Aortic regurgitation refers to a heart defect in which damage to the aortic valve prevents the semilunar valves from closing completely. This causes a characteristic circulatory disorder. When the heart contracts, blood is ejected from the left ventricle and then flows through the aorta into other vessels. In the absence of pathology in this area, the aortic valve flaps are completely connected, and this prevents blood from returning back. Blood moves through the aorta, completing its circulation. But if a pathology such as aortic valve insufficiency develops, normal blood flow is disrupted, the aortic valves do not completely close the aortic opening and part of the blood returns back to the left ventricle. Blood from the left atrium also arrives at the same time. There is much more blood in the left ventricle than it should be, it becomes overfilled, it rises, it needs to cope with a large volume of blood, making great efforts to maintain blood flow. Over time, as a result of this increased load, the muscle that pushes blood out becomes thicker. In addition, against the background of aortic insufficiency, the heart itself does not receive sufficient nutrition due to impaired coronary blood flow. This further aggravates the heart condition. Aortic valve insufficiency can be an isolated defect, or it can occur in various forms with other heart defects.
Symptoms
Given the large compensatory capabilities of the myocardium, the disease can be asymptomatic for a long time. And even when doing physical exercise, a person may not immediately feel any symptoms. Further progression of coronary and cerebral disorders lead to the appearance of the first symptoms in the form of dizziness, weakness, fatigue, increased heart rate and increased heart rate. Aortic insufficiency is manifested by tachycardia, felt at rest, symptoms intensify after physical exertion. There is pallor. Shortness of breath and angina attacks develop, which are poorly relieved by nitroglycerin.
A person with aortic valve insufficiency has external characteristic manifestations. He can see the pulsation of the cervical vessels “carotid dance” and he shakes his head in time with the pulse. When measuring blood pressure, increased systolic pressure is detected, but diastolic pressure always decreases, sometimes down to zero. Blood pressure always changes. The pulse is fast, high, large. An intensified elevating apical impulse is detected. The heart expands to the left.
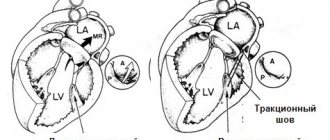
When listening, there is a weakening of the first tone at the apex, and a weakening of the second tone above the aorta (with severe destruction of the valve leaflets - until it completely disappears). A soft blowing diastolic murmur appears in the third intercostal space on the left and above the aorta. It can be heard more clearly if the patient exhales completely and holds his breath. Changes in blood flow that occur against the background of this defect cause a large expansion of the left ventricle, leading to mitral valve insufficiency. This will be manifested by the appearance of a systolic murmur. It is heard at the apex of the heart. Less common is Flint's diastolic murmur. Sometimes with this defect you can hear two noises on the femoral artery.
Complications
Complications of aortic insufficiency develop as its severity increases. At the beginning, normal syncope (fainting) may appear due to insufficient blood supply to the brain. Conduction disorders in the form of blocks of the left bundle branch and atrioventricular conduction of impulses can also often occur in patients with aortic insufficiency.
Coronary insufficiency can accompany aortic insufficiency, but more often in combination with aortic valve stenosis. The patient develops attacks of angina (pain in the heart of a pressing, squeezing nature) and even myocardial infarction.
Heart failure is the most common complication of already severe aortic regurgitation. The patient complains of shortness of breath during physical exertion, asthma attacks, and swelling of the lower extremities.
Sudden death often develops as a result of life-threatening arrhythmias - paroxysmal ventricular tachycardia, ventricular fibrillation. In this case, the person does not even have time to call an ambulance - the arrhythmia develops so quickly.
Diagnostics
First of all, the doctor can think about the presence of aortic valve insufficiency based on the results of the examination of the patient. Because the manifestations of this pathology have their own characteristics, revealed externally and by listening. As mentioned above, at a certain stage in the development of the disease, the patient’s characteristic appearance appears and heart murmurs appear. The diagnosis is confirmed after special research methods. Echocardiography can detect signs of this defect in the form of reverse blood flow, increased work of the muscular wall of the left ventricle in systole, and fluttering of the mitral valve as blood fills the left ventricle. A phonocardiogram clearly reveals changes in tones and noises that identify this defect. ECG and x-ray of the heart may not detect changes for a long time. They are detected already in the later stages, when left ventricular hypertrophy develops.
