Causes of B12 deficiency anemia
A lack of vitamin B12 may be due to the following reasons or a combination of them:
- impaired absorption of the vitamin in the intestine: gastritis associated with Helicobacter pylori infection, Crohn's disease, previous intestinal surgeries, polyposis of the gastric mucosa, cancer, intestinal fistulas, etc.;
- congenital metabolic disorders;
- chronic intoxication with nitric oxide, used as sedation in anesthesiology.
- minor absorption disorders, for example, a decrease in the availability of B12 in food with chronic pancreatitis, moderate atrophic gastritis, taking metformin, medications to reduce the production of hydrochloric acid, etc.;
- poor diet, vegetarianism;
- chronic alcoholism.
One form of B12 deficiency anemia is Addison-Biermer disease. With it, autoantibodies appear against the cells of the gastric mucosa.
It is worth noting that B12 and folate deficiency anemias are closely related. Folic acid (vitamin B9) also takes part in the formation of red blood cells. Even a full supply of these components in food does not guarantee the absence of anemia in cases where there is an increased consumption or there is a violation of utilization in the bone marrow. This may be due to parasitosis, intestinal dysbiosis, pregnancy, liver and blood diseases.
Diagnosis of anemia
Laboratory diagnostic methods: determination of Hb, Ht, reticulocytes, erythrocyte volume and examination of a peripheral blood smear.
Anemia is indicated by a decrease in such indicators as: Hb in men less than 130 g/l and in women less than 120 g/l; decrease or increase in reticulocytes, Ht less than 35% in women and less than 42% in men, etc.
Anemia varies according to:
- Degree of severity (mild, moderate, severe)
- Red blood cell size (microcytic, normocytic, macrocytic)
- According to the hemoglobin content in erythrocytes (hypo-, normo-, hyperchromic)
- Regenerative capacity of bone marrow (hypo-, hyper-, normoregenerative).
Symptoms of anemia
Symptoms of B12 deficiency anemia
At the initial stage of development, symptoms may be erased or not bother you at all. As the syndrome develops, the following signs may appear:
- weight loss not associated with objective reasons;
- burning of the tongue and changes in taste sensations;
- increase in the size of the tongue, smoothing of the papillae, redness of the mucous membranes;
- alternating constipation and diarrhea;
- nausea;
- tingling in the arms and legs, numbness;
- gait disturbance;
- urinary disorders;
- decreased sex drive;
- decreased muscle tone;
- visual impairment;
- pallor, yellowness of the skin;
- graying of hair;
- cardiopalmus;
- dyspnea;
- vitiligo (spots on the skin), etc.
It is worth noting that disorders in the psychoemotional and cognitive spheres are not uncommon: deterioration of memory, attention and thinking, mood swings, tearfulness, irritability, depressive tendencies. An older person may develop dementia. The severity of neuropsychiatric symptoms does not depend on the severity of anemia, but is determined by how long it lasts and how quickly a person receives medical help.
Symptoms of vitamin B12 deficiency
It is easier to prevent anemia than to treat and restore the body from the damage caused. Symptoms of cobalamin deficiency are easy to detect in yourself or loved ones:
- Against the background of a decrease in hemoglobin and an increase in bilirubin, the skin turns pale and yellowish.
- The heartbeat quickens, stabbing pain in the chest area due to overload is possible.
- Dizziness due to insufficient oxygen supply to the brain.
- Memory impairment, decreased mental abilities.
- Shortness of breath after minor physical exertion.
- Decreased visual acuity, blurred objects, “goosebumps” before the eyes.
- Digestive system disorders: heartburn, increased gas formation, diarrhea, distortion of taste.
- Stomatitis, it says, the tongue is raspberry colored.
- Nervous system disorders: muscle weakness, numbness or tingling of the extremities, impaired coordination of movements, insomnia, convulsions.
It is important to understand that long-term B12 deficiency leads to irreversible neurological changes. Timely identification and elimination of the deficiency normalizes the condition in 1.5-2 months.
Diagnostic features
Treatment of B12-deficiency anemia is prescribed after a comprehensive examination. The doctor will order the following laboratory hematological and other tests:
- general blood analysis;
- biochemical and immunological studies: determination of the level of B12 in plasma, assessment of the level of homocysteine in serum or blood plasma, determination of antibodies to gastric parietal cells, etc.;
- bone marrow aspiration or trephine biopsy.
Gastroscopy may also be required to detect atrophic gastritis.
The diagnosis is made by a doctor based on complaints, manifestations of the disease, and laboratory test parameters. It is important to find out the cause of the syndrome, especially to detect Addison-Biermer disease.
