A coagulogram is a graphical expression of the results of a study of the hemostatic system. It is otherwise called a hemastosiogram. This is a fairly complex blood test that allows you to evaluate the functioning of the blood coagulation and anticoagulation systems and identify possible disorders. A coagulogram during pregnancy is a mandatory examination. Any deviations in the hemostatic system can cause miscarriage or premature birth.
For the health of the woman and the unborn child, it is important that the coagulation and anti-coagulation systems work in a balanced manner. If this balance is disturbed, any of the systems is more active, and various pathologies can develop in the woman and fetus. If the anticoagulant factor is more active, a woman may experience spontaneous bleeding, placental abruption is possible, and there is a danger of large blood loss during childbirth and after its completion.
If the activity of the coagulation component of hemostasis predominates, the blood becomes thick and there is a risk of developing blood clots, which can cause fetal hypoxia. The woman herself may develop blood clots, deep vein thrombosis of the lower extremities and pelvis, as well as pulmonary embolism.
Coagulogram parameters
During the analysis, the following parameters are examined:
- Fibrinogen. This special protein is synthesized in the liver and takes part in blood clot formation. Fibrinogen is considered one of the main components of a blood clot. When a vessel is damaged, it turns into insoluble fibrin strands, which ultimately form a blood clot. It closes the vessel defect, thereby preventing blood loss. The fibrin clot remains at the site of injury until complete healing only if the components of the clot are present in sufficient quantities. A deficiency of prothrombin and fibrinogen leads to bleeding; an excess amount of these factors can result in the formation of blood clots without damaging the vessel walls.
- Prothrombin. Production occurs in the liver with the participation of vitamin K. One of the main blood clotting factors. This indicator makes it possible to prevent placental abruption, bleeding during childbirth, and the development of thrombosis. It allows you to identify pathologies of the liver and digestive system.
- APTT. This is the time during which the formation of a blood clot occurs. With its help, the functioning of the coagulation system is assessed according to the internal mechanism and it is determined whether there is a lack of plasma blood factors.
- Thrombin time. During this time, a blood clot forms after the blood plasma mixes with thrombin.
- Prothrombin time. During this time, a thrombin clot is formed when thromboplastin and calcium are added to the plasma.
- RFMK. These are intermediate products of fibrin thrombus breakdown as a result of fibrinolysis (soluble fibrin-monomer complexes). They are difficult to detect because they are removed from the plasma very quickly.
- Antithrombin III. This complex protein is produced by liver and vascular cells. It prevents blood clotting and the formation of clots.
- Lupus anticoagulant. These are immunoglobulins M and G, which in case of autoimmune lesions of platelets (thyroiditis, rheumatoid arthritis, lupus erythematosus) are produced against their membranes. Normally, it is not present in the blood of a pregnant woman. Determined in the presence of autoimmune diseases or gestosis. Lupus anticoagulant complicates pregnancy and can lead to miscarriage.
- D-dimer. This is an indicator of the process of clot formation and fibrin dissolution.
Hemostasiogram - interpretation of indicators
A blood test for a coagulogram can be of two types:
- the main one - allowing to identify the quantitative content of fibrinogen, prothrombin, INR, aPTT and thrombin time;
- advanced - in addition to the main parameters, D-dimer, lupus AK and antithrombin are subject to study
- Fibrinogen is a coagulation factor formed from fibrin. The higher the amount of fibrinogen, the higher the risk of blood clots. The decrease in fibrinogen occurs synchronously with total protein in a biochemical blood test;
- Prothrombin and INR are indicators of blood clotting rate. Prothrombin is the second coagulation factor, and INR (international normalized ratio) is a laboratory indicator of the external pathway of the hemostatic system;
- APTT (activated partial thromboplastin time) is an indicator of blood clotting time from the moment of bleeding to the onset of clot formation against the background of reagents;
- Thrombin time is an indicator of the time (in seconds) during which a clot forms. In DIC syndrome, thrombin time is not determined;
- D-dimer is an additional indicator for assessing the blood coagulation system. It is a fibrin breakdown product. A significant increase may have a physiological etiology, since the D-dimer increases with increasing period;
- Antithrombin III is a specific protein responsible for blood thinning;
- Lupus anticoagulant is an indicator of the disease “systemic lupus erythematosus,” in which antibodies to blood enzymes are produced.