Causes and risk factors
Aortic valve insufficiency develops due to loose closure of the valves during the relaxation phase of the ventricles, which can develop for a number of reasons:
- idiopathic (unknown cause) dilation of the aorta;
- congenital defects of the aortic valve (usually bicuspid aortic valve);
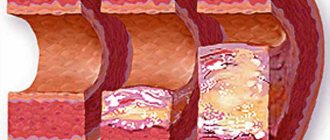
- sclerosis of the valves (due to atherosclerosis);
- rheumatism;
- infective endocarditis;
- arterial hypertension;
- myxomatous degeneration (disorder of connective tissue development);
- dissection of the ascending aorta;
- Marfan syndrome;
- aortic valve injuries;
- ankylosing spondylitis;
- syphilitic aortitis;
- rheumatoid arthritis.
Most of these causes lead to chronic aortic insufficiency, which can be asymptomatic for a long time. Others, in particular infective endocarditis, aortic dissection, and trauma are often accompanied by a sudden development of severe aortic insufficiency. This leads to serious hemodynamic disturbances. As a result, much less blood reaches vital organs: the brain, kidneys, liver, heart.
Treatment of aortic valve insufficiency
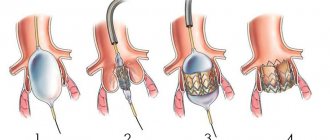
There are two types of treatment for this pathology. Aortic insufficiency is eliminated if treated with surgery, which radically solves the problem. In this case, an artificial valve is implanted. But the positive outcome of such an operation depends on the severity of the changes that have occurred in the myocardium.
Aortic valve insufficiency is treated conservatively; treatment is aimed at reducing the symptoms of this disease, which can be eliminated temporarily. At the same time, the time of onset of heart failure is delayed. The conservative method is aimed at maintaining the functioning of the heart and improving the condition of other organs. In order to prevent cerebral circulatory failure, as well as coronary circulatory failure, it is necessary to maintain a sufficient heart rate. This becomes possible with the use of cardiac glycosides (korglykon, strophanthin and others).
Vitamins, cocarboxylase, and riboxin are also used to maintain nutrition of the heart muscle. If complications occur, their treatment is prescribed.
Forecast
The prognosis for aortic insufficiency is better, the lower the degree of regurgitation and the earlier treatment is started. Preventive examination by a general practitioner, cardiologist, full antibiotic therapy in case of infective endocarditis and rheumatic fever - all this helps to improve the prognosis. It is very important to listen to yourself, your body, so as not to miss the first symptoms (lethargy, decreased performance, fainting, shortness of breath during physical activity).
Usually, with severe clinical heart failure, the prognosis worsens, since irreversible changes occur in the structure of the heart.
Who is indicated for surgical treatment?
The only form of surgery is aortic valve replacement. The operation is indicated for:
- severe form of regurgitation with impaired left ventricular function;
- if the course is asymptomatic, with preserved ventricular function, but pronounced expansion (dilatation).
Aortic valve replacement surgery is often combined with coronary artery bypass grafting.
Prevalence
Patients with aortic regurgitation are recorded only in functional diagnostic rooms. Therefore, prevalence can be judged in relation to the number of Doppler-examined patients rather than in relation to the total population.
Various degrees and signs of reverse blood flow through the aortic opening are found in 8.5% of examined women and 13% of men. Among all heart defects in adults, chronic aortic regurgitation is detected in every tenth patient. Most often in old age in men.
Severity
The ability to measure intracardiac pressure and register the backflow on ultrasound made it possible to subdivide the course of the defect into 3 degrees of severity.
- At stage 1 (initial), aortic insufficiency is characterized by a volume of returned blood of less than 30 ml per heartbeat, the proportion of the return fraction (regurgitation) is up to 30% of the volume of the left ventricle, the return flow enters inward at a distance of up to 5 mm beyond the valve.
- At grade 2 (moderate), the volume of returned blood is 30-59 ml for each contraction, the proportion of the regurgitation fraction increases to 50%, the stream extends beyond the valve to a distance of 10 mm.
- In grade 3 (severe), aortic return reaches 60 ml or more per contraction, and the fraction is more than 50%, while the length of the return jet is more than 10 mm.
The mechanism of regurgitation in normal and pathological conditions
Cardiologists identify minor physiological regurgitation, which is possible under normal conditions. For example, 70% of tall adults have incomplete closure of the tricuspid valve, which the person is not aware of. Ultrasound reveals slight swirling flows when the valves are completely closed. This does not affect general blood circulation.
Pathology occurs during inflammatory processes:
- rheumatism,
- infective endocarditis.
