Auscultation of the heart is usually carried out sequentially: in a supine (on the back), in a standing position of the patient, and also after physical activity (gymnastics). To ensure that respiratory sounds do not interfere with listening to sounds of cardiac origin, before listening, it is necessary to ask the patient to inhale, exhale completely and then hold his breath in the exhalation position. This technique is especially important for beginners in the study of auscultation.
Auscultation of the heart is preferably done indirectly, with a stethoscope. Due to the fact that individual places for listening to the heart are located at a very close distance from each other, direct auscultation with the ear is used in exceptional cases to complement the mediocre one. To correctly assess auscultation data, you need to know the places of projection of the heart valves on the chest wall and the best places to listen to them, since sound vibrations depend not only on the proximity of the valve apparatus, but also on the conduction of these vibrations along the blood flow.
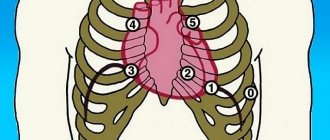
Projection of the valves onto the chest: 1. The pulmonary valve lies behind the cartilage of the third left rib, near the sternum and partly behind it; 2. The aortic valve lies behind the sternum immediately below and deeper than the opening of the pulmonary trunk; 3. The mitral valve is projected at the site of attachment to the sternum of the cartilage of the fourth left rib; 4. The tricuspid valve lies behind the sternum almost in the middle between the places of attachment of the cartilages of the V right and III left ribs. In healthy people, during auscultation of the heart, two tones can be clearly heard: the first sound, which occurs during systole, is systolic, and the second sound, which occurs during diastole, is diastolic.
Beginning clinicians need to accustom themselves to systematically paying attention to all the features of sound phenomena and pauses. The first task is the orienting determination of the first tone, since the sound cycle of the heartbeat begins with it. Then all four openings of the heart are heard in sequential order.
Listening sites: The most distinct tone of the mitral valve is heard at the apex of the heart (1.5 - 2.0 cm medially from the left midclavicular line), the pulmonary valve - in the second left intercostal space at the edge of the sternum, the tone of the aorta - at the edge of the sternum in the second right intercostal space , tricuspid valve - at the base of the xiphoid process of the sternum; the aortic valve is also heard at the attachment site of the III-IV ribs - Botkin-Erb point (V point of auscultation). Listening to the valves is carried out in the specified sequence, corresponding to a decrease in the frequency of their damage. For each subject it is necessary to determine: 1. strength or clarity of tones;
2. timbre of tones;
3. frequency,
4. rhythm;
5. presence or absence of noise.
When listening to a healthy heart, two tones are heard, periodically replacing each other. Starting auscultation of the heart from the apex, we hear:
1. short, stronger sound - first tone,
2. short first pause,
3. weaker and even shorter sound - second tone
4. a second pause, twice as long as the first.
The first tone, in contrast to the second, is somewhat longer, lower in tone, stronger at the apex, weaker at the base, and coincides with the apical impulse. It is more convenient for beginners to distinguish the first tone from the second, focusing on a short pause, i.e., guided by the fact that the first tone is heard before it, or, in other words, a short pause follows the first tone. In the case of a frequent heart rhythm, when it is not possible to clearly differentiate the tones, you need to place the fingers of your right hand at the site of the apical impulse (or to the carotid artery in the neck) while listening. The tone that matches the impulse (or the carotid pulse) will be the first. It is impossible to determine the first heart sound by the pulse on the radial artery, since the latter is delayed in relation to the first heart sound.
The first tone is formed from 4 main components:
1. Atrial component - associated with vibrations of the atrial myocardium. Atrial systole precedes ventricular systole, so normally this component merges with the first sound, forming its initial phase.
2. Valvular component - oscillation of the atrioventricular valve leaflets in the contraction phase. The magnitude of the oscillations of the leaflets of these valves is influenced by intraventricular pressure, which in turn depends on the speed of contraction of the ventricles.
3. Muscular component - also occurs during the period of ventricular contraction and is caused by myocardial vibrations.
4. Vascular component - formed due to vibrations of the initial parts of the aorta and pulmonary trunk during the period of expulsion of blood from the heart.
The second sound, which occurs at the beginning of diastole, is formed by 2 main components: 1. Valve component - slamming of the aortic and pulmonary valves. 2. Vascular component - vibration of the walls of the aorta and pulmonary trunk.
