Cobalamin deficiency leads to a lack of red blood cells and hemoglobin in the blood, which causes anemia. Acute deficiency occurs in 0.1% of the population; elderly people over 70 years of age are most susceptible to it, among whom low values are detected in every tenth, and B12 deficiency anemia is diagnosed in every hundredth. If therapy is not started in time, pancytopenia is possible - the body will begin to experience a deficiency of various blood elements. Diagnosis and treatment of all types of anemia in Anapa is carried out in a medical clinic.
Symptoms of vitamin B12 deficiency
It is easier to prevent anemia than to treat and restore the body from the damage caused. Symptoms of cobalamin deficiency are easy to detect in yourself or loved ones:
- Against the background of a decrease in hemoglobin and an increase in bilirubin, the skin turns pale and yellowish.
- The heartbeat quickens, stabbing pain in the chest area due to overload is possible.
- Dizziness due to insufficient oxygen supply to the brain.
- Memory impairment, decreased mental abilities.
- Shortness of breath after minor physical exertion.
- Decreased visual acuity, blurred objects, “goosebumps” before the eyes.
- Digestive system disorders: heartburn, increased gas formation, diarrhea, distortion of taste.
- Stomatitis, it says, the tongue is raspberry colored.
- Nervous system disorders: muscle weakness, numbness or tingling of the extremities, impaired coordination of movements, insomnia, convulsions.
It is important to understand that long-term B12 deficiency leads to irreversible neurological changes. Timely identification and elimination of the deficiency normalizes the condition in 1.5-2 months.
Reasons for a critical decrease in cobalamin
B12 deficiency anemia occurs when there is insufficient intake of animal protein into the body and in cases where cobalamin is not absorbed and does not enter the blood.
In the first case, people most often suffer who limit themselves in nutrition - losing weight, vegetarians, adherents of methods with an unbalanced diet. B12 is found in meat, beef liver, dairy products, and egg yolks.
The second, endogenous cause requires diagnosis. The absorption of cobalamin is ensured by the enzyme Castle factor. When the synthesis of intrinsic factor Castle decreases or stops, the vitamin that enters the body is not absorbed.
Absorption into the bloodstream is prevented by diseases of the gastrointestinal tract:
- atrophic gastritis,
- chronic pancreatitis,
- Crohn's disease,
- diverticula of the small intestine,
- tumors.
In some hormonal diseases, including hyperthyroidism, B12 consumption increases several times. At the same time, the body experiences a shortage of it even with normal intake and without problems of absorption.
In some cases, the cause of deficiency is helminths and bacteria, taking certain medications and oral contraceptives, and alcoholism. Even frequent intestinal upset can interfere with the absorption of the substance.
Pernicious anemia (B12 deficiency, folate deficiency, megaloblastic)
Terminology
The long, but not complete list of synonymous diagnoses that served as the title of the article requires comment;
Along the way, the content of these terms will also become clearer. What our blood is made of, what its biological role is, what anemia is - the materials “Clinical Blood Test” and “Anemia. Blood and bloodlessness." More information about B vitamins can be found in the articles “Vitamin B. Hypovitaminosis” and “Vitamin B. Hypervitaminosis”.
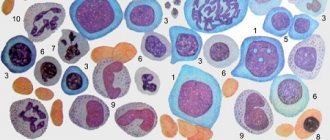
Pernicious in translation from Latin into Russian means “dangerous”, and in medical translation it means “severe, malignant, prognostically unfavorable”. Megaloblastic (sometimes written “megaloblastic”) means that the bone marrow contains a large number of large cells that are “under-erythrocytes” - one of the intermediate, immature forms of red blood cells.
B12 is a vitamin (it is clear which group), otherwise called the Castle factor and is represented by four different cobalt-containing substances with the same biological properties, which made it possible to distinguish them into a single subgroup of vitamin B.
Folic (literally “leafy”) acid is a vitamin of the same group, namely B9.
Thus, we get: dangerous, malignant B-vitamin deficiency immature erythrocyte anemia. Previously, it was called that: pernicious anemia or pernicious anemia. But it is also called Addison-Biermer's disease or Biermer's anemia, and here's why.
In 1822, the symptoms of a certain serious blood disease were first mentioned by the English physician J.S. Combe. In 1849 , his compatriot, the outstanding physician and scientist Thomas Addison, gave a more detailed description and interpretation. Much later, in 1871 , but independently of Addison, the German researcher Michael Anton Birmer studied and characterized this disease in detail, which he gave the name progressive pernicious anemia.
