhythmic drugs are prescribed to treat fetal arrhythmias rather than maternal arrhythmias. In these cases, their doses should be selected in such a way as to provide a therapeutic effect in the fetus without causing proarrhythmic effects or other undesirable effects in the mother.
Safety of antiarrhythmic drugs
Class I drugs
Among Class I A drugs, the greatest amount of data regarding safety during pregnancy is available for quinidine. During more than 60 years of its presence in the global pharmaceutical market, experience has been accumulated in the use of the drug for the treatment of arrhythmias in both pregnant women and the fetus [2]. Possible maternal side effects of quinidine include gastrointestinal disturbances, blood dyscrasias, and hearing and vision problems [2]. Spontaneous uterine contractions under the influence of quinidine have been described [9], but this complication is extremely rare. In general, quinidine is quite safe for the fetus. Isolated cases of thrombocytopenia and damage to the VIII pair of cranial nerves were observed mainly when average therapeutic doses were exceeded [10].
For procainamide, quite a lot of experience has also been accumulated in its use during pregnancy. It has also proven itself to be a fairly safe drug. When using the drug in the first trimester of pregnancy, no teratogenic effects were observed [11]. Experience with the use of procainamide shows that with a relatively short duration of treatment, the profile of its adverse reactions is quite favorable. Lupus syndrome usually develops with long-term treatment [12]. In addition, the advantage of procainamide over quinindine is the possibility of intravenous administration. Procainamide is considered as one of the drugs of choice for the treatment of tachycardia with a wide QRS complex [13]. In pregnant women, procainamide has gained a reputation as one of the most optimal antiarrhythmic drugs. Its doses may require adjustment at different stages of pregnancy.
Disopyramide, unlike the previous two drugs, has been poorly studied in pregnant women, so its use should be avoided. There is a report of the development of painful uterine contractions and sudden bleeding in a 26-year-old woman with Wolff-Parkinson-White syndrome when the drug was administered in the third trimester of pregnancy [14].
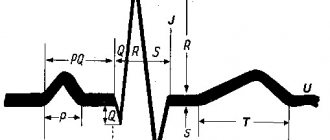
When treated with any class I A drug, there is a risk of potentially fatal ventricular arrhythmias (torsade de pointes), which are accompanied by prolongation of the QT interval on the ECG, and they are observed more often in women than in men [15]. All drugs in this class should be used in a hospital setting under constant monitoring of cardiac function and serum concentrations.
Class IB drugs include lidocaine, mexiletine, tocainide, moricizine, and phenytoin. There is quite a lot of experience with the use of lidocaine during pregnancy, but it mainly concerns its use as an anesthetic during childbirth. The drug was used much less frequently for the treatment of arrhythmias in pregnant women. Available experimental data and clinical experience suggest that lidocaine is well tolerated by mother and fetus [12,16]. The incidence of congenital anomalies did not increase with its use [17].
When using lidocaine, isolated toxic reactions in the fetus have been described [2]. Its administration is recommended to be avoided during prolonged labor and fetal distress. Lidocaine blood concentrations may increase in cases of fetal acidosis, leading to the development of toxic reactions from the heart and central nervous system [18]. Lidocaine is metabolized in the liver, so women with impaired liver function and heart failure should reduce its loading and maintenance doses.
Mexiletine is structurally similar to lidocaine. There is much less experience with its use during pregnancy, but it also appears to be a fairly safe drug [19].
Phenytoin is an anticonvulsant. Previously, it was widely used to treat arrhythmias that occur during intoxication with cardiac glycosides. In recent decades, due to the emergence of safer alternatives (beta-blockers, specific antibodies to digoxin and lidocaine), it has extremely limited value as an antiarrhythmic agent. Phenytoin is classified by the FDA as Category D* and should not be used during pregnancy if possible. Its use in the first trimester is especially dangerous, as it has a high teratogenic potential**. Some anomalies are observed in 30% of children exposed to phenytoin in utero, and full-blown “hydantoin” syndrome is observed in 10% [20]. Fruits with low microsomal epoxide hydrolase activity are at greatest risk [21]. Recently, it was shown that phenytoin, which has a membrane-stabilizing effect, can influence sodium and potassium channels in the myocardium [22]. It is possible that it causes bradycardia or arrhythmia in the fetus, leading to hypoxia, which, in turn, causes intrauterine growth retardation or death. Episodes of severe hypoxia produce highly reactive free radicals, causing orofacial clefts and shortening of the distal phalanges. Changes in blood flow and blood pressure resulting from cardiac dysfunction can lead to the development of cardiovascular damage.