The third tone is caused by vibrations that appear during rapid relaxation of the ventricles, under the influence of the flow of blood flowing from the atria. This tone can be heard in healthy people, mainly in young people and adolescents. It is perceived as a weak, low and dull sound at the beginning of diastole, 0.12-0.15 s from the beginning of the second tone.
The fourth tone precedes the first sound and depends on the oscillations that occur during atrial contraction. For children and adolescents it is considered physiological; its appearance in adults is pathological.
The third and fourth sounds are better heard during direct auscultation and are clearly identified when recording a phonocardiogram. The detection of these tones in elderly people, as a rule, indicates severe myocardial damage.
Auscultation rules
Basic rules for cardiac auscultation:
- maintaining silence, warm room;
- carried out in a horizontal and vertical position of the patient, and, if necessary, after physical therapy. loads;
- listen to the heart both during quiet shallow breathing of the patient and when holding the breath after maximum exhalation.
Auscultation rules
Sound phenomena associated with the pathology of the mitral valve are listened to in a position on the left side, and the aortic valve - in a vertical and tilted forward position with arms raised up.
Projection of the heart valves on the anterior chest wall:
- The projection of the bicuspid valve is on the left side of the sternum in the area of attachment of the third rib;
- The projection of the tricuspid valve is on the sternum, in the middle of the distance between the place of attachment to the sternum of the cartilage of the third rib on the left and the cartilage of the fifth rib on the right;
- The pulmonary valve is projected into the second intercostal space to the left of the sternum;
- The aortic valve is located in the middle of the sternum at the level of the third costal cartilage.
To synchronize sound phenomena with the phases of systole and diastole, it is necessary to simultaneously palpate the patient’s right carotid artery with the left hand, the pulsation of which practically coincides with ventricular systole.
Heart auscultation points
- Sound phenomena associated with the activity of the mitral valve are better transmitted to the apex of the heart;
- In the second intercostal space to the right of the sternum - sounds of the aortic valve;
- In the second intercostal space to the left of the sternum - sounds from the pulmonary valve;
- At the base of the xiphoid process, sound phenomena resulting from the operation of the tricuspid valve are better determined;
- The fifth point—Botkin-Erb point, in the IV intercostal space—serves for additional auscultation of the mitral and aortic valves
Cardiac cycle
The heart beats at a rate of sixty to eighty beats per minute. This, of course, is an average value, but ninety percent of people on the planet fall under it, which means it can be taken as the norm. Each beat consists of two alternating components: systole and diastole. The systolic heart sound, in turn, is divided into atrial and ventricular. This takes 0.8 seconds, but the heart has time to contract and relax.
Heart sounds
I (systolic) tone occurs predominantly in the phase of isovolumetric contraction of the ventricles of the heart.
Components of the first heart sound
- valve component;
- gastric or muscular (sharp rise in pressure in the ventricle during isovolumetric contraction);
- vascular (oscillations of the initial sections of the great vessels when they are stretched by blood in the expulsion phase);
- atrial (oscillations associated with contraction of the atria).
II (diastolic) heart sound occurs at the very beginning of ventricular diastole due to:
- slamming of the semilunar leaflets of the aortic valve and pulmonary trunk (valvular component);
- vibrations of the walls of the initial sections of these vessels (vascular component).
Change in heart sounds
- changing the volume of the main tones (I and II);
- splitting (bifurcation) of basic tones;
- appearance of additional tones:
- III and IV tones,
- sounds of mitral valve opening,
- additional systolic sound (click)
- and the so-called pericardial tone.
The volume of the first tone normally depends on the following factors:
- From the tightness of the ventricular chamber during the period of isovolumetric contraction (from the tightness of the closure of the atrioventricular valves);
- From the speed and force of contraction of the ventricles in the phase of isovolumetric contraction, which is determined by:
- intensity and speed of metabolic processes in the myocardium (contractility of the heart muscle);
- on the density of structures involved in oscillatory movements, primarily on the density of atrioventricular valves;
- from the position of the atrioventricular valve leaflets immediately before the onset of the isovolumetric contraction phase.
The volume of the second tone normally depends on the following factors:
- from the tightness of the closure of the semilunar valves of the aorta and pulmonary artery;
- on the rate of closure and oscillation of these valves during the protodiastolic period, which in turn depends on:
- blood pressure level in the main vessel,
- on the density of the structures involved in oscillatory movements, primarily on the density of the semilunar valves, as well as the walls of the great vessels;
- from the position of the semilunar valve leaflets immediately before the onset of the protodiastolic period.