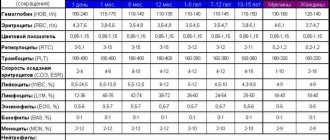
The table shows an example of normal values and deviations from the norm.
| Index | Norm | Pathology |
| fibrinogen | 4.0-6.0 g/l | Increase: heart attack, stroke, burns, postpartum period, surgical actions; Decreased: lack of vitamins, taking anticoagulants, development of disseminated intravascular coagulation |
| PV | 78-142% | Increased: thrombosis, taking thinning drugs; Decreased: DIC syndrome, blood diseases |
| TV | 10-18 sec | Increased: heparin use, liver failure, bleeding; Reduction: 1st stage of internal combustion engine |
| APTT | 17-20 sec | Increased: hemophilia, APS (rare); Decrease: bleeding, 1st phase of DIC |
| D-dimer | 1st trimester – 750 ng/ml 2 trimester up to 1000 ng/ml 3rd trimester up to 1500ng/ml | Increases in thrombophilia, disseminated intravascular coagulation syndrome, diabetes mellitus; A decrease in the indicator has no diagnostic value, with the exception of the therapy performed. |
| antithrombin | 70-115 % | Increase: taking anticoagulants; Decrease: thrombosis |
| Lupus AK | negative | Appearance means APS, HIV, Systemic lupus erythematosus |
Differences in results between pregnant and non-pregnant women
Indicators of the coagulation system have a significant difference between pregnant and non-pregnant patients:
- What kind of blood coagulogram analysis is this, interpretation in adults and the norm in the table
- Fibrinogen in non-pregnant women is 2 units less.
- APTT is slightly elevated in women who are not in an interesting position.
- D-dimer is no more than 250 ng/ml.
How is the test done?
No special preparation is required. Like any blood test, it is taken in the morning on an empty stomach. Blood is taken from a vein in the bend of the elbow. Pregnant women get tested at the antenatal clinic. Decoding is the responsibility of the gynecologist with whom the expectant mother is registered. If all blood parameters are normal, this test is taken every trimester, that is, only three times:
- at the first visit to the gynecologist about pregnancy;
- around the 23rd week;
- shortly before birth - at the 34th - 36th week (this is especially important for those who are indicated for a cesarean section).
During pregnancy, blood is donated for a coagulogram every trimester.
If there are deviations from the norm, coagulation testing will have to be performed more often.
The need and frequency of testing for coagulation during pregnancy
For pregnant women, a coagulogram is an extremely important analysis. With its help, the balance of the coagulation and anticoagulation systems is monitored.
- The absence of such a balance carries, as mentioned above, consequences that threaten the health of the expectant mother and fetus.
- An imbalance towards the anticoagulation system can cause metrorrhagia, placental abruption, blood loss during and after childbirth in a woman in labor, and towards the coagulation system it thickens the blood, forming blood clots. In this case, a child who receives oxygen exclusively from the placenta experiences oxygen starvation, hypoxia develops, brain pathologies may develop, the woman suffers from leg pain and the development of blood clots, and this can also cause a heart attack, stroke or miscarriage.
The test procedure is as follows: before taking blood, it is better to fast, that is, take the test on an empty stomach. Blood is taken from a vein on the bend of the elbow, and the result of the hemostasiogram is deciphered by your attending physician.
If the indicators are normal, the diagnosis is carried out three times as planned:
- During the registration of a pregnant woman (usually the 1st trimester),
- In the second trimester,
- A week or two before giving birth, which is especially important for women who are preparing to give birth by cesarean section.
In case of complications or abnormal pregnancy, homeostasis is checked much more often in order to respond adequately and prescribe effective treatment.
The normal indicators for a woman during this period, due to changes in physiology, are somewhat different from the indicators before conception, since the female body sets up another blood circulation through the utero-placental-fetal blood flow (insuring itself from significant blood loss). Therefore, only your registered doctor can diagnose the coagulogram results.
Indications for additional testing
Sometimes a pregnant woman has to take a coagulogram test more often than once per trimester. This happens in cases where a woman has the following pathologies:
- Autoimmune diseases.
