A little about the circulatory system
The human circulatory system has a complex structure; biological fluid circulates in the pulmonary and systemic circulation.
The heart, which acts as a pump, consists of four sections - two ventricles and two atria (left and right). The vessels that carry blood from the heart are called arteries, and the vessels that carry blood to the heart are called veins. The arterial one is enriched with oxygen, the venous one – with carbon dioxide.
Thanks to the interventricular septum, venous blood, which is located on the right side of the heart, does not mix with arterial blood, which is on the right side. Valves located between the ventricles and atria and between the ventricles and arteries prevent it from flowing in the opposite direction, that is, from the largest artery (aorta) to the ventricle, and from the ventricle to the atrium.
When the left ventricle, whose walls are the thickest, contracts, maximum pressure is created, oxygen-rich blood is pushed into the systemic circulation and distributed through the arteries throughout the body. In the capillary system, gases are exchanged: oxygen enters the tissue cells, carbon dioxide from the cells enters the bloodstream. Thus, the arterial becomes venous and flows through the veins into the right atrium, then into the right ventricle. This is a large circle of blood circulation.
Next, the venous blood flows through the pulmonary arteries into the pulmonary capillaries, where it releases carbon dioxide into the air and is enriched with oxygen, again becoming arterial. Now it flows through the pulmonary veins into the left atrium, then into the left ventricle. This closes the pulmonary circulation.
Venous blood is located in the right side of the heart
General information
For some reason, almost all people are sure that arterial blood is the type that flows in arterial vessels. In fact, this opinion is wrong. Arterial blood is enriched with oxygen, which is why it is also called oxygenated. It moves from the left ventricle to the aorta, then goes through the arteries of the systemic circulation. After the cells are saturated with oxygen, the blood turns into venous and enters the veins of the BC. In a small circle, arterial blood moves through the veins.
You may be interested in: Aromatase inhibitors: purpose and list of drugs
Different types of arteries are located in different places: some are deep in the body, while others allow you to feel the pulsation.
Venous blood moves through the veins into the CD and through the arteries into the MC. There is no oxygen in it. This liquid contains a large amount of carbon dioxide, decay products.
Characteristics
Venous blood differs in a number of parameters, ranging from appearance to the functions it performs.
- Many people know what color it is. Due to its saturation with carbon dioxide, its color is dark, with a bluish tint.
- It is poor in oxygen and nutrients, but it contains a lot of metabolic products.
- Its viscosity is higher than that of oxygen-rich blood. This is explained by an increase in the size of red blood cells due to the entry of carbon dioxide into them.
- It has a higher temperature and lower pH level.
- Blood flows through the veins slowly. This is due to the presence of valves in them, which slow down its speed.
- There are more veins in the human body than arteries, and venous blood overall accounts for approximately two-thirds of the total volume.
- Due to the location of the veins, it flows close to the surface.
Function
Blood has specific and general functions. The latter include:
- nutrient transfer;
- transport of hormones;
- thermoregulation.
Venous blood contains a lot of carbon dioxide and little oxygen. This difference is due to the fact that oxygen enters only the arterial blood, while carbon dioxide passes through all vessels and is contained in all types of blood, but in different quantities.
How to determine the type of bleeding
Visually, this is quite easy to do: the blood from the vein is dark, thicker and flows out in a stream, while the arterial blood is more liquid, has a bright scarlet hue and flows out like a fountain.
External differences between venous and arterial bleeding
Venous bleeding is easier to stop; in some cases, if a blood clot forms, it may stop on its own. A pressure bandage placed below the wound is usually required. If a vein in the arm is damaged, it may be enough to raise the arm up.
As for arterial bleeding, it is very dangerous because it will not stop on its own, the blood loss is significant, and death can occur within an hour.
Detailed description of the study
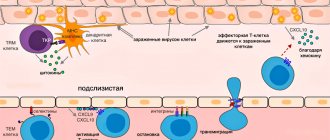
One of the mechanisms of immune defense is normally the production of antibodies - immunoglobulins, Ig - which belong to the gamma globulin fraction of blood serum proteins. By their nature, antibodies are glycoproteins - molecules containing carbohydrate and protein - and are divided into five classes: IgA, IgM, IgG, IgE, IgD. They differ in structure and functions, but have a similar structure. When immunoglobulins react to molecules of the body's own, they are called autoantibodies.
Antiphospholipid syndrome (APS) is an autoimmune disease that includes recurrent thrombosis and obstetric pathology. APS is based on the synthesis of antiphospholipid antibodies and their thrombus-stimulating effect. These immunoglobulins come in several types.
Antiphospholipid syndrome is one of the types of acquired thrombophilias. Thrombophilias are conditions in which thrombosis of blood vessels develops. With APS, blood clots occur both in the venous and arterial beds and can recur (recur) in 70-80% of cases in the same place. Deep vein thrombosis is dangerous due to the high risk of developing embolism - blockage - of the pulmonary vessels.