Reasons for weakening of the first tone:
- leaky closure of the atrioventricular valves (with mitral or tricuspid valve insufficiency);
- a sharp slowdown in ventricular contraction and rise in intraventricular pressure with a decrease in myocardial contractility in patients with heart failure and acute myocardial damage;
- a significant slowdown in the contraction of the hypertrophied ventricle ( with stenosis of the aortic mouth);
- unusual position of the atrioventricular valve leaflets immediately before the onset of isovolumetric contraction of the ventricles.
Strengthening the 1st tone:
Causes:
- An increase in the rate of isovolumetric contraction of the ventricles (with tachycardia or thyrotoxicosis, when the rate of all metabolic processes in the body, including the heart, increases);
- Compaction of the heart structures involved in vibrations and the formation of the first sound (with mitral stenosis).
A loud (popping) first heart sound with mitral stenosis is caused both by the compaction of the leaflets of the mitral valve itself, the oscillations of which occur with greater frequency, and by a change in the rate of contraction of the left ventricle and the shape of the intraventricular pressure curve.
Reasons for weakening of the second heart sound:
- violation of the tightness of the closure of the semilunar valves of the aorta and pulmonary artery;
- decrease in the speed of closing of the semilunar valves with:
- HF accompanied by a decrease in the rate of ventricular relaxation
Strengthening (emphasis) of the second heart sound
Causes of enhancement in the aorta:
- increased blood pressure of various origins (due to an increase in the rate of slamming of the aortic valve leaflets);
- compaction of the aortic valve leaflets and aortic walls (atherosclerosis, syphilitic aortitis).
Causes of enhancement in the pulmonary artery:
1) increased pressure in the pulmonary artery (with mitral stenosis, cor pulmonale, left ventricular heart failure).
Split heart sounds:
The main cause of splitting of the first heart sound is asynchronous closure and fluctuations of the mitral (M) and tricuspid (T) valves (right bundle branch block).
Additional heart sounds
The third heart sound occurs at the end of the phase of rapid filling of the ventricles after 0.16 - 0.20 seconds. after the second tone. It is caused by a hydraulic shock against the wall of the ventricle of a portion of blood moving under the influence of a pressure gradient from the atrium to the ventricle.
IV heart sound occurs during active atrial systole, i.e. immediately before the first tone. It is caused by a hydraulic shock of a portion of blood from the atrium against the upper front of the blood that filled the ventricle during the previous phases of fast and slow filling.
The tone (click) of the opening of the mitral valve, together with the flapping I tone and the II tone accentuated on the pulmonary artery, form a peculiar melody of mitral stenosis, called the “quail rhythm” and reminiscent of the quail singing “it’s time to sleep.”
Diastole
Here, too, everything is not as simple as it might seem at first glance. Ventricular relaxation lasts 0.37 seconds and occurs in three stages:
- Protodiastolic: After blood has left the heart, the pressure in its cavities decreases and the valves leading to large vessels close.
- Isometric relaxation: the muscles continue to relax, the pressure drops even more and becomes equal to the atrial pressure. This causes the atrioventricular valves to open and blood from the atria enters the ventricles.
- Ventricular filling: Following a pressure gradient, fluid fills the lower chambers of the heart. When the pressure equalizes, the flow of blood gradually slows down and then stops.
Then the cycle repeats again, starting with systole. Its duration is always the same, but diastole can be shortened or lengthened depending on the speed of the heartbeat.
Heart murmurs
Heart murmurs are relatively long-lasting sounds that occur during turbulent blood flow.
3 hemodynamic parameters that determine the possibility of murmurs:
- Diameter of the valve orifice or lumen of the vessel;
- Blood flow speed (linear or volumetric);
- Blood viscosity.
Murmurs heard over the heart area are divided into:
- inside and extracardiac (intra- and extracardiac); organic and functional;
Intracardiac murmurs
- organic, arising as a result of gross organic damage to the valves and other anatomical structures of the heart (IVS and MPP);
- functional noises, which are not based on gross violations of anatomical structures, but on dysfunction of the valve apparatus, acceleration of blood movement through anatomically unchanged openings or a decrease in blood viscosity.
Organic noises
All organic intracardiac murmurs are formed when narrowing, dilation or other obstruction occurs in the area of the valve openings, in the cavities of the heart or in the initial sections of the great vessels.