In addition, phenytoin may have adverse effects on the development of the child. There is evidence that in persons exposed to phenytoin in utero, impairment of certain aspects of cognitive function is determined not only in childhood, but also in adulthood [23]. However, short-term use of the drug, especially in the second and third trimesters, is relatively safe [12]. In pregnant women, it is considered as an alternative treatment for arrhythmia caused by intoxication with cardiac glycosides, in case of ineffectiveness of safer antiarrhythmics [12].
It is recommended to avoid the use of tocainide and moricizine during pregnancy due to the lack of information about their safety [7].
Class IC drugs propafenone and flecainide are well tolerated by pregnant women and the fetus. Flecainide penetrates well through the placental barrier, especially in the third trimester of pregnancy [24,25], but its concentrations in fetal blood are lower than in amniotic fluid [24]. With its use, an abnormal heart rate in the fetus was observed, which disappeared without serious consequences when the concentration of the drug in the blood plasma decreased [26]. The question of the safety of using flecainide in the first trimester of pregnancy remains unresolved [8].
Flecainide has a proarrhythmic effect [27]. Based on data from the CAST trial, which showed increased mortality with its use, it is contraindicated in patients who have had a myocardial infarction [28]. However, in general, flecainide is considered a fairly safe drug during pregnancy [29]. The drug is highly effective for ventricular and atrial tachyarrhythmias in pregnant women. Many authors consider flecainide as a first-line drug for the treatment of supraventricular tachycardia developing against the background of hydrops fetalis [30,31]. A retrospective analysis showed higher fetal survival when treated with flecainide compared to cardiac glycosides [29]. However, no side effects were detected in the fetus. Flecainide also did not cause serious cardiac arrhythmias in the mother [30]. Reports of adverse reactions from flecainide are rare, but intrauterine death has been described, which may be associated with its use [27].
There is less experience with the use of propafenone during pregnancy than with flecainide [32]. When it was prescribed in the third trimester of pregnancy, no adverse reactions were observed in the mother or fetus. It should be noted that propafenone has the same effects on cells as flecainide, so its use should, if possible, be avoided in women with a history of myocardial infarction. The safety of the drug in the first trimester of pregnancy has not been determined [7].
Class II drugs (beta blockers)
Beta blockers can be used to treat various supraventricular and ventricular arrhythmias in the mother and fetus. They are also widely used during pregnancy to treat hypertension, hyperthyroidism and hypertrophic cardiomyopathy. When treating pregnant women with beta-blockers, quite a variety of side effects were observed in the fetus: bradycardia, apnea, hypoglycemia, metabolic disorders, induction of preterm labor, but their frequency was low [16]. Prospective randomized trials failed to identify significant differences in the incidence of adverse reactions of beta-blockers compared with placebo, and therefore it was suggested that these reactions are a manifestation of fetal distress in high-risk pregnancies [13,33].
There is a report of a slowdown in fetal development under the influence of propranolol [34], but other studies have failed to confirm these results. This effect was not observed in placebo-controlled studies of metoprolol [35]. Atenolol causes fetal growth retardation when used in the first trimester, so its use in early pregnancy should be avoided [36,37]. When using the drug in the second and third trimesters, such an effect was not observed [37].
Preference in pregnant women should be given to cardioselective beta-blockers (for example, metoprolol or atenolol) or drugs with internal sympathomimetic activity, as they cause fewer side effects associated with blockade of beta2-adrenergic receptors - peripheral circulatory disorders and increased myometrial tone [13].
Class III drugs (potassium channel blockers)
This class of antiarrhythmic drugs includes amiodarone, bretylium, sotalol and ibutilide.