- Liver diseases.
- Phlebeurysm.
- Disturbances in the functioning of the urinary, endocrine and hematopoietic systems.
- Vascular pathologies.
- Condition after surgery.
- Multiple pregnancy.
- Predisposition to increased blood clotting.
- Tendency to bleed.
- Deviations from the norm discovered during the first study.
- Having bad habits.
- Miscarriage.
- Fetoplacental insufficiency, gestosis.
Deciphering violations in the results and their causes
Below is a table of deviations from the norm in the coagulogram, which are dangerous during pregnancy and their possible causes.
| Index | Numerical value within normal limits | Possible deviation | Causes |
| APTT | 15-20 seconds | increase to 25-39 sec. reduction to 10-12 sec. | vitamin K deficiency, von Willebrand disease, liver disease. DIC syndrome, inflammatory processes. |
| Fibrinogen | 6 g/l | Increase over 6 g/l | Infectious diseases, necrotic processes, burns and injuries, lupus, heart attack, tumor |
| D-dimer | 250 ng/ml | Increase more than 4.5 times | Preeclampsia, kidney disease, internal hematomas and hemorrhages |
| Platelet level | 150-350 * 1099 per 1 l. blood | increase; decrease. | diarrhea, toxicosis, frequent vomiting, thromboembolism, dehydration, chronic bleeding, poor nutrition, disorders of the immune system. |
Coagulogram norms and interpretation
The test results are interpreted by a gynecologist. Coagulogram indicators should have the following values during pregnancy:
- Fibrinogen. During pregnancy, the level of this protein should be normal in the first trimester. In the second trimester it rises to 4–5 g/l. Closer to childbirth, the normal level is 6 grams/liter.
- Thrombin time. This indicator during pregnancy is slightly higher than normal. Its value should be between 11 and 18 seconds. If it is higher than normal, there may be liver pathologies.
- APTT. As for the activated partial thromboplastin time, in expectant mothers it is slightly reduced, which is the norm during this period. Its value is from 17 to 20 seconds.
- Prothrombin. This is one of the most important hemostasiogram indicators for a pregnant woman, since exceeding the norm can lead to placental abruption. This figure should be between 78 and 142%.
- Prothrombin time. This important indicator is normally no more than 18 seconds and should not change during pregnancy. Otherwise, you should definitely consult a doctor to find out the cause and take action.
- Lupus anticoagulant. This is an indicator of the presence of antibodies that contribute to an increase in aPTT. There should be no antibodies during pregnancy. If they are detected, then this is a sign of gestosis or an autoimmune disease.
- RFMK. The norm in the first trimester is 78-130 units, in the second - 85-135, in the third - 90-140.
- Antithrombin III. This is an anticoagulant component of hemostasis, which is considered one of the main parameters of the analysis. Normally it should be 75-125%. If it is below 75%, then there is a tendency to form blood clots. If it is above 125%, there is a risk of bleeding.
- D-dimer. Shows the process of blood clot formation. During pregnancy it may increase slightly. The normal value is from 33 to 726 ng/ml. If it rises sharply in a pregnant woman, this may indicate gestosis, diabetes mellitus, or kidney disease.
During pregnancy, it is very important to monitor all coagulogram indicators and, if necessary, undergo treatment
If pregnancy proceeds with complications, for example with gestosis, disturbances occur in blood coagulation. The lifespan of platelets decreases, fibrinolytic activity increases. In the absence of treatment for gestosis, there is a high probability of developing a severe complication - disseminated intravascular coagulation syndrome (DIC syndrome). At the first stage - hypercoagulation - many small blood clots form, blood circulation between mother and child is disrupted. Then comes hypocoagulation - the breakdown of blood clots when coagulation factors are depleted. And the third stage is the complete absence of coagulation (acoagulation), which leads to uterine bleeding and, most often, to the death of the fetus.
Deciphering the coagulogram of a pregnant woman is quite a difficult matter. Each woman is individual and each needs a special approach. Even if the indicators deviate slightly from normal values, do not panic. The main thing is to undergo all additional examinations on time and correct unwanted changes at an early stage together with your doctor.
