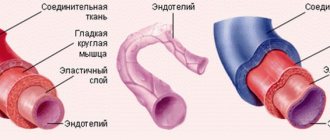
Human arteries and veins perform different jobs in the body. In this regard, significant differences can be observed in the morphology and conditions of blood flow, although the general structure, with rare exceptions, is the same for all vessels. Their walls have three layers: inner, middle, outer.
The inner shell, called intima, necessarily has 2 layers:
- the endothelium lining the inner surface is a layer of squamous epithelial cells;
- subendothelium - located under the endothelium, consists of connective tissue with a loose structure.
The middle shell consists of myocytes, elastic and collagen fibers.
The outer shell, called “adventitia,” is a fibrous connective tissue with a loose structure, supplied with vascular vessels, nerves, and lymphatic vessels.
The structure of the walls of veins and their difference from arteries
- The inner wall is lined with epithelial cells
- Average MMC
- External RVST, fixed to surrounding tissues.
Veins have a thinner wall: they expand easily and collapse easily.
There are valves - folds of the inner membrane - distributed unequally: less in the arms than in the legs, the rest above the confluence of the venous tributaries. Designed to prevent reverse blood flow and prevent stagnation in venous inflows. If the valve is not developed, then varicose veins, if stagnation, then a blood clot, and possible damage to the vessel.
The peculiarity of the hemodynamic conditions of the veins is low pressure (15-20 mm Hg) and low blood flow rate, which causes a lower content of elastic fibers in these vessels.
The number of muscle elements in the wall of these vessels depends on whether the blood moves with or against gravity.
Veins of the muscleless type are found in the dura mater, bones, retina, placenta, and red bone marrow. The wall of muscleless veins is lined internally with endothelial cells on the basement membrane, followed by a layer of fibrous SDTK; there are no smooth muscle cells.
Veins of the muscular type with weakly expressed muscular elements are located in the upper half of the body - in the system of the superior vena cava. These veins are usually in a collapsed state. The tunica media contains a small number of myocytes.
Veins with highly developed muscular elements make up the vein system of the lower half of the body. A feature of these veins is well-defined valves and the presence of myocytes in all three membranes - in the outer and inner membrane in the longitudinal direction, in the middle - circular direction.
Anatomy
Veins and arteries consist of three layers:
- Tunica adventitia : The outer layer of a blood vessel, composed of collagen and elastin. This layer allows the vessel to expand or contract, depending on the type of vein or artery. This function is important for controlling blood pressure.
- Tunica media : This is the middle of the blood vessel. Elastin and muscle fibers form the shell of the carriers. The amount of elastin or muscle varies depending on the type of blood vessel. For example, elastic arteries contain few muscle fibers in their membranes.
- Tunica Intima: This name refers to the inner layer of a blood vessel. It mainly contains elastic membranes and tissues and may include valves that help blood move in the right direction.
Functions of the venous system
Functions of veins:
- Transport of blood to the heart.
- Blood reservoir - deposition is facilitated by thin-walled, numerous veins (many in the abdominal cavity, they hold 80% of the blood in case of shock => GM, heart, liver, kidneys). In shock, blood pressure drops down to 0. The veins of the lungs can accumulate up to 28% of the blood, and swelling is possible due to inflammation.
- Regulates hemodynamics: blood flow speed, blood pressure provide blood supply, carried out reflexively. There are many receptors in the walls of the veins: chemo, mechano, baro. When they are irritated, reflexes are triggered:
- venovenous;
- venoarthrial (increased pressure, decreased arterial blood flow);
- venolymphatic.
- Participation in metabolic processes between blood and tissue. The walls of the capillaries are well permeable, metabolic processes are ensured by thin-walled venules, post-capillaries; with inflammation, permeability (swelling) increases, since the walls of the venules react to histamine.
Arteries
These are blood vessels that carry blood from the heart to all organs and tissues. There are arterioles and arteries (small, medium, large). Their walls have three layers: intima, media and adventitia. Arteries are classified according to several criteria.
Based on the structure of the middle layer, three types of arteries are distinguished:
- Elastic. Their middle layer of the wall consists of elastic fibers that can withstand the high blood pressure that develops during its release. This type includes the pulmonary trunk and aorta.
- Mixed (muscular-elastic). The middle layer consists of varying numbers of myocytes and elastic fibers. These include the carotid, subclavian, and iliac.