Amiodarone combines the properties of drugs of classes I, II, III and IV. It is a powerful antiarrhythmic agent intended primarily for the treatment of ventricular arrhythmias. The drug contains 38% iodides, which cause the development of hypothyroidism in the fetus [38]. A feature of amiodarone is its very long half-life (26-107 days), and therefore it can accumulate in the body. Along with hypothyroidism, when amidarone is used during pregnancy, bradycardia and prolongation of the QT interval in the fetus/newborn, low birth weight, and premature birth have been reported [39,40]. Congenital anomalies have also been described in newborns whose mothers took the drug in the first trimester of pregnancy, so amiodarone should not be prescribed during the period of organogenesis [40,41]. If possible, its use should be avoided throughout pregnancy. The simultaneous administration of amiodarone and beta-blockers is also not recommended. The adverse reaction profile of amiodarone allows its use only in life-threatening situations, in case of ineffectiveness of other antiarrhythmic drugs [42,43]. It is categorized as Category D by the FDA.
Sotalol is a non-cardioselective beta-blocker with a simultaneous blocking effect on potassium channels. It quickly and completely passes through the placental barrier. The most dangerous side effect of the drug is the development of torsades de pointes. However, the risk of this complication can be reduced by careful history taking and examination of the pregnant woman, as well as treatment under ECG monitoring. Sotalol is highly effective against atrial flutter in newborns [44,45]
The FDA categorizes sotalol as Category B (Animal reproduction studies have not demonstrated a risk to the fetus, and no controlled studies have been conducted in pregnant women, or adverse effects (other than decreased fertility) have been shown in animal experiments, but their results have not been confirmed in controlled studies in women in the first trimester of pregnancy (and there is no evidence of a risk in other trimesters), although experience with its use in pregnancy is limited. Available data suggest that the drug is well tolerated.
The experience of using bretylium in pregnant women is also extremely small. It is a group C drug. Insufficient safety data prevents its routine use from being recommended. During pregnancy, bretylium should be reserved for life-threatening arrhythmias when other drugs are ineffective.
A new representative of this class of antiarrhythmic drugs is ibutilide. It is used to relieve ventricular fibrillation and atrial fibrillation. The main side effect of ibutilide is torsades de pointes. This side effect occurs in 1.7% of patients [46]. In experimental studies, the drug led to the development of congenital anomalies in animals. The mechanism of its teratogenic action is similar to that of phenytoin [22]. There is no clinical experience with the use of ibutilide in pregnant women, so it is recommended to avoid its use in this category of patients [7]. The FDA has classified ibutilide in safety category C.
Class IV drugs (calcium channel blockers)
This class is represented by verapamil and diltiazem. In pregnant women with supraventricular tachycardia, verapamil has a good therapeutic effect, however, when it was used to treat supraventricular arrhythmia in the fetus, various side effects were observed, incl. serious: bradycardia, heart block, contractility depression, hypotension, arrhythmias and fetal death [47]. Since many organogenesis processes in the first trimester of pregnancy involve calcium, concerns have been raised about the teratogenic effect of calcium channel blockers. They were based primarily on data from an experimental study that showed impaired embryogenesis in frogs [48]. A retrospective analysis of pregnancy outcomes in 57 women who received verapamil in the first trimester did not reveal an increase in the incidence of congenital anomalies under its influence [49]. In children of 137 women who received the drug in the second and third trimesters of pregnancy, no undesirable consequences of its use were also detected [50]. However, if safer alternatives are available, it is recommended to avoid the use of verapamil during pregnancy.
There is much less experience with the use of diltiazem in pregnant women. Teratogenic effects and miscarriages have been observed in animal experiments [51,52]. Theoretically, diltiazem may cause the same side effects as verapamil. Both drugs are classified as Category C by the FDA.
Adenosine
Adenosine in doses up to 24 mg has been successfully used to relieve supraventricular tachycardia in pregnant women without causing significant side effects in the mother and fetus [13]. Mothers experienced increased uterine tone, bradycardia, hypotension and dyspnea, but they were transient (several minutes). The fetus also experienced transient bradycardia [2]. The drug was prescribed mainly in the second and third trimesters of pregnancy. There is very little experience with its use in the first trimester, therefore, if possible, you should refrain from prescribing it in the early stages of pregnancy. However, it is considered the drug of choice for stopping supraventricular tachycardia in pregnant women [53]. Adenosine can provoke bronchospasm, so it should not be prescribed to women suffering from bronchial asthma [54]. It is classified as a Category C drug by the FDA.