At what stage of pregnancy is a coagulogram performed?
The question of how often to take a coagulogram during pregnancy cannot be answered unambiguously. The patient’s examination protocols indicate the need for hemostasiograms to be taken three times throughout the entire pregnancy, once per trimester:
- during registration (up to 12 weeks);
- at 20–24 weeks of pregnancy (time of the second screening);
- at 32–36 weeks of pregnancy (to prepare for delivery).
However, this test scheme is only suitable for those patients who do not have a complicated medical history, pregnancy proceeds without complications, and previous coagulogram results were within normal limits. In all other cases, the timing of the analysis is decided by the attending physician.
Important! Before any surgical intervention (appendectomy, cholecystectomy, cesarean section), donating blood for a coagulogram is mandatory!
Additional coagulation analysis may be prescribed for the following conditions:
- smoking during pregnancy;
- fetoplacental insufficiency;
- fetal hypoxia;
- delayed growth and development of the fetus;
- Rhesus conflict;
- varicose veins;
- history of infertility and miscarriage;
- multiple pregnancy;
- disruption of the cardiovascular, urinary and other organ systems.
Rules for taking a coagulogram test during pregnancy
Blood for hemostasiogram analysis is taken from a vein with a syringe. In order for the result to be the most reliable, it is necessary to prepare for a coagulogram test during pregnancy, adhering to such measures as:
- Before the procedure, do not eat food for 7-8 hours. Most often, blood donation occurs in the morning, so you must come on an empty stomach. In the morning you are allowed to take a couple of sips of water and brush your teeth.
- It is advisable to limit yourself from stress and anxiety during any tests.
- Avoid increased physical activity for two days preceding the procedure.
Detailed coagulogram during pregnancy: what indicators are included?
There are two types of coagulogram: standard and expanded. As a screening method, a standard type of coagulogram is used, including the following indicators:
- Blood coagulogram (blood clotting test): interpretation in adults, norm in the table
- APTT (activated partial thromboplastin time). This indicator determines the optimal time for the formation of a blood clot. A decrease in aPTT threatens the development of DIC syndrome (disseminated intravascular coagulation) in the postpartum period; an increase in the indicator means an increased risk of bleeding.
- Fibrinogen. It has a protein nature and is produced in the liver. Refers to the main link in thrombus formation. Fibrinogen levels increase slightly before labor. A sharp increase in the indicator is characteristic of the development of an infectious process.
- Thrombin time. Shows how long it takes fibrinogen to transform into fibrin, and then fibrin forms a blood clot.
- Prothrombin (or prothrombin index, PTI). It is one of the components of blood plasma. Shows how active the plasma prothrombin complex is compared to the plasma prothrombin time. An increase in the level of PTI is characteristic of placental abruption.
An extended coagulogram during pregnancy includes additional indicators:
- Prothrombin time (or PTT). An indicator showing how many seconds it takes to form thrombin from prothrombin, which is involved in the formation of a blood clot.
- Antithrombin III. This is a protein that slows down blood clotting. A decrease in it during pregnancy carries a risk of developing pathological thrombosis, and an increase carries a risk of bleeding.
- Platelets. Blood cells responsible for the state of the coagulation system. They are the ones who fill the fibrin networks, forming a blood clot. A slight decrease in platelets during pregnancy is a common occurrence, but significant fluctuations are a sign of pathology (a decrease in their production or, conversely, increased destruction). A significant decrease in the indicator carries the risk of developing DIC syndrome.
- INR (international normalized ratio). This is a calculated indicator characterizing the ratio of the patient’s prothrombin time to the total average thrombosed time. An increased INR carries a risk of bleeding, a decreased INR carries a risk of thrombosis. The indicator is often determined to monitor the condition when treating patients with anticoagulants and antiplatelet agents.
- D-dimer. One of the main indicators of the thrombus formation procedure. Determining d-dimer in a coagulogram during pregnancy and before conception makes it possible to timely identify the risk of thrombosis and begin timely treatment with anticoagulants.
- Lupus anticoagulant. Antibody formation indicator. Normally, it should be absent during pregnancy. Its presence in the blood indicates either the presence of autoimmune diseases or the development of Rh conflict.