Most typical for mitral localization, the formation of heart disease. It should not be confused with prolapse (stretching and bending of the valves into the atrium). It is with prolapse that physiological regurgitation often occurs and is found in growing children and adolescents. It is taken into account as a possible cause of extrasystole. The child must be observed by a cardiologist and re-examined. No special treatment is required.
The formation of scars after an acute heart attack, against the background of cardiosclerosis, in the area approaching the valve leaflets and threads, leads to breakdown of the necessary tension mechanism and changes the shape of the leaflets. Therefore, they do not completely close.
In a pathological process, an equally significant role is played by the diameter of the outlet, which must be blocked. Significant enlargement due to left ventricular dilatation or hypertrophy prevents the tight junction of the aortic valve leaflets.
Consequences of aortic regurgitation
The return of blood to the left ventricle inevitably leads to its expansion and increase in volume. Possible expansion of the mitral annulus and further enlargement of the left atrium.
At the point of contact of the blood flow, “pockets” are formed on the endocardium. The greater the degree of regurgitation, the faster the left ventricular overload develops.
Studies have shown the meaning of heart rate:
- bradycardia increases the volume of return flow and promotes decompensation;
- tachycardia reduces regurgitation and causes greater adaptation.
Forms of aortic regurgitation
It is customary to distinguish between acute and chronic aortic regurgitation.
Features of the acute form
Typical causes of acute aortic regurgitation are:
- injuries;
- dissecting aneurysm;
- infective endocarditis.
The volume of blood entering the left ventricle during diastole increases suddenly. Adaptation mechanisms do not have time to develop. The load on the left side of the heart and myocardial weakness increases sharply. Insufficient blood volume is released into the aorta to support general circulation.
Patients develop signs of pulmonary edema and cardiogenic shock. Symptoms are very severe when hypertension and aortic aneurysm dissection are combined.
Features of chronic aortic regurgitation
A distinctive feature of the chronic form is sufficient time for the full activation of compensatory mechanisms and adaptation of the left ventricle. This causes a period of compensation for circulatory disorders. Myocardial hypertrophy helps compensate for the reduced output.
When reserve energy reserves are depleted, a stage of decompensation occurs with severe heart failure.
Pathological changes
Anatomical changes depend on the disease, in which aortic insufficiency is a concomitant pathology and complication.
- Rheumatic damage to the aortic valves ends with wrinkling and soldering of the valves at their base. Insufficiency and some narrowing of the hole are formed.
- In infective endocarditis, damage begins at the edges of the valves. As a result of inflammation, they become scarred and deformed.
- The syphilitic process spreads from the aorta to the valves. Damage to the medial shell of the vessel and loss of elasticity lead to expansion of the connecting hole. The valves themselves are thickened and inactive.
- In atherosclerosis, damage also extends from the aorta to the valves. Atherosclerotic plaques and lime are deposited in them. By shrinking, the valves are unable to completely close the hole.
What does a doctor's examination give?
During the examination, the doctor pays attention to:
- pallor of the face and mucous membranes (due to insufficient filling of peripheral vessels);
- rhythmic constriction and dilation of the pupils;
- pulsating movements of the tongue;
- shaking of the head in rhythm with heart contractions (due to shocks from the carotid arteries);
- visible pulsation of blood vessels in the neck (symptom of “dancing arteries”), in the arms, movement of the lower leg in time with the contractions of the heart;
- at a young age, the defect causes the formation of a “heart hump” due to strong constant internal blows to the chest;
- when palpating the heart area, a powerful cardiac impulse is felt.
When determining the pulse, a feeling of rapid filling and then decline is created.
Auscultation of the heart and large vessels reveals typical noises from sudden movement of blood.
Blood pressure measurement shows an increase in the upper level with a significant decrease in the lower level (up to 40 - 50 mm Hg)
Causes associated with aortic damage
The portion of the aortic arch closest to the heart is called the aortic root. It is its structure that influences the “health of the valves” and the width of the gate ring from the left ventricle. Root lesions include:
- age-related or degenerative changes causing dilatation;
- cystic necrosis of the middle layer of the aorta in Marfan syndrome;
- dissection of the aneurysm wall;
- inflammation (aortitis) with syphilis, psoriatic arthritis, ankylosing spondylitis, ulcerative colitis;
- giant cell arteritis;
- malignant hypertension.
Among the reasons, a negative effect of drugs used to reduce appetite in obesity was found.