In pregnant women, the activity of the enzyme adenosine deaminase, which is involved in the metabolism of adenosine, decreases by approximately 25%, but the potency of the drug does not increase due to changes in intravascular volume [55]. Moreover, it may even decrease, leading to the need to increase doses [56].
Digoxin
Digoxin has been used for many years to treat maternal and fetal supraventricular arrhythmias [44]. The drug penetrates well through the placenta. In therapeutic doses, it causes virtually no side effects in the mother and fetus [12,16]. In cases of overdose, spontaneous abortion [57] and fetal death associated with intrauterine hypoxia have been described [58]. Caution should be exercised when simultaneous use of digoxin with drugs that increase its concentration in the blood, and appropriate dose adjustments should be made [12]. The dose of the drug should also be adjusted in case of renal failure. During the treatment period, it is necessary to monitor the concentrations of digoxin in the blood, although in the third trimester, the radioimmune method of assessment can obtain falsely elevated results, since a digoxin-like substance circulates in the blood [59].
Extensive long-term experience with the use of digoxin allows us to conclude that it is one of the safest antiarrhythmic drugs during pregnancy [13]. However, according to FDA criteria, it is classified as Category C.
The main characteristics of antiarrhythmic drugs during pregnancy are summarized in the table.
Thus, despite the fact that there is not a single antiarrhythmic drug that is absolutely safe during pregnancy, most of them are tolerated quite well, and their use is not associated with a high risk of complications for the fetus and mother. Drug therapy should, if possible, be avoided in the first trimester. If it is necessary to prescribe medications in the early stages of pregnancy, preference should be given to drugs whose safety has been confirmed by extensive and long-term experience in this category of patients.
Symptoms
Characteristic features:
- change in heart rate;
- interruptions in heart function;
- unmotivated fatigue;
- dyspnea;
- noise in ears;
- tremor (shivering) of the limbs;
- nausea, vomiting;
- dizziness;
- visual impairment;
- loss of consciousness.
Symptoms usually first appear after 20 weeks, when the workload on the heart increases. Complications are more often detected in the third trimester. With previous heart diseases, the condition of the expectant mother worsens from the early stages of gestation.
What types of arrhythmia occur during pregnancy?
Arrhythmia is a serious medical problem. Heart rhythm disturbances pose a threat to the formation of the fetus and the course of gestation. Complications may develop:
- spontaneous miscarriage;
- gestosis;
- premature birth;
- chronic hypoxia and fetal malnutrition.
Practice shows that the risk of complications is higher with previous cardiovascular pathology.
Let's take a closer look at what forms of arrhythmia are detected during gestation. and how to recognize them by their characteristic features.
Extrasystole
Extrasystolic arrhythmia is the most common type of cardiac dysfunction in pregnant women. It occurs predominantly in the third trimester and is often asymptomatic. Accompanied by interruptions in cardiac activity and other nonspecific symptoms.
Short-term extrasystole is not dangerous to the health of the mother and fetus. The resulting hemodynamic disturbances do not interfere with the course of pregnancy. As the pathology progresses, fetal hypoxia develops. The risk of complications is higher with concomitant heart disease.
Sinus arrhythmia
With this option, the normal rhythm of the heartbeat is disrupted and becomes chaotic. At first it may become more frequent, then slow down with subsequent normalization. The intervals between individual contractions take on different lengths.
The cause of the pathology is a malfunction of the sinus node. It is through it that the impulse passes with a certain periodicity. But if the rhythm is disrupted, the node sends signals at various intervals. All parts of the heart contract sequentially, but without a clear rhythm. This is how sinus arrhythmia develops.
In clinical cardiology, it is customary to separately distinguish respiratory arrhythmia. Here, disorders are associated with movements of the chest during inhalation and exhalation.
Sinus arrhythmia during pregnancy is usually not dangerous for the mother and fetus. Such attacks do not affect the general condition of the body and have a short duration. But, if a woman’s well-being worsens, the fetus suffers, a consultation with a cardiologist and selection of therapy is indicated. Progressive sinus arrhythmia during pregnancy threatens the development of fetal hypoxia and premature birth.