- RFMC (soluble monomer complexes). An indicator that allows you to assess the massiveness of thrombus formation. During pregnancy, it can be 2–3 times higher than the non-pregnant norm. A significant increase occurs in shock conditions: disseminated intravascular coagulation syndrome, trauma, extensive thrombosis.
Coagulogram - what is it?
Many patients needlessly begin to worry when they hear from their attending physician such unusual at first glance words as coagulogram or otherwise hemostasiogram . So what kind of coagulogram analysis is this and why is it taken?
First of all, it is worth noting that this is a fairly common method in modern medicine for studying the functioning of the hemostatic system of the human body, which is responsible for such important vital functions as stopping bleeding when blood clots or blood vessels , as well as maintaining the normal fluid state of the blood.
Hence the answer to the question of what a hemostasiogram - a study that determines how well the body’s hemostasis system functions. A blood coagulogram test helps to study such an important blood function as the ability to clot, i.e. formation of a blood clot.
Having received the results of coagulation , the attending physician can predict in advance the outcome of the operation or childbirth. Information about blood clotting is vital in emergency situations, for example, when a person is injured, when seconds count and you need to stop the bleeding .
Therefore, you hardly need to worry too much about how much this research costs. After all, the price of a hemostasiogram cannot be compared with the confidence that the patient will be alive and healthy.
Indications for prescribing such an analysis as a hemostasiogram are the presence of the following diseases in the patient:
- intestinal thrombosis;
- stroke;
- thromboembolism
- vascular thrombosis and varicose veins of the lower extremities;
- chronic cirrhosis
- gestosis;
- inflammatory processes in the acute stage;
- hemorrhagic pathologies, for example thrombocytopenia , hemophilia or von Willebrand disease .
In addition, such an analysis is necessarily prescribed to determine the rate of blood clotting in preparation for planned operations, for example, cesarean section, as well as during pregnancy to assess the state of hemostasis and before spontaneous childbirth . Every woman in labor must have a blood test such as a coagulogram in her exchange card.
Human hemostasis system
Having determined what a hemostasis test is, it is worth understanding in more detail such a concept as blood clotting . Perhaps we should start with a definition. So, the hemostasis system of the human body is the most important biological system, the main functions of which can be considered to be the preservation of basic blood parameters, as well as stopping bleeding.
It is not for nothing that the human body is called the whole universe and is compared to a complex mechanism. And the hemostasis system can serve as a striking example of how ingeniously people are designed. Blood is a unique biological fluid that can literally work miracles in our body.
It not only circulates through the vessels, but also, unnoticed by a person, restores veins and arteries throughout his life due to its ability to form blood clots or dense clots, i.e. roll.
There are three main components of the human hemostasis system:
- endothelial cells (the inner layer consisting of flat cells lining lymphatic and blood vessels, as well as the cavities of the heart), which, when vascular walls rupture or other damage, are capable of releasing biologically active components such as prostacyclin , thrombomodulin and nitric oxide . They, in turn, trigger the process of blood clot formation.
- Platelets or blood platelets that have the ability to “stick together” with each other in order to subsequently form a primary hemostatic plug .
- Plasma factors (15 plasma factors in total, most are enzymes ) that, due to chemical reactions, form a fibrin clot , which should finally stop the bleeding.
Summarizing all of the above, we can clearly answer the question of what a blood test for hemostasis shows during pregnancy, in preparation for a planned operation, or during diagnostics. This test gives an idea of how well or poorly a patient's blood is clotting. In other words, how quickly doctors can stop bleeding when it occurs.
How to properly prepare for a hemostasiogram?
Preparation for a hemostasiogram is an important step on which the test results depend. Blood is drawn from the ulnar vein, strictly on an empty stomach. In order for the analysis results to be informative within 8-10 hours, you should refrain from taking any medications, intense physical activity, or drinking alcoholic beverages. If a woman, for medical reasons, is forced to take medications that affect blood clotting, it is imperative to notify the doctor about this.
Increased thrombin time
This indicates a tendency to hypocoagulation. Thrombin time is increased when:
- treatment with fibrinolytics, heparin;
- a significant decrease in fibrinogen in the blood plasma (with functional disorders in the liver);
- excess physiological anticoagulants;
- some blood diseases;
- the second stage of the syndrome-DIC (impaired blood coagulation processes in critical conditions: severe injuries, shock, burns, massive thrombosis).