In addition, a specialist needs to distinguish this type of anemia from other diseases accompanied by disturbances in hematopoietic processes. Thus, if liver cirrhosis is suspected, disorders associated with long-term use of certain drugs (sulfonamides, anticonvulsants), sideroblastic anemia will require differential diagnosis.
Publications in the media
Anemia of this group develops due to vitamin B12 deficiency (daily requirement 1–5 mcg). Pernicious anemia is an autoimmune disease with the formation of antibodies to gastric parietal cells or intrinsic Castle factor. In most cases it is combined with fundic gastritis and achlorhydria. There are also B12-deficiency anemias of nutritional origin. Pernicious anemia can be congenital or acquired. The predominant age is over 60 years.
Etiology • Pernicious anemia •• Fundal gastritis (type A) ••• AT to gastric parietal cells ••• Immune disorders (production of AT to intrinsic Castle factor) • Other B12-deficiency anemia •• Vegetarian diet without additional vitamin B12 intake •• Gastrectomy •• Afferent loop syndrome •• Broad tapeworm infestation •• Malabsorption syndrome •• Chronic pancreatitis •• Chronic alcoholism •• Drugs (biguanides, phenylbutazone, aminosalicylic acid, oral contraceptives).
Genetic aspects. There are a number of genetically heterogeneous forms of pernicious anemia • Classic adult pernicious anemia (170900, presumably Â) with impaired absorption of vitamin B12 • Pernicious anemia in adolescents with polyglandular autoimmune syndrome (*240300, 21q22.3, r) • Juvenile pernicious anemia with relative malabsorption vitamin B12 and proteinuria (*261100, Immurslund–Grasbeck syndrome, 10p12.1, MGA1, r). With this megaloblastic anemia, malformations of the urinary tract and proteinuria are possible • Congenital pernicious anemia (*261000, chronicle 11, GIF, r gene mutation) due to the lack of gastromucoprotein secretion with normal gastric acidity and mucosal morphology. Expression of HLA-DR2, HLA-DR4 is characteristic.
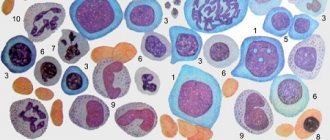
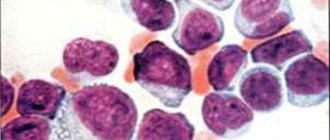
Pathomorphology • Bone marrow - megaloblastic type of hematopoiesis, increased iron content, hypersegmented neutrophils • Stomach - fundal gastritis, goblet cell hypertrophy, parietal cell atrophy, chief cell atrophy, characterized by cellular atypism • Spinal cord - myelin degeneration of the posterior and lateral columns, degenerative changes in the ganglia dorsal roots (funicular myelosis) • Degeneration of peripheral nerves.
The clinical picture is determined by vitamin B12 deficiency • General signs of anemia (weakness, shortness of breath, tachycardia, pallor, tinnitus, etc.) • Funicular myelosis (paresthesia, decreased vibration sensitivity, muscle atrophy, polyneuritis, pathological reflexes) • Impaired coordination (positive test Romberg and finger-nose test) • Mental disorders (confusion, depression, dementia) • From the gastrointestinal tract - atrophic glossitis (raspberry “varnished” tongue), hepatosplenomegaly, anorexia • Skin - hyperpigmentation, purpura, vitiligo.
Age characteristics • Juvenile pernicious anemia often occurs in adolescents and is generally similar to anemia in adults • Congenital pernicious anemia usually appears before age 3 • In the elderly, pernicious anemia occurs most often in combination with other autoimmune disorders, depression and dementia.
Concomitant pathology • Autoimmune diseases (rheumatoid arthritis, Graves' disease, hypothyroidism, hypoparathyroidism, Hashimoto's thyroiditis, diabetes) • Idiopathic adrenal insufficiency • IDA • Agammaglobulinemia • Tropical sprue • Crohn's disease • Infiltrative diseases of the ileum and small intestine.
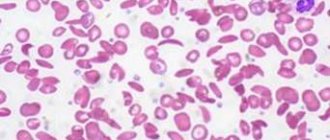
Laboratory tests • Pancytopenia (anemia, leukopenia, thrombocytopenia) • Peripheral blood smear: macrocytosis (mean erythrocyte volume >115 µm3), elliptocytosis, anisocytosis, poikilocytosis; Howell-Jolly bodies (spherical or ovoid eccentrically located granules; found in circulating red blood cells, more often and in greater numbers after splenectomy) and Cabot rings, hypersegmented neutrophils, reticulocyte count normal or slightly reduced • Plasma vitamin B12 concentration <100 pg/ml (normally 160–950 pg/ml) • Increased serum ferritin concentration • Achlorhydria • Hypergastrinemia • When stimulated by pentagastrin, gastric juice pH >6 • AT to intrinsic factor of Castle • AT to parietal cells • Hyperbilirubinemia due to direct fraction • Decreased content haptoglobin • Increased LDH activity.
