The symptom complex of vegetative-vascular dystonia includes many manifestations that affect the functioning of almost all organs. Extrasystole with VSD is a very common symptom and accompanies almost every VSD patient. It is exclusively neurological in nature and in most cases does not threaten the patient’s life, but it brings a lot of inconvenience and leads to an exacerbation of the disease.
What is characteristic of vegetative-vascular dystonia
It is important for a VSD patient to understand that his arrhythmia is of a functional nature. And no matter where exactly and in what quantity it occurs, one thing is clear: the heart is healthy, and the reason lies in something completely different.
Extrasystole in such patients manifests itself when a large amount of adrenaline enters the blood. But as soon as it decreases to normal, all sensations subside. That is, the problem is temporary and reversible. But patients tolerate it very hard. For them, this is like death: heart failures catch them suddenly, they can be repeated for several months and even years, until the cause is eliminated.
At this moment, a person is seized by a feeling of fear. He begins to choke, his legs give way, and he may lose consciousness. The patient becomes pale, begins to rush about, and scream. The sensation in the chest resembles a blow to the rib cage.
An even greater fear is the compensatory break after an extraordinary compression. The patient fears that his heart will stop. It seems to him that he will die, and this cannot be avoided.
If the excitement intensifies, then the symptoms worsen. Atrial fibrillation occurs. It seems that the heart works outside the regime, chaotically, as it pleases. Fortunately, this condition rarely occurs.
Diagnosis of cardioneurosis
Cardioneurosis does not cause organic pathological changes in the heart muscle and its arteries. To exclude various diseases, the patient must use diagnostic capabilities.
The diagnostic criteria for cardioneurosis are:
- continuous or recurring symptoms for at least three months;
- a clear connection between the appearance or intensification of symptoms with anxiety, periods of hormonal changes (pregnancy, adolescence, pre- and menopause);
- the presence of signs of dysfunction of the autonomic nervous system: sweating of the hands and feet, marbled skin tone, chilliness and coldness of the extremities, persistent white dermographism (a stripe that appears when a hard object is passed over the skin), a tendency to tachycardia and extrasystole, unstable blood pressure.
A depressed state, the inability to deal with problems is a typical onset of cardioneurosis in adolescents
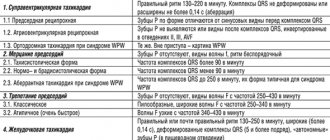
To exclude myocardial ischemia, ECG studies are performed. Cardioneurosis is not characterized by a decrease in the ST interval, changes in the T wave and ventricular complex.
In blood tests there is no increase in the concentration of enzymes indicating myocardial necrosis, leukocytes do not react.
Why do extrasystoles occur during VSD?
Cardiac “dancing” in vegetative-vascular dystonia can occur when both parts of the autonomic nervous system are disrupted.
If the sympathetic department fails, extrasystoles appear after physical exertion. They are poorly controlled by sedatives, and may even intensify after taking them.
If the functioning of the parasympathetic system is disrupted, in addition to cardiac symptoms, digestive disorders are of concern: epigastric pain, diarrhea, bloating. A cup of coffee or sweet tea or a brisk walk will help relieve such an attack.
If the cause is psychological, treatment measures are directed in the other direction.
Most often, dystonics are bothered by two types of extrasystole:
- Ventricular. Usually makes itself felt in the first half of the day. It is caused by disturbances in mental balance, for example, great joy or grief. It also appears when the weather changes or when drinking strong drinks. Other provoking factors include magnesium and calcium deficiency, osteochondrosis. It all starts with an intense beat in the heart area, followed by a pause. The patient becomes covered in cold, sticky sweat and develops a feeling of fear. Despair sets in, he cannot choose a comfortable position for himself, becomes numb or begins to fuss. The violence of his heart leads him into an uncontrollable state, causing him a lot of suffering.
- Supraventricular. The most common type of arrhythmia in VSD. The causes of this condition coincide with those of the ventricular form. In addition, dystonics who are addicted to antiarrhythmic and diuretic drugs are at risk. Patients claim that the condition worsens when lying down. It is this sign that indicates that the cardiac failure is functional in nature.
Who can develop cardioneurosis?