A shortening of thrombin time indicates a risk of thrombosis, and also occurs in conditions accompanied by an increase in fibrinogen content in the blood and in the first stage of DIC syndrome.
What is a hemostasiogram?
Blood coagulation system. Laboratory diagnosis of hemostasis disorders. Interpretation of results. Features of hemostasis during pregnancy. Molecular genetic analyses. Platelet function.
What is a hemostasiogram?
Blood coagulation system. Laboratory diagnosis of hemostasis disorders. Interpretation of results. Features of hemostasis during pregnancy. Molecular genetic analyses. Platelet function.
Blood clotting tests are important for identifying possible disorders in the hemostatic system, as well as for assessing the effectiveness of therapy, selecting the dose and monitoring therapy to prevent complications. Only with the help of laboratory diagnostics can an accurate diagnosis be made and the effect of medications adequately assessed.
High-quality laboratory diagnostics are very important for the attending physician to make the right decision. We use high-quality foreign-made reagents, conduct internal quality control and participate in external quality control programs. Comprehensive tests are developed jointly with clinicians who are our strict experts. We provide not only the results, but also a detailed report from the laboratory doctor on the hemostasiogram, determination of lupus anticoagulant, and platelet aggregation.
The need for hemostasis studies may arise in a person of any age and gender! Our laboratory examines women preparing for pregnancy and pregnant women; women taking contraceptives; patients receiving therapy with aspirin and heparin. Therefore, we provide excellent research quality, which is highly valued by clinicians .
Our laboratory offers various types of hemostasis studies. Both screening tests, such as a basic coagulation test, and complex studies, such as induced platelet aggregation, are performed.
Tests are taken at all CIR clinics, which is convenient for our patients. Test results can be received by email or courier.
The hemostasis system performs two main functions: maintaining blood in liquid form inside the vessels, on the one hand, and, on the other hand, quickly responding to vascular damage (forming blood clots to stop bleeding). The following are involved in blood clotting: the vascular wall, blood cells, and blood plasma proteins. The plasma hemostasis system consists of three interconnected systems - the coagulation system (coagulation), the anticoagulant system (anticoagulant) and the fibrinolysis system (thromt dissolution).
Coagulation parameters characterize the cascade leading to the formation of fibrin, the protein that forms the basis of the blood clot. Triggering of coagulation can occur as a result of activation of the intrinsic and extrinsic pathways.
Blood clotting disorders:
- hypocoagulation - decreased blood clotting, manifested by bleeding,
- hypercoagulation - increased blood clotting, manifested by thrombosis,
- thrombophilia - a tendency to form blood clots.
Assessment of blood coagulation: hemostasiogram (coagulogram). Contents of blood cellular elements. Cellular elements (platelets, erythrocytes, leukocytes) ensure the formation of a primary plug in the damaged area. Activation of cellular elements is an important factor in launching the plasma component of hemostasis. The inclusion of individual indicators of a general blood test in a hemostasiogram helps to correctly interpret deviations in the analysis and the clinical picture.
Screening tests for studying the plasma component of hemostasis - aPTT, prothrombin time, prothrombin according to Quick, INR, thrombin time, fibrinogen.
APTT or APTT (activated partial or partial thromboplastin time) is an assessment of the internal pathway of blood coagulation , the activator is phospholipids. The aPTT is the time required for plasma to clot when intrinsic pathway factors (calcium, phospholipids, and kaolin) are added.
Prolongation of APTT is observed with a deficiency of coagulation factors XII, XI, IX, VIII, kininogen, prekallikrein, factors V, X, prothrombin and fibrinogen, antiphospholipid syndrome, DIC syndrome.
A shortening of APTT is observed during hypercoagulation, including during pregnancy, in phase 1 of DIC syndrome.
The property of aPTT to lengthen with an excess of heparin makes it possible to monitor therapy with heparin-type drugs . Adequate prolongation of APTT is up to 2.5 times. If there is a change, it is important to monitor the aPTT when corrected with normal plasma. Thus, correction of an increased aPTT with normal plasma indicates that the concentration of blood coagulation factors in the plasma is reduced. Lack of correction may indicate the presence of blood clotting inhibitors (for example, lupus anticoagulant).