Thrombocytopenia may also occur with antiphospholipid syndrome. Thrombocytopenia is a condition in which the number of platelets in the blood is less than 150 × 109/L. People with thrombocytopenia have an increased risk of bleeding and bleeding. Numerous small purple spots may appear on the skin, which is why the disease is called thrombocytopenic purpura.
There are primary and secondary APS. The first is diagnosed when the reason causing the increase in antiphospholipid antibodies is unknown. The second is isolated when the underlying disease is known, which causes an increase in the formation of these immunoglobulins and is often associated with chronic stimulation of the immune system. The main four groups of reasons for stimulation are:
- Autoimmune diseases;
- Medications;
- Infectious diseases: viral and bacterial, the production of antiphospholipid antibodies is especially common in HIV infection and syphilis;
- Malignant tumors.
A number of drugs increase the concentration of antiphospholipid antibodies, including phenothiazines and other drugs that cause drug-induced lupus: chlorpromazine, hydralazine, phenytoin, procainamide and quiniline.
Antiphospholipid antibodies increase in both viral and bacterial infections. However, with them the increase is transient - short-term - and their appearance should be distinguished from APS.
Obstetric pathology in APS is associated with miscarriage. Miscarriage caused by an increased concentration of antiphospholipid antibodies is possible at any stage, but more often occurs in the second or third trimester. Fetal death is a consequence of thrombus formation in the small vessels of the placenta, due to which the latter ceases to perform its functions and further pregnancy becomes impossible.
A comprehensive study for APS includes the following groups of antiphospholipid antibodies:
AT to cardiolipin.
Cardiolipin is a phospholipid that is part of biological membranes, namely, it is found in the mitochondrial membrane, one of the cell structures where it participates in metabolic processes. In antiphospholipid syndrome, immunoglobulins are produced in response to cardiolipin, so their determination with the appointment of the appropriate analysis is one of the main points in the correct diagnosis.
AT to phospholipids.
These autoantibodies are aimed at damaging the main components of the biological membranes of human cells. These components are phospholipids. Of these molecules, the most antibodies are produced to phosphatidylserine, which is located on the inner surface of platelets and on the membranes of the cells of the inner layer of blood vessels (endothelium). Phosphatidylserine takes an active part in the formation of a blood clot (thrombus), and when antibodies to this molecule are produced, inadequate thrombus formation occurs.
Lupus anticoagulant (LA).
VA is a group of antibodies to phospholipids, which also increase the risk of blood clots. It was first isolated from patients with systemic lupus erythematosus, but is currently included in one of the criteria for defining antiphospholipid syndrome.
Antibodies to beta-2 glycoprotein.
These ATs are one of the main markers of APS. Their identification in cases of suspected APS is recommended by Russian and foreign clinical guidelines. Beta-2 glycoprotein immunoglobulins are often associated with secondary antiphospholipid syndrome secondary to systemic lupus erythematosus.
Antibodies to prothrombin.
Prothrombin is a protein involved in blood clotting processes. Antibodies to it directly contribute to the development of APS symptoms.
This analysis can determine the presence of APS with a high degree of probability, is widely used in clinical practice, is affordable and has no absolute medical contraindications. Venous blood must be donated for testing.
A detailed description of the studies and reference values are presented on the pages with descriptions of individual studies.
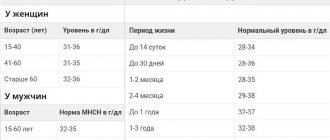
When do you need to take a General blood test without leukocyte formula (venous blood)?
- To assess general health (routine medical examinations, screening examinations, etc.);
- For diagnostics at the first stage of a wide range of diseases that may manifest themselves as changes in the characteristics of peripheral blood;
- Diagnosis of anemia, polycythemia along with the study of hemoglobin and hematocrit;
- Monitoring ongoing drug treatment for patients suffering from bleeding or chronic anemia;
- Determination of the activity of erythrocyte formation processes in the bone marrow.
References
- Guyton, A.K., Hall, J. Medical physiology / ed. IN AND. Kobrina. - M.: Logosphere, 2008. - 1296 p.
- Internal diseases in 2 volumes: textbook / ed. ON THE. Mukhina, V.S. Moiseeva, A.I. Martynova, 2010. - 1264 p.
- Secrets of rheumatology. - St. Petersburg: BINOM Publishing House, 1999. - 768 p.
- Reshetnyak, T.M. Antiphospholipid syndrome: diagnosis and clinical manifestations (lecture). Scientific and practical rheumatology, 2014. - No. 1.
- Federal clinical guidelines. Laboratory diagnosis of rheumatic diseases, 2014. - 12 p.
- Makarenko, E.V. Antiphospholipid syndrome. Problems of health and ecology, 2021. - No. 4 (54).
- Miyakis, S., Lockshin, M., Atsumi, T. et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J ThrombHaemost, 2006. - Vol. 4(2). - P. 295-306.