Wolff-Parkinson-White syndrome
WPW syndrome is a form of supraventricular tachycardia. Observations show that this form of arrhythmia in pregnant women is rare and is usually associated with previous heart pathology. The anatomical substrate of the disease is the formation of additional atrioventricular pathways (“bridges”). The bioelectric impulse from the sinus node spreads abnormally quickly and can move in a circle.
Symptoms of WPW are nonspecific. Pathology is detected on an ECG. During an attack, heart rate reaches 200 beats/min. Atrial fibrillation and cardiac arrest are possible.
Paroxysmal tachycardia
Paroxysmal conditions rarely occur during pregnancy without a previous background. They usually complicate myocardial ischemia. By localization they can be atrial and ventricular.
An attack of paroxysmal tachycardia occurs suddenly. Heart rate increases to 200 beats/min. There may be complaints of tinnitus and dizziness. In pregnant women, an attack often occurs against a background of nausea. Possibly reversible speech impairment.
A prolonged attack of paroxysmal tachycardia is dangerous for the mother and fetus. Termination of pregnancy is possible.
What arrhythmias are more common in pregnant women?
The most common types of extrasystole are atrial and ventricular. These are extraordinary, premature contractions of the heart. They may not be felt at all and can only be detected during examination or taking an ECG. But a pregnant woman may feel an extrasystole as a sinking heart or experience other unpleasant sensations (see article on cardiac arrhythmias).
The significance of extrasystole, as well as other rhythm disturbances, for the course of pregnancy, the health of the mother and child, for the choice of method of delivery depends on whether the woman has heart disease, cardiovascular disease or other systems and organs. Therefore, all pregnant women with arrhythmias are subject to thorough examination by a cardiologist.
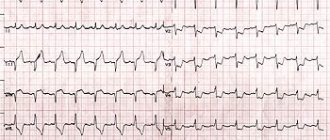
What tests should be performed if arrhythmia is detected or suspected in pregnant women?
In addition to general clinical examinations (clinical blood test, general urine test, fluorography), it is necessary to take an ECG, install a daily (or multi-day) ECG monitor (or ECG and blood pressure), perform an echocardiography, take a blood test for markers of inflammation, a blood test that allows assess thyroid function. As a rule, this is enough to find out whether there is any disease. In some cases, the doctor will prescribe additional studies and consultations with specialists, for example, an ENT doctor, if an infectious process is suspected, an endocrinologist, etc.
How dangerous are rhythm disturbances in pregnant women? Do they require treatment? Is this dangerous for the child?
Most expectant mothers do not develop any diseases. In this case, extrasystole is usually not dangerous.
In the vast majority of cases, supraventricular and ventricular extrasystole is not a contraindication to natural childbirth and does not require drug treatment.
The question of prescribing specific antiarrhythmic therapy is decided only by a cardiologist according to strict indications, taking into account all data on the mother’s health condition and taking into account the characteristics and number of arrhythmias according to Holter monitoring. There are no absolutely safe drugs for the fetus.
But if necessary, an experienced doctor will select the safest medicine in a minimal but sufficient dose.
Surgical treatments should, if possible, be delayed until the postpartum period, although ideally they should precede the planned pregnancy if the woman has a pre-existing arrhythmia. Pregnancy is not an absolute contraindication to radiofrequency catheter ablation (RFA) (for example, in the case of frequent, symptomatic, drug-resistant arrhythmias), but, of course, this procedure is a last resort due to the risk of exposure to the fetus; it can be carried out no earlier than the second trimester of pregnancy.
A healthy lifestyle and normalization of the psychological state are the key to successful treatment.
Much attention should be paid to the elimination of harmful substances and products and a healthy lifestyle. Sometimes this is enough to completely eliminate the arrhythmia.
Correction of the psycho-emotional status makes it possible to eliminate or significantly reduce a woman’s subjective feelings associated with arrhythmias, and in some cases reduce the number of rhythm disturbances, which makes it possible not to use antiarrhythmic drugs during pregnancy. To identify the connection between rhythm disturbances and psychological causes, psychological diagnostics and psychological counseling, and mental stress tests are carried out.
Case from practice
Patient E., 29 years old, was admitted to the cardiology department with complaints of rapid heartbeat, shortness of breath, and darkening of the eyes. From the anamnesis it is known that the first pregnancy proceeded without any special features. Previously, she was not registered with a cardiologist; she did not complain about heart function. According to the previous ECG, there are signs of sinus arrhythmia.