Prothrombin time is the time required for plasma to clot when calcium and tissue factor are added. The method reproduces the external pathway of blood coagulation with the assessment of the so-called prothrombin complex - factors VII, X, prothrombin. The extrinsic pathway involves vitamin K-dependent coagulation factors, so PT is used to evaluate indirect anticoagulant therapy.
There are two standard ways to present the results of this test:
- Prothrombin according to Quick reflects the content of coagulation factors as a percentage and serves to assess the external coagulation pathway.
- INR ( international normalized ratio). A comparison is made of the patient's blood coagulation with special plasma, normalized according to the international standard, which makes it possible to more reliably assess the state of the external pathway of plasma hemostasis in the patient. This is important for assessing the effect of drugs and selecting the dose.
Prolongation of PT (PT and INR increase, Prothrombin according to Quick decreases) may indicate a congenital deficiency of factors II, V, VII, X, liver diseases with impaired liver function, vitamin K deficiency (malabsorption, cholestasis, dietary habits, intestinal dysbiosis), treatment indirect anticoagulants, reduction or change in the structure of fibrinogen.
A shortening of PT (PC and INR decrease, Prothrombin according to Quick increases) indicates hypercoagulation, incl. during pregnancy and after childbirth, as well as when taking certain contraceptives.
Fibrinogen
- a blood protein that is synthesized in the liver. When blood clotting begins, fibrinogen polymerizes to form fibrin. An increase in fibrinogen concentration indicates a state of thrombophilia, observed with burns, in the last months of pregnancy, after childbirth, with myocardial infarction, and after surgery. In addition, the level of fibrinogen is increased during inflammatory processes and stress. A decrease in the amount of fibrinogen can be hereditary or acquired (liver dysfunction).
Thrombin time (TT) is the time during which fibrin is formed from fibrinogen. This indicator evaluates the rate of blood clotting when thrombin is added. The rate of fibrin formation depends on the quantity and quality of fibrinogen and the presence of anticoagulants in the blood.
TV increases with a decrease in fibrinogen concentration and changes in its molecule, the presence of inhibitors of fibrin formation, autoantibodies to thrombin, paraproteinemia, increased levels of fibrinogen/fibrin degradation products, the presence of heparin and other conditions. A decrease in TV is observed in the first stage of DIC syndrome and a significant increase in fibrinogen in the blood.
Thus, a competent comprehensive assessment of the APTT results, prothrombin time, thrombin time and fibrinogen indicators allows us to identify the presence of certain disorders, evaluate the effectiveness of the therapy, suspect the risk of thrombosis or bleeding, allows us to prescribe the necessary drugs and prevent drug overdose.
Anticoagulant system. Accidental activation of the coagulation mechanism is prevented by a special system, which includes several important proteins: antithrombin III, protein C and protein S. Adequate operation of the anticoagulant system is an important condition for maintaining the fluid state of blood inside the vessels. A decrease in the activity of anticoagulant factors can cause severe thrombotic complications. Our laboratory carries out the determination of antithrombin III and protein C.
Features of blood clotting during pregnancy
During pregnancy, a third circle of blood circulation appears - the placental one. The placenta is an organ that separates the mother and fetus. A special feature is that the placenta does not have a capillary link on the maternal side. Directly from the spiral arteries, the mother's blood enters the intervillous space and the chorion villi are washed with maternal blood. Through the veins of the deciduous membrane, blood returns back to the mother's bloodstream. That is, the placenta represents the boundary of interaction between two organisms, an aggressive phase that leads to the activation of thrombotic mechanisms. Hidden tendencies of impaired hemostasis appear in the arteries of the placenta with a greater degree of probability and lead to additional excessive blood clotting. Many pregnancy complications arise from thrombosis of the spiral arteries. During pregnancy, the activity of factors in the internal blood coagulation pathway increases, which is manifested by a shortening of the aPTT. During pregnancy, the amount of fibrinogen increases, the level of RCMP and D-dimers increases. Despite these changes, during normal pregnancy no pathological activation of hemostasis is observed; these changes are considered adaptive. It is advisable to assess blood coagulation at different stages of pregnancy. It is very important that the first blood clotting test is carried out early in pregnancy. Then the likelihood of risks when prescribing medications in a timely manner will be minimal. Excessive blood clotting leads to increased fibrin deposition in the placenta and premature aging of the placenta. Prescribing specific therapy makes it possible to slow down this process and prevent premature aging of the placenta.