When noise is detected, it is necessary to determine:
- the ratio of noise to the phases of cardiac activity (systolic, diastolic, etc.);
- duration of noise (short or long);
- timbre, noise volume in general and volume changes in the phase of the cardiac cycle;
- area of maximum noise auscultation;
- direction of noise;
- the form of noise from body position, breathing phases and physical activity.
Functional noise
- dynamic noises, which are based on a significant increase in blood flow velocity in the absence of any organic heart diseases (dynamic noises in thyrotoxicosis, cardiac neurosis, febrile states);
- anemic noises, the cause of which is a decrease in blood viscosity and some acceleration of blood flow in patients with anemia of various origins.
- Dynamic and anemic functional murmurs occur in the absence of any organic heart disease and are therefore called “innocent” murmurs.
- All functional (“innocent”) murmurs are systolic
- Innocent noises:
- are not constant, they change with changes in body position and breathing,
- short, short,
- are not carried out far from the place of maximum auscultation,
- not rough, more often soft, blowing, gentle noises,
- are not accompanied by sharp myocardial hypertrophy, dilatation of cavities and other signs of organic heart disease.
Extracardiac (extracardiac) murmurs
Pericardial friction noise occurs when the surface of the pericardial layers becomes uneven and rough. This is observed when:
- dry (fibrinous) pericarditis;
- aseptic pericarditis in patients with acute myocardial infarction;
- uremic pericarditis in patients with renal failure.
The pericardial friction noise is heard during systole and diastole and resembles the crunching of snow, the rustling of paper or grinding, scratching.
The pericardial friction murmur differs from intracardiac murmurs in the following ways:
- most often heard in a limited area, usually in the zone of absolute dullness of the heart, and is not carried out anywhere;
- intensifies when pressing with a stethoscope on the anterior chest wall;
- is a highly variable sound phenomenon;
- heard in both phases of cardiac activity (systole and diastole).
Pleuropericardial murmur occurs when the pleura immediately adjacent to the heart becomes inflamed due to friction of the pleural layers against each other, synchronously with heart contractions.
Pleuropericardial murmur should be distinguished from pericardial friction murmur by the following features:
- it is usually heard along the left edge of the relative dullness of the heart;
- intensifies at the height of a deep breath;
- weakens or disappears with maximum exhalation and breath-holding.
In Dahl's dictionary
m. French music every sound, ringing, hum, voice; and every change in sound is an increase or decrease in tone. Hit the tone, hit the given note. | music sound quality or language. Good and bad violin tone. This piano has a full, thick and soft tone. The tone of string instruments is sharper than that of wind instruments. | music mode, which is major (dur) and minor (mol), and in each there are also divisions, according to the number of notes; in our church music, tone and mode are replaced by voices. | Painter. the degree of brightness or dominance of one or another color or paint; commonality of paint, suit. | The commonality of a person’s speech and techniques, the way he treats people. A man of good taste, who knows all social decency. He speaks in the tone of a teacher, or a boss. Set the tone, show off, show off. | See ton. Tonic, main note, dominant sound, tonic note, main note in tone. Tonic meter of poetry, melodious, Russian, based on word (and not syllable) stress. | doctor. tonic spasms, from excessive muscle tension, opposite sex. clonic. - a drug for the nerves.
Determination of the properties of the arterial pulse
Properties of arterial pulse:
- synchronicity on both hands,
- condition of the vascular wall,
- frequency,
- rhythm,
- voltage,
- filling,
- size,
- form.
Pulsus differens is observed in unilateral obliterating diseases of large arteries and with external compression of large arterial vessels (aortic aneurysm, mediastinal tumor, enlargement of the left atrium with mitral stenosis, etc.).
Pulsus deficiens, pulse deficiency , i.e. the difference between the number of heart contractions and the pulse rate appears with certain heart rhythm disturbances (atrial fibrillation, frequent extrasystole, etc.) and indicates a decrease in the functionality of the heart.
Blood pressure measurement
Systolic blood pressure is the maximum pressure in the arterial system developed during left ventricular systole. It is determined mainly by the stroke volume of the heart and the elasticity of the aorta and large arteries.
Diastolic blood pressure is the minimum pressure in the arteries during cardiac diastole. It is largely determined by the magnitude of the tone of the peripheral arteries.
Pulse BP is the difference between systolic and diastolic BP.