Circulation
Venous blood (with a low oxygen content) enters the right atrium through the superior and inferior vena cava. The blood then enters the right ventricle, which contracts and pumps it into the pulmonary trunk. The trunk soon divides into the right and left pulmonary arteries, which carry blood to both lungs. The arteries, in turn, break up into lobar and segmental branches, which are further divided into arterioles and capillaries. In the lungs, venous blood is cleared of carbon dioxide and, enriched with oxygen, becomes arterial. It enters the left atrium through the pulmonary veins and then into the left ventricle. From there, under high pressure, the blood is pushed into the aorta, then goes through the arteries to all organs. The arteries branch into smaller and smaller ones and eventually become capillaries. The speed of blood flow and its pressure by this time are significantly reduced. Oxygen and nutrients enter the tissues through the walls of the capillaries from the blood, and carbon dioxide, water and other metabolic products enter the blood. After passing through the network of capillaries, the blood becomes venous. The capillaries merge into venules, then into increasingly larger veins, and eventually the two largest veins - the superior and inferior vena cava - flow into the right atrium. As long as we are alive, this cycle repeats itself over and over again.
Table of contents
- Etiology and pathogenesis
- Clinical manifestations
- Principles of treatment
Deep-lying vessels are pathologically altered capillaries that feed hemangiomas and malformations, as well as enlarged venules located in the skin at a depth of up to 5 mm.
In our company you can purchase the following equipment for removing deep-lying vessels:
- M22 (Lumenis)
Conditions in which deep-lying vessels are present in the skin include the following:
- Infantile hemangiomas
- Capillary hemangiomas
- Cavernous hemangiomas
- Vascular malformations
- Phlebeurysm
Different functions - different structure.
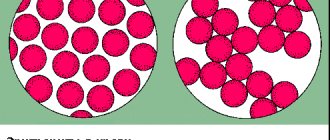
The highest blood pressure will be at the blood outlet from the heart (in the left ventricle), slightly lower pressure will be in the arteries, even lower in the capillaries, and the lowest in the veins and at the entrance of the heart (in the right atrium).
The arteries carrying the oxygenated blood pushed out by the heart must resist the high pressure in the circulatory system. That's why they have an elastic membrane. In addition, they must also change their lumen in order to vary the level of blood flow in different organs in response to the actions of the autonomic nervous system - for this they have a well-developed layer of smooth muscle tissue. Therefore, the walls of the arteries are much thicker than the venous ones, they are much more elastic and contain a large number of muscle elements.
The walls of the veins, in turn, are thin and pliable, contain virtually no muscle elements, and ensure the return of blood to the heart. The veins in the lower body have valves that prevent blood from flowing back. Thus, the vascular bed adapts to changing load levels mainly due to changes in the lumen of the arteries.
Clinical manifestations
Infantile hemangiomas
The earliest sign of infantile hemangioma is blanching of the skin (possibly with small telangiectasias), which later transforms into a red or crimson spot ( Fig. 7 ). A characteristic feature is the rapid growth of the tumor in the first 4 weeks of a child’s life. It usually grows faster than the newborn itself, which distinguishes it from vascular malformations, which increase in proportion to the growth of the infant.
Infantile hemangioma may become convex or dome-shaped, acquire a lobulated structure, or remain flat. During the first year of a child’s life, the phase of tumor proliferation occurs, with its greatest increase recorded in the first 4–6 months.
The involutive phase of infantile hemangioma can be short or long, and this is impossible to predict in advance. But it is reliably known that of all lesions that have resolved by the 6th year of a child’s life, 38% leave behind scars, telangiectasia, or anetodermic (atrophic) skin. If the hemangioma resolves after 6 years, these residual effects are recorded in 80% of cases. It has also been observed that infantile hemangiomas, which take longer to develop, have a higher incidence of residual skin lesions.
Rice. 7. Infantile hemangioma on the forehead ( a ), scalp ( b ), cheek ( c ) and upper lip ( d ) (Itinteang T., et al. Biology of infantile hemangioma. Frontier Surg 2014; 1)
Capillary hemangiomas
Typically these are red spots of progressive size in the periorbital area. Hemangiomas turn white when pressed, unlike port-wine stains, whose color does not change. Due to the extent of the tumor, the child may be unable to open the affected eye ( Figure 8 ). A decrease in visual acuity on the affected side is typical - amblyopia is observed in 43–60% of patients.