Molecular genetic tests
A hemostasiogram is a screening test and reflects the state of blood coagulation at the time of blood donation. Therefore, a hemostasiogram may not show those risks whose mechanisms have not yet been activated. To assess the risks of thrombophilia, which is the cause of miscarriage, severe gestosis, myocardial infarction, stroke and other thrombosis, other studies are required. Hidden hereditary risk factors for blood clotting disorders pose a particular danger in obstetric and gynecological practice. At the moment of conception, each of us receives genetic material from our parents. This genetic material may carry genes that are associated with an increased risk of a particular condition. If both parents pass on such a gene, this condition is called homozygosity, if only one - heterozygosity. For some genes, a heterozygous state is sufficient; for others, a homozygous state is sufficient. In order to find out whether there are pathological genes and in what state they are (hetero- or homozygous), molecular genetic studies are carried out.
In the CIR Laboratory, the following molecular genetic studies are carried out to assess the risks of developing pathology in the hemostasis system:
- Polymorphism of genes of the hemostatic system - 12 factors, including the common Leiden mutation (f.V), prothrombin gene mutation, MTHFR mutation.
- Polymorphism of vascular tone genes . Vessels play an important role in the development of thrombosis and increased blood pressure (hypertension). An assessment of the risks of increased blood pressure must be carried out in case of miscarriage, antenatal fetal death, or in the presence of arterial hypertension in a woman or in relatives.
- Polymorphism of endothelial function genes . The lining of blood vessels, the endothelium, also plays a huge role in blood clotting. It is the endothelium that is the surface where a blood clot forms. Normally, the endothelium produces substances that prevent unnecessary blood clotting. But when the production of these substances is disrupted, thrombosis occurs.
You need to take these tests if you answer “yes” to at least one of these points:
- If there have been two or more fetal growth arrests in the past in early pregnancy
- with several unsuccessful IVF attempts (ART, IVF, ICSI, etc.)
- in the presence of severe pregnancy complications in the past (severe forms of late toxicosis of intrauterine fetal death, fetal growth retardation)
- when an increase in the level of antiphospholipid antibodies and/or an increase in the level of homocysteine is detected
- in the presence of a history of blood clotting disorders (thrombosis) in the presence of relatives with thrombotic complications under the age of 50 years (deep vein thrombosis, pulmonary embopia, stroke, myocardial infarction, sudden death)
Tags:
D-dimer, hemostasis, blood coagulation, pregnancy tests, miscarriage, mutations of the hemostatic system
Back to section
Increasing values (extending interval)
- Liver pathologies;
- Uremia (intoxication of the body due to kidney disease);
- DIC syndrome;
- Deficiency of protein intake in the body;
- Pathological pregnancy (miscarriage, placental abruption);
- Cardiovascular diseases (heart attack, stroke);
- Pneumonia (pneumonia);
- Hyperbilirubinemia (increased levels of bilirubin in the blood);
- Tuberculosis (infectious disease caused by Koch's bacillus);
- Hypofibrinogenemia (with the level of fibrinogen in the blood less than 0.5 g per 1 l) in acquired or congenital form;
- Dysfibrinogenemia (defect in the structure of fibrinogen at the molecular level);
- Paraproteinemia (presence of defective and abnormal protein compounds in the plasma);
- An increase in fibrin and fibrinogen breakdown products in the blood;
- The presence of anticoagulants in the plasma (antithrombins, hirudin, heparin and others);
- Fibrinolytic therapy (a type of treatment aimed at restoring blood flow by dissolving a blood clot);
- Development of autoimmune antibodies to thrombin;
- Production of lupus anticoagulant (antibodies against enzymes of the circulatory system);
- Myeloma multiforme (cancer of blood plasma cells) and other oncological processes.