- Muscular. Their middle layer is represented by individual myocytes arranged in a circular pattern.
According to their location relative to the organs, arteries are divided into three types:
- Trunk – supply parts of the body with blood.
- Organ - carry blood to the organs.
- Intraorgan - have branches inside organs.
What connections between extra- and intracranial veins do you know? Their meaning
Extracranial: superficial, deep
Intracranial - GM veins, open in the sinuses of the dura mater, do not collapse, there are no valves. From the sinuses through the internal jugular vein is the main route for the outflow of venous blood from the cranial cavity.
Pathways of communication between intra- and extracranial veins:
- Through the venous outlet: 3 pairs, hole in the bones of the skull, blood from inside to outside
- The ophthalmic vein connects the cavernous sinus with the facial vein
- Through the diploe veins (the spongy substance of the skull bones between the plates)
- Through the foramen magnum into the vertebral venous plexuses
Physiology/hemodynamics
Normally, oxygenated blood leaves the left side of the heart through very large arteries. Which then branch into smaller and smaller arteries, then into arterioles and capillaries, which penetrate all organs and tissues of the human body. They are visible only under a microscope. The capillary bed connects the smallest arteries (arterioles) with the smallest veins (venules). Capillaries are very small vessels with very thin walls, thanks to which oxygen and nutrients easily flow from the blood into the tissues of the body. The tissues, in turn, release carbon dioxide and various waste products into the blood, which returns through the veins to the heart (Figure 1).
Picture 1.
Blood from the heart enters the large arteries (indicated in red), then it flows into smaller arteries and arterioles of the upper and lower extremities, as well as other organs and systems of the human body. Then the blood enters a network of tiny vessels - capillaries, which penetrate all human tissues and organs. The blood releases oxygen and various nutrients, and then returns through the veins (highlighted in blue) to the heart.
The venous system of the lower extremities consists of superficial and deep veins. Deep veins are large vessels through which the bulk of the blood moves due to the work of muscles. Superficial veins are smaller vessels that collect blood from the skin and subcutaneous tissue, and, due to the work of venous valves, move it upward, back to the heart. The superficial and deep veins communicate with each other through communicating or perforating veins, which are also equipped with valves. It is due to the operation of the valves that blood moves from the bottom up and from the superficial veins to the deep ones; such one-way movement is the key to the proper functioning of the veins.
Regulation of blood flow through the vessels is carried out by the nervous, endocrine system, as well as local vasoactive substances produced in tissues. This complex regulation allows blood flow to increase or decrease depending on the body's needs, for example, increased blood flow in the muscles during exercise, and decreased at rest. By changing the tone of skin vessels, body temperature is regulated. When it is cold, the blood vessels in the skin constrict, blood moves closer to the center of the body, due to this mechanism the body retains heat. On the contrary, when it is hot, the blood vessels in the skin dilate and the body gives off more heat. Various body injuries and injuries trigger processes that can cause blood flow to increase or decrease, for example, in the area of a skin burn or in a sprained area.
The walls of the veins are very thin and pliable, so the venous system can change its capacity to accommodate different amounts of blood. Blood volume is proportional to the pressure inside the veins. When the amount of blood in the veins decreases or its pressure on the vein walls decreases, the veins collapse like an empty balloon. When the volume of blood or its pressure on the walls of the vein increases, the veins expand, like an inflated balloon. If the pressure in the veins becomes very high, the venous wall stretches, its permeability increases and the vein allows fluid to pass through, which rushes into the tissue. This is how swelling occurs.
To maintain normal blood circulation in the body, the following 4 components are very important:
- Normal functioning of the heart, which, when contracting, works like a pump
- Pressure gradient between areas of low and high venous pressure
- “Muscular-venous pump” - the muscles of the lower extremities contract and work like a pump, pushing blood to the heart
- Normal, non-dilated, completely patent veins, with functioning venous valves
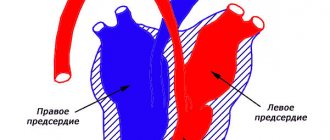
(1) The heart is the main pump of the human circulatory system. Blood moves through the arteries due to rhythmic heart contractions. It is important to understand that venous blood, after returning to the heart, must be pumped to the lungs, where it is enriched with oxygen. If the vein does not perform this function, as happens with heart failure, then venous blood stagnates and edema can appear even with absolutely normal veins.