Three days before hospitalization, the woman felt a sharp heartbeat. I contacted my local gynecologist. The doctor sent the patient for an ECG, which showed supraventricular tachycardia. The woman was hospitalized and examined by a cardiologist and gynecologist on duty. At the time of examination, no pregnancy complications were identified.
Upon admission to the hospital, the patient's ECG showed signs of supraventricular tachycardia with a heart rate of 200 beats/min. Conservative therapy was carried out: Verapamil, potassium-magnesium mixture. An additional examination was carried out; echocardiography did not reveal any cardiac pathology. Within 24 hours, the patient’s condition improved and the attack was relieved. The control CTG showed signs of fetal hypoxia (Fisher score 7). Then the woman remained under the supervision of a cardiologist and gynecologist.
At 37-38 weeks, the patient was transferred to the pregnancy pathology department to prepare for delivery. The birth took place by caesarean section, without any special features. On the third day after the birth of the child, the heart rhythm was restored. There was no relapse in the postpartum period.
Atrial fibrillation
Atrial fibrillation is a disorder of the atria. At the same time, muscle fibers contract very often - up to 600 beats/min. It is customary to distinguish two forms of this condition:
- fluttering – sequential muscle contraction, heart rate up to 400 beats/min.;
- fibrillation – chaotic contraction of cardiomyocytes, heart rate up to 600 beats/min.
Atrial fibrillation during pregnancy does not go unnoticed. Women complain of rapid heartbeat and a feeling of shortness of breath. As the disease progresses, the risk of developing myocardial infarction and stroke increases. This condition can lead to termination of pregnancy at any stage.
Etiology of arrhythmia
of diseases can become fertile ground for the onset of arrhythmia.
, both
cardiovascular
and other body systems.
These are hypertension, coronary artery disease and myocardial infarction, heart failure, inflammatory, dystrophic diseases of the myocardium, valve defects (congenital and acquired), anomalies of heart development. Often the cause of rhythm disturbances is the dysfunction of the endocrine
system (hypo- and hyperfunction of the thyroid gland, Conn's syndrome, pheochromocytoma, menopause),
nervous, bronchopulmonary, and digestive systems
. Diseases affecting the entire body (anemia, infectious diseases and poisoning) can provoke arrhythmia.
Significant risk factors: abuse of alcohol, strong tea or coffee, any form of smoking, taking certain medications.
In addition, fasting, an unbalanced diet, food depletion of vitamins and microelements, dehydration, that is, any circumstances of disruption of water-electrolyte metabolism or acid-base status can lead to a failure of the normal electrical activity of the heart. Hereditary predisposition also matters.
However, in approximately 1/10 patients, even with high-quality examination, the cause of the arrhythmia cannot be determined (idiopathic arrhythmia).
Diagnostic scheme
If we suspect a heart pathology, we refer the patient to a specialized specialist – a cardiologist. The examination scheme includes:
- Anamnesis collection. It is important to find out whether the patient has heart and vascular diseases, endocrine disorders and other conditions - a possible cause of arrhythmia.
- Physical examination. We focus on the condition of the skin, assess heart rate, and measure blood pressure. We perform auscultation of the heart and great vessels.
- Instrumental methods: ECG and echoCG. According to indications, daily ECG monitoring is performed. These methods are recognized as safe for the fetus and are prescribed at any stage of gestation. If concomitant pathology is identified, consultation with specialized specialists is indicated.
Principles of treatment
We treat moderate heart rhythm disturbances in pregnant women on an outpatient basis. Hospitalization is indicated for the progression of pathology, the development of emergency conditions, and the appearance of signs of heart failure. A cardiologist and a gynecologist are monitoring the woman. If pregnancy complications develop, appropriate therapy is carried out.
Arrhythmia that occurs during gestation can become the basis for an induced abortion. The reason for termination of pregnancy is a progressive pathology that cannot be corrected and threatens the woman’s life. For medical reasons, abortion is performed up to 22 weeks.