Psychologists have identified the character traits of a person with possible neurotic disorders. These include:
- tendency to anxiety and suspiciousness;
- excessive self-control;
- panic attacks in the event of a tense situation;
- frequent mood changes;
- causeless fatigue.
People with various phobias (fear, for example, of heights, darkness, enclosed spaces) are susceptible to cardioneurosis
Extrasystole and other signs of VSD
Considering that extrasystoles cause severe discomfort to dystonics and knock them out of their normal state, they become the cause of the development of other symptoms of VSD. These include:
- increased sweating;
- irritation;
- worry and anxiety;
- weakness and malaise;
- chills and feeling of heat.
Panic attacks that occur during heart dances become the basis for the formation of cardioneurosis. A dystonic person risks developing a phobia against the background of such interruptions in the heart.
Attacks of arrhythmia that occur at night disturb the sleep of the sufferer and provoke insomnia. It can also accompany him as a result of constant worry and anxiety.
Extrasystoles in neurocirculatory dystonia, despite their harmlessness, cause circulatory disorders, including cerebral circulation. As a result, the patient experiences attacks of suffocation, lack of air, and dizziness. Shortness of breath appears.
One of the complications provoked by extraordinary heart contractions during VSD is a panic attack. It begins with an attack of panic and fear, accompanied by a feeling of anxiety and tension. Other symptoms include tachycardia, internal trembling and sweating, nausea, suffocation and dizziness. Characterized by unpleasant sensations in the heart area, tingling and numbness of the arms and legs. The panicker is overcome by fear of death, consciousness is confused, and thinking is impaired.
Thus, arrhythmia, being a sign of VSD, provokes the development of other symptoms of the disease and aggravates its course.
Origin of violations
The causes of cardioneurosis are considered to be many factors that can provoke too strong and complex irritation.
An excessive process of inhibition or excitation in cortical structures contributes to the formation of pathology
There is an opinion that such a pathology develops in individuals with congenital inferiority of brain cells and too strong a connection between the cerebral cortex and the heart.
The impetus for the development of cardiac neurosis can be given by:
- both physical and mental trauma;
- violent conflict situations (family quarrels);
- unsatisfied desires (sexual disorders);
- very stressful work, study (anxiety during exams, lack of sleep);
- poor nutrition (with various diets, physical overload);
- chronic intoxication (alcohol, nicotine, drugs, industrial toxic substances).
Endocrine disorders play a significant role in cardioneurosis, especially in women (during menopause, thyrotoxicosis, ovarian hormone deficiency). In these cases, there is a mismatch in the work between the pituitary gland and the peripheral glands. A similar mechanism is “triggered” in adolescents during pregnancy.
What medications can be used to treat cardioneurosis?
As a medicinal intervention, a patient with cardioneurosis is offered drugs from the groups of neuroleptics, tranquilizers, and antidepressants.
Of the well-known traditional drugs used in cardiology, you can use drugs that have a slight psychotropic effect (β-blockers Verapamil, Nifedipine).
The hypersthenic type of neurotic reaction requires increasing the threshold of excitability with the help of specific medications (Trioxazine, Amizil, Meprotan).
For the hyposthenic type, stimulants and restoratives are prescribed (Securinin, vitamins, tincture of Eleutherococcus).
In premenopausal age with cardioneurosis, Mildronate, Magne B6, Preductal are especially indicated. The duration of the course and dose are determined by the doctor individually.
Modern therapy emphasizes the use of nootropics, which were previously used to improve the brain's memory function. Phenibut and Pantogam are considered effective for cardioneurotic disorders.
Pantogam active is considered an improved formula of a modern nootropic
How to help with a panic attack of cardialgia?
It is impossible to make a correct diagnosis of cardioneurosis at the level of the first person you meet and even an ambulance. If your loved ones are already familiar with the disease, you should:
- provide access to air - open a window, turn on the air conditioner, loosen the collar or belt clasp;
- place the patient in a quiet place;
- try to make it clear by your behavior that the fear is unfounded;
- If possible, measure pulse and blood pressure;
- distract the patient from his worries;
- You can massage the limbs, collar area (it is not advisable to use cold or hot compresses);
- Novo-passit solution, tablets or tincture of Valerian, Motherwort, Corvalol, Persen, Valocordin are recommended as home sedatives for cardioneurosis. You can take the drops again after 4 hours.