(2) According to the laws of physics, any liquid moves from a high pressure zone to a lower pressure zone. The pressure difference between different zones is called gradient. There are such zones in the human body, thanks to which blood can move against the force of gravity. For example, the pressure in the veins of the lower extremities is higher than in the veins of the pelvis and abdominal cavity, and in the right parts of the heart it is even lower and may even be negative, which is why venous blood moves towards the heart. With some diseases of the lungs and heart, the pressure in the right parts of the heart may be increased, which can also lead to edema.
(3) “Muscular-venous pump” - like the heart, which pumps blood through the arteries, the muscles of the lower extremities contract to pump blood through the veins. The most important muscles performing the pumping function are the gastrocnemius muscles. There is also a venous network in the foot area; the muscles and ligaments of the foot also act as an additional pump. With each step, the muscles of the foot and lower leg contract rhythmically, pushing blood through the veins towards the heart, overcoming the effects of gravity. If a person leads a sedentary lifestyle and there is not enough activity in his life, the muscular-venous pump ceases to function normally and edema may appear. It can also occur as a result of injury or after a stroke. Sometimes the gait of older people changes, it becomes shuffling, the old people seem to shift from one foot to another. In this case, the muscular-venous pump also stops working and swelling may appear.
(4) Most veins in the human body are equipped with valves that allow blood to flow in only one direction. For the normal functioning of the venous system, the valves must be intact, that is, not damaged, and functioning correctly. As a result of contraction of the leg muscles, a portion of blood moves up through the veins, the valves allow blood to pass upward, and immediately close. They work like the rungs of a ladder, allowing blood to move forward towards the heart.
Figure 2.
The work of the “muscular-venous pump” is similar to a pump that pumps blood from the lower extremities to the heart. Due to the many valves with which the veins of the lower extremities are equipped, blood moves only in one direction: from the more superficial layers to the deep ones and from bottom to top, towards the heart. (a) When muscles contract, blood is forced out of the veins and moves upward. (b) When the muscles relax, the valves close, preventing blood from flowing back.
Each venous valve consists of two thin elastic flaps located opposite each other, opening and closing synchronously. If the vein dilates more than normal, as happens with varicose veins, the valve flaps cannot close and block the lumen of the vein, as a result, the blood moves in the opposite direction - this is called reflux. The flow of blood through a vein can also be disrupted if a blood clot forms that blocks the lumen of the vein. In both cases, venous pressure increases significantly, the vein wall becomes thinner as it stretches, and the liquid part of the blood seeps into the tissue, causing swelling. Edema is one of the main signs (symptoms) of improper functioning of the venous system.
If venous outflow is disrupted for a short time, for example after an air flight or prolonged static exercise, the main manifestation is swelling, which completely disappears overnight. If venous edema persists for a long time, for months, the skin and subcutaneous tissue begin to change, thickening and darkening may appear in the lower leg area, and subsequently infection, erysipelas, and microbial eczema may occur. All this can lead to the formation of long-term non-healing trophic ulcers.
Around which organs are the periorgan venous plexuses more developed? Their meaning
In many places there are well-developed venous plexuses:
- Small pelvis,
- spinal canal,
- Around the bladder
The significance of these plexuses can be seen in the example of the intravertebral plexus. When filled with blood, it occupies those free spaces that are formed when cerebrospinal fluid is displaced when changing body position or during movements. Thus, the structure and location of the veins depends on the physiological conditions of blood flow in them.
The cardiovascular system
The cardiovascular system connects the heart and blood vessels together. The system forms a closed circuit of vessels that transport blood throughout the body.
The cardiovascular system is essential for maintaining life. This is the first major network of organs to develop in embryos.
All body tissues need oxygen and nutrients to survive. They also require the removal of waste, which is a byproduct of metabolism.
Blood is needed both to provide oxygen and nutrients and to remove waste from tissues.
The heart pumps blood throughout the body. It must work constantly and with sufficient force so that all tissues of the body receive enough blood to function. Cardiovascular disorders can have serious consequences.
Cardiovascular diseases are a group of disorders that affect the heart and blood vessels, such as coronary heart disease.
These diseases are the leading cause of death worldwide, accounting for approximately 17.9 million deaths in 2021.