Rice. 8. Capillary hemangioma of the lower eyelid (Kavoussi SC, et al. Spontaneous periocular ecchymosis in children: Differential diagnosis and current trends in evaluation and manangement. J Clin Exp Ophthalmol 2014; 5: 1–10)
Cavernous hemangiomas
They are neoplasms located deep in the skin, which appear as a bluish swelling on the arm or other area of the body ( Fig. 9 ). They can have a small diameter or reach large sizes.
Rice. 9. Cavernous hemangioma in the periauricular area (Skintags Removing)
Vascular malformations
A port-wine stain ( capillary malformation ) first appears as a light pink or pink area that, upon closer inspection, consists of individual vascular branches. Most malformations are located on the face or neck, in 45% occupying from 1 to 3 areas innervated by the trigeminal nerve, and in 55% they can move to the opposite side of the face.
As the child grows, the port-wine stain increases in size, becoming light red or completely red ( Figure 10 ). At the same time, it looks like a continuous network of vessels, where it is impossible to identify individual branches. Malignancy of a port-wine stain is possible with degeneration into a cancerous tumor.
Rice. 10. Port-wine stain as an adult (Instagram.com/birthmarksbeauty)
Venous malformations appear as soft, bluish-colored lesions that typically occur on the face, extremities, or trunk ( Figure 11 ). They are dependent lesions, i.e. expand and contract depending on the patient's position. Venous malformations are prone to thrombosis, resulting in phleboliths, which in this case are a pathognomonic symptom.
Lymphatic malformations occur from birth and appear as small, dome-shaped nodules that are reddish in color due to slight bleeding. Based on the size of the lymphatic chambers, they are divided into macrocystic (> 2 cm), microcystic (<2 cm) and mixed. Macrocystic lymphatic malformations can significantly increase in size ( Fig. 12 ), leading to bone deformation and disfigurement of the child's face.
Rice. 11. Venous malformation of the face (Craniofacial team of Texas)
Rice. 12. Lymphatic malformation in the neck (Dr. P. Marazzi/Science Photo Library)
https://www.merckmanuals.com/
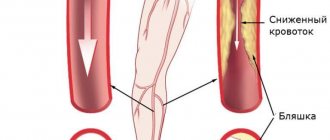
Phlebeurysm
Clinical manifestations are extremely varied - from small venous telangiectasias (“spider veins”) to large protrusions of large veins under the skin, with ulcers and necrosis. If we talk about a mild degree of the disease, which can be cured non-surgically, venous telangiectasias are divided into tree-like (branching), arachnid (stellate), linear (simple), spotted (pantiform). In the absence of therapy, they gradually spread throughout the skin ( Fig. 13 ), after which large and deep vessels can be affected with the addition of various complications.
Rice. 13. Telangiectasia on the thigh (Primary Care Dermatology Society)
Principles of treatment
The choice of treatment method should begin with a thorough assessment of the patient's condition. Based on this, it should be determined whether a particular method can solve the identified problem.
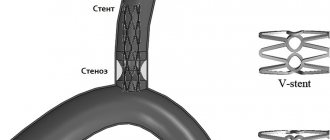
To treat deep-lying vessels, including those feeding hemangiomas and malformations, sclerotherapy - the introduction of a special substance into the vascular lumen, which causes destruction of the endothelium with the subsequent formation of a thin fibrous cord. In this way, vessels with a diameter of 4 mm or more can be eliminated.
The “gold standard” for removing small superficial vessels with a depth of up to 5 mm is the Nd : YAG laser . Its radiation has an optimal penetration depth and is well absorbed by blood hemoglobin. Laser therapy procedures are carried out without compromising the integrity of the skin, are well tolerated and do not require long-term rehabilitation. Nd:YAG laser can be combined with sclerotherapy or surgical removal of large and deep-lying vessels.
In the case of deep-lying vessels, they are often “covered” by a network of surface capillaries, which absorbs part of the laser radiation. Therefore, a combination of intense pulsed light (IPL) and a 1064 nm Nd:YAG laser is used for effective therapy. Both of these modules are part of the universal M22 platform from Lumenis.
Questions from our users:
- deep vessels removal
- remove blood vessels with laser
- vessels after laser resurfacing
- blood vessels treatment