Treatment of arrhythmia in pregnant women is not an easy task. The choice of tactics is determined by gestational age and concomitant diseases. When developing a patient management plan, the following factors should be taken into account:
- Treatment of arrhythmia must be comprehensive. It is important not only to normalize the rhythm, but also to eliminate the cause of the development of pathology;
- When selecting medications, the duration of pregnancy should be taken into account. Many common drugs are prohibited in the first trimester as dangerous to the embryo. Some drugs are not used throughout gestation. When choosing a drug, you should also take into account its effect on the myometrium - some medications provoke uterine hypertonicity and lead to termination of pregnancy;
- planned operations for cardiac arrhythmias are carried out at 16-22 weeks. Emergency intervention – at any time.
It is important to understand: there are no absolutely safe antiarrhythmic drugs. All of them can affect the fetus. Therefore, medications are prescribed only if it is impossible to cope without them. It is possible to use some drugs in reduced dosages. In this way, on the one hand, we help the woman’s body cope with rhythm disturbances, and on the other hand, we reduce the negative impact of the drug on the course of gestation.
In the treatment of arrhythmia in pregnant women, special attention is paid to non-drug methods. Recommended:
- Healthy food. The expectant mother's diet should include red meat and dairy products, vegetables and fruits. Food should be steamed and boiled. Fried foods are prohibited;
- move more. Fitness for pregnant women, yoga, water aerobics - everything will be beneficial;
- avoid stress. Any emotional experience is a path to heart disease;
- don't overexert yourself. Serious physical activity and hard work during pregnancy are prohibited.
Pregnancy against the background of a previous arrhythmia should be planned. If a woman has heart disease, she should consult a cardiologist before conceiving. According to indications, treatment is carried out before pregnancy, drugs are selected that correct the heart rhythm in the future. Such planning reduces the risk of complications and increases the chances of a successful pregnancy.
Sinus arrhythmia of the heart
The heart, as you know, contracts in a certain sequence, rhythmically. Heart rate is directly related to a person’s breathing, his condition and environment. For example, with increasing physical activity, a more intense contraction is observed. However, sometimes rhythm disturbances are not a natural reaction to environmental changes, but are pathological in nature. So, sinus arrhythmia is a change in heart rate towards its increase or decrease.
The very name of the disease suggests that “problems” occur in the sinus node, where there is a disturbance in the formation of an electrical impulse. As a rule, such a picture becomes a consequence of cardiovascular diseases. Most often, the disease manifests itself in two forms:
- Tachycardia (100 or more beats per minute) - pathological rapid heartbeat;
- Bradycardia (60 or less beats per minute) - decreased heart rate
Separately, it is necessary to highlight respiratory arrhythmia.
Causes of sinus arrhythmia
As already mentioned, many diseases of the heart and blood vessels can cause sinus arrhythmia. Although there are several other factors contributing to the development of the disease:
- Violation of the electrolyte composition of the blood, in other words, a lack, excess or incorrect ratio of potassium, calcium and magnesium in the blood cells. For example, with a deficiency of potassium and magnesium, the heart muscle is unable to fully relax. This, in turn, leads to spasm and, as a consequence, a lack of oxygen and nutrients in organs and tissues. Also, potassium deficiency can provoke the accumulation of sodium and fluid in organs and tissues, in particular in the heart, which also contributes to disruption of its functioning;
- Age and various types of diseases can also be called the cause of sinus arrhythmia. It is with age that almost irreversible changes in the body are observed: senile amyloidosis, liver disease, decreased thyroid function;
- Hypoxia (oxygen starvation), hypertension (high blood pressure), acidemia (high levels of acids in the blood).
In addition, the causes of sinus arrhythmia can be hidden in an unbearable sports schedule (too strict regimen, loads exceeding physical capabilities, poor nutrition and lack of long rest), stress. Some medications, alcohol, and various types of energy stimulants can cause the disease.
Symptoms of sinus arrhythmia
The most noticeable signs of the disease are dizziness, nausea, weakness, and fainting. These symptoms of sinus arrhythmia are associated with large time intervals between heartbeats or indicate the appearance of blockade of impulses at the exit of the atrium.
Diagnosis of symptoms of sinus arrhythmia
Perhaps every person can remember that at least once they have experienced discomfort in the heart area, tremors, and rapid heartbeat. In the event that such a condition is short-term and non-recurrent, there is no need to worry. However, if attacks become more frequent, accompanied by fainting, darkening of the eyes, severe weakness, you should visit a doctor as soon as possible.