Conditions affecting the results of studies • A false increase in the average erythrocyte volume is caused by the following factors: •• cold agglutinins •• hyperglycemia •• severe leukocytosis • A false normal level of vitamin B12 in the blood plasma is caused by the following conditions: •• myeloproliferative diseases •• liver diseases • False a decrease in the level of B12 in the blood plasma is detected in the presence of the following factors: •• multiple myeloma •• taking oral contraceptives •• pregnancy •• folic acid deficiency •• transcobalamin II deficiency. Special tests • Schilling test - decreased absorption of vitamin B12 • Bone marrow puncture.
TREATMENT
Management tactics • For pernicious anemia, treatment must be carried out for life • Outpatient regimen • Monthly administration of cyanocobalamin • Endoscopic examination every 5 years to exclude stomach cancer or as indicated • Diet with a high protein content.
Drug therapy. Cyanocobalamin - 100 mcg subcutaneously daily for 1 week, then 1 time per week for 1 month and then 1 time per month for life.
A complication of treatment is hypokalemia (may appear in the 1st week of treatment).
The course and prognosis are favorable with timely and adequate treatment with the vitamin cyanocobalamin. Signs of central nervous system damage may persist if the patient’s treatment was started 6 months or more from the onset of the disease.
Synonyms • Pernicious anemia • Addison–Biermer disease • Biermer disease
ICD-10 • D51 Vitamin B12 deficiency anemia
Features of treatment
Treatment of B12 deficiency anemia is based on replenishing the deficiency with vitamin B12 preparations. In almost all cases, this allows you to get a positive effect. Sometimes parenteral administration is advisable. Intramuscular injections are given daily or every other day, dosage is up to 500 mcg, depending on the severity of the condition. In the presence of a precomatous state, a dose of up to 1000 mcg may be required.
The dosage is reduced as the number of red blood cells and hemoglobin levels increase. Therefore, it is important to perform intermediate monitoring; the doctor will tell you how often you will need to take a blood test during therapy. Typically, the course of treatment takes at least 21–28 days.
If there are symptoms of funicular myelosis (paresthesia - numbness of the limbs), vitamin B12 is administered in large dosages daily for at least 10 days. Then the dose is reduced, and the course of therapy is supplemented with vitamin B1 at 100 mcg per day.
The criterion for the effectiveness of treatment is: an increase in the number of reticulocytes on the fifth – seventh day from the start of the course of therapy. As soon as remission is achieved, the patient is transferred to maintenance therapy. It consists of using the B12 drug at a dosage of 100–200 mcg 2–3 times a month, taking into account the daily requirement.
It is worth noting that patients with severe neurological symptoms can be transferred to lifelong maintenance therapy: 1 mg monthly.
It is important to understand that the form of the drug does not matter - drugs in tablets and injection solution are absorbed equally well. But the second method is preferable in cases where there are diseases of the gastrointestinal tract or impaired absorption of vitamins in the intestines.
Folic acid is used intramuscularly or orally, the standard dose is 50–60 mg. It is usually combined with B12. However, it is important to know that the use of folic acid causes an increased consumption of B12, sometimes leading to increased paresthesia in the limbs. The doctor will develop a treatment regimen for B12-deficiency anemia, taking this fact into account individually, especially for pregnant patients.
If there is a significant decrease in hemoglobin levels, blood transfusions may be indicated. Pre-comatose, comatose state, and cardiac symptoms are also grounds for serious intervention. It is preferable to choose red blood cell transfusion in a course of up to 6 transfusions.
Prognosis and prevention
Timely treatment of B12-deficiency anemia in most cases can completely eliminate the hematological disorder. Already on days 4-5, changes in test results can be detected; an increase in hemoglobin and the number of red blood cells is observed on the 7th day. These indicators are completely normalized after 8 weeks.
Neurological symptoms can go away for quite a long time, up to six months. Spinal cord damage associated with anemia is irreversible, so it is very important to promptly consult a doctor: a hematologist or therapist.
Increased attention to the prevention of this disease should be paid to patients who have undergone bariatric surgery or gastrectomy. At risk are vegetarians, people on strict diets with limited meat and offal, pregnant women and women who have recently given birth. Prevention consists of using the B12 drug in the form of tablets or injections; the doctor will select a safe prophylactic dose.