If the symptoms do not disappear, weakness increases, you should call an ambulance.
Despite the difficulties in diagnosis and selection of therapy, the patient needs to be patient and undergo a full examination. You should not treat cardioneurosis on your own. Changing your regimen and playing sports should be equated to medication. Without them, it is impossible to get rid of cardioneurosis. For women suffering from menopausal symptoms, the gynecologist will offer a special course of therapy. You cannot trigger neurosis and complicate your life.
Methods for treating cardioneurosis
Adequate treatment of cardioneurosis requires the involvement of a psychiatrist or psychoneurologist. A big mistake of patients and doctors is refusing the help of specialists. After all, conventional drugs used in cardiology do not work in this case. And the inability to relieve an attack with Nitroglycerin is known as a diagnostic sign of cardioneurosis.
Experts recommend starting to treat cardioneurosis with psychotherapy. It provides:
- reduction of general anxiety;
- distracting the patient from unnecessary negative thoughts and emotions;
- helps to set the intention for healing.
Psychotherapists will recommend classes in a group or individually, and the possibility of using auto-training. Currently, psychological attitudes that can be used on the Internet are important.
It is believed that in a group of like-minded people it is easier for a person to talk about his illness
Patients should change their routine, walk more often, and do what they love and enjoy.
You should exclude spicy and fatty foods, smoked foods, alcohol, preservatives from your diet, do not abuse sweets, and do not overeat. You need to quit smoking, and when working with occupational hazards, reconsider your capabilities and move on to safer work. After morning exercises, a contrast shower is necessary.
Physical therapy, physiotherapeutic procedures, and herbal treatment have a good effect.
Herbal mixtures to improve the functioning of the nervous system in case of cardioneurosis include:
- mint,
- Melissa,
- valerian root,
- hop cones,
- hawthorn fruits,
- chamomile flowers,
- motherwort leaves.
You can prepare the decoction yourself in a thermos.
How COVID-19 affects the heart
Initially, scientists assumed that COVID-19 affects exclusively lung tissue, and the numerous accompanying complications associated with the work of the heart are only a consequence of hypoxia (oxygen starvation) and a pronounced inflammatory process.
However, as the mechanisms of influence of SARS-CoV-2 on the body were studied, it was proven that the virus penetrates cells and attaches to the ACE2 protein. This protein is found in the endothelium (the cells lining blood vessels), as well as in the lungs, heart and other organs. The virus, penetrating these cells, partially destroys them and causes damage to cardiac tissue, reducing blood supply to the heart, which increases the risk of inflammation.
Thus, one of the most dangerous complications of the heart after coronavirus is myocarditis . The inflammatory process affecting the muscle tissue of the heart may not make itself felt for a long time, but as a result it becomes the cause of serious problems. The severity of clinical manifestations depends on the degree of damage to the heart muscle. The cause of inflammation of the heart muscle can also be an increase in temperature and intoxication of the body.
The greatest danger is inflammation of the myocardium, which has gone unnoticed by doctors. Untreated myocarditis leads to serious complications:
- arrhythmia - a violation of the conductivity of electrical impulses, which are manifested by tachycardia, extrasystole, atrial fibrillation;
- cardiomyopathy - heart failure, which is accompanied by a change in the volume of the ventricles, enlargement of the atria, a violation of the ejection of blood from the heart into the vascular bed;
- intracardiac thrombus ;
- sudden death.
Inflammatory changes in the myocardium disrupt the electrical stability of the heart. This leads to tachyarrhythmia, which intensifies with physical activity. Therefore, patients who previously had no heart problems often complain of poor exercise tolerance after coronavirus.
Cardiac myocarditis, as a complication after coronavirus, occurs in patients of all age groups, but due to the fact that the onset of the disease is often asymptomatic or with minimal symptoms, patients are not examined and do not seek help on time.
That is why, after recovery from COVID-19, it is necessary to undergo a complete diagnosis of the functioning of the cardiovascular system and, if necessary, select an individual program to restore the functioning of the heart and blood vessels.
Euromed Clinic offers patients to undergo a rehabilitation program, which is developed individually taking into account the severity of the COVID-19 disease, the presence of concomitant diseases and a number of other factors.