At the initial stages, sinus arrhythmia is quite asymptomatic. However, the good news is that the manifestation of such an ailment as sinus arrhythmia on an ECG is possible. Therefore, even a routine medical examination will help identify the disease.
Sinus arrhythmia in children
Sinus arrhythmia is quite common in children and adolescents. There are periods when the disease is more likely to develop:
- 4-8 months;
- 4-5 years;
- 6-8 years;
- Pubertal (adolescent) period.
Sinus arrhythmia in children may have the following causes:
- Genetic conditioning, that is, the predisposition is already embedded in the genes, is present in parents and ancestors;
- Intrauterine pathologies of the fetus;
- Diseases and abnormal conditions of the heart muscle;
- Severe stress, emotional overstrain;
- Electrolyte imbalance caused by severe infectious and inflammatory processes (sore throat, pneumonia, intestinal infections).
It is customary to distinguish between 2 types of sinus arrhythmia:
- Respiratory . characterized by the fact that when you inhale, the heart rate increases, and when you exhale, on the contrary, it decreases. Such arrhythmia does not cause harm to health and does not cause pain, and therefore requires observation rather than treatment;
- Arrhythmia not associated with breathing is less common, but requires treatment. The cause of the disease can be heart disease, thyroid problems, and infectious diseases.
It is important to start treatment on time. As a last resort, for sinus arrhythmia in children, antiarrhythmic drugs and reflex treatment methods (neck massage, eye strain) are prescribed. Almost dozens of people are not prescribed pacemakers, and they are wary of physical procedures.
Sinus arrhythmia during pregnancy
Sinus arrhythmia occurs in 20% of pregnant women. The reason is the changes that occur in the body “at the request” of the fetus. Usually we are talking about rapid heartbeat, tachycardia.
The main reason for the development of sinus arrhythmia during pregnancy is considered to be an increase in the total volume of circulating blood, as well as the appearance of an additional circulation connecting the systems of the mother and child.
In addition, tachycardia can also develop as a result of emotional stress and instability to stress. Sinus arrhythmia during pregnancy can also be caused by anemia, electrolyte disharmonies caused by toxicosis.
During the period of bearing a child, a woman may experience exacerbation of chronic diseases. The latter can also provoke sinus arrhythmia.
Arrhythmia during pregnancy is dangerous because the risk of impaired blood supply to the fetus increases. As a result, it does not receive the required amount of oxygen and nutrients, which negatively affects the development of the fetus.
Treatment of arrhythmia during pregnancy should be carried out under the supervision of a physician (cardiologist) and a gynecologist. First of all, the cause of the disease should be identified. After its elimination, the rhythm will be restored. For example, in case of anemia, care should be taken to increase hemoglobin, and in case of excessive nervousness, the expectant mother is prescribed motherwort. If the cause of sinus arrhythmia is pathology of the cardiovascular system, antiarrhythmic drugs are used for treatment.
Treatment of sinus arrhythmia
Since sinus arrhythmia can be caused by various reasons, the underlying disease should be treated after identifying the cause. Normalization of the working day, a healthy lifestyle, in particular proper nutrition, and the required number of hours of rest and sleep are also shown. Provided that the disease is caused by pathologies of the heart muscle and cardiovascular system, treatment of sinus arrhythmia involves the prescription of antiarrhythmic and sedative drugs. For some indications, the patient may need a pacemaker or surgery.
In any case, the correct and effective treatment for sinus arrhythmia will be only what is prescribed by the doctor after appropriate diagnosis.
Expert advice: how to screen pregnant women with arrhythmia
Pregnant women with complaints about heart function, as well as with asymptomatic arrhythmia if changes are detected on the ECG, should be observed by a cardiologist. To clarify the diagnosis, daily ECG monitoring is carried out in dynamics:
- when the problem is first identified;
- at 30 weeks;
- at 37-39 weeks;
- 6 weeks after birth.
Pregnant women with arrhythmia are at high risk for developing obstetric complications. To detect abnormalities in a timely manner, you need to undergo ultrasound screenings (12-14, 18-21 and 32-34 weeks). The condition of the fetus is assessed objectively at each appointment, from 32 weeks - on CTG. If deviations are detected, hospitalization in the department of pathology of pregnant women or a therapeutic hospital is indicated.