Later, the American William Murphy intensively sought treatment for anemia (for anemia in general, without nosological division), conducting experiments on artificially bled dogs. Murphy fed them different foods and compared recovery rates; His attention was drawn to the raw liver. Since the 1920s, through the efforts of W. Murphy, J. Whipple and J. Minot, pernicious anemia ceased to be an unambiguously and completely lethal disease: the life-saving medicine lay precisely in the liver. And it all ended with Murphy, Whipple and Minot in 1934 for isolating a substance (a group of compounds, as it turned out) known today as vitamin B12.
In parallel with these works, the American scientist William Bosworth Castle studied anemia, about whom the memorial publication of the US National Academy of Sciences (2018) says: “From a purely descriptive art, he transformed hematology into a dynamic interdisciplinary science.” Among other things, W.B. Castle once subjected himself and a group of volunteer patients to a not very appetizing experiment (involving the ingestion and regurgitation, after an hour, of raw meat, which was then used as a treatment for severe anemia). This strange experiment, however, was a brilliant idea: Castle proved beyond doubt that in order to turn raw meat into real medicine, it must be in the stomach - where a certain processing, activating reagent is contained. This gastric enzyme, gastromucoprotein, is today known throughout the world as “intrinsic Castle factor,” while “extrinsic Castle factor” refers to vitamin B12 itself.
In a series of articles about vitamins, the Lakhta Clinic has repeatedly drawn attention to the fact that the history of the discovery and study of these amazing substances turned out to be very difficult, tortuous, and sometimes dramatic. But humanity in general and medicine in particular are distinguished by incredible self-preservation stubbornness when something truly threatens us. Today, cardiovascular pathology, malignant tumors, viral hepatitis, autoimmune and hereditary diseases are on the agenda. And figuratively speaking, these killers will not hide from us anywhere, just as the plague and leprosy, vitamin deficiencies and anemia did not hide: the true causes will be exposed, the pathogenesis will be thoroughly studied, and cures will be found. Hurry up, gentlemen, scientists. Hurry up. We know that everything imaginable and inconceivable is being done; We know that somewhere in laboratories, clinics, university centers, modern Castles, Addisons, Birmers, Jenners, Mechnikovs, Flemmings are wrinkling their high foreheads and rubbing their eyes, sore from insomnia. Still, hurry up, please...
Returning to the confusing problem of B12-deficiency anemia: pernicious anemia is not a synonym, it is a special case. As is already clear from what has been said, the lack of cobalt-containing vitamins and folic acid in the body can be due to two fundamentally different reasons.
Diagnosis of pernicious anemia
To determine vitamin B12 levels, a biochemical blood test is performed. If the levels are below normal, a lack of cobalamin is noted or a deficiency is diagnosed.
The most important thing in diagnosis is to identify the cause of B12 deficiency anemia. To do this, a number of diagnostic studies are carried out:
- stool analysis for worm eggs;
- Schilling's test - a test of the body's ability to absorb B12 from the intestines;
- gastroscopy – endoscopic examination of the stomach, detection of gastritis, cancer and other diseases;
- colonoscopy – examination of the intestines, detection of tumors;
- X-ray of the stomach;
- Ultrasound of the abdominal organs;
- electroencephalography and MRI of the brain.
The doctor will prescribe those examinations that he considers necessary, taking into account age and concomitant diseases (or if they are suspected).
Primary diagnosis of anemia
A comprehensive study taking into account the quantitative and qualitative composition of cells, as well as biochemical blood parameters, which allows us to identify signs of iron deficiency anemia.
The research results are provided with a free doctor’s commentary.
English synonyms
Iron deficiency anemia screening.
Research method
Colorimetric photometric method, flow cytometry, SLS (sodium lauryl sulfate) method, conductometric method, immunoturbidimetry.
Units
μmol/l (micromoles per liter), *10^9/l (10 in st. 9/l), *10^12/l (10 in st. 12/l), g/l (grams per liter), % (percent), fl (femtoliter), pg (picogram).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- Eliminate alcohol from your diet 24 hours before the test.
- Do not eat for 12 hours before the test.
- Do not take medications for 24 hours before the test (as agreed with your doctor).
- Avoid physical and emotional stress 30 minutes before the test.
- Do not smoke for 30 minutes before the test.
General information about the study
Anemia is a pathological condition characterized by a decrease in the number of red blood cells and/or hemoglobin in the blood. The causes of anemia are varied and can be closely related to chronic somatic diseases (kidney and liver pathologies, autoimmune, infectious and inflammatory diseases, diabetes, tumors), acute and chronic blood loss, hereditary diseases and malnutrition, lack of vitamins and microelements. They occur when there is insufficient production of red blood cells in the bone marrow (for example, with deficiency of iron, vitamins B12 and B6, bone marrow depletion) or premature and excessive destruction of red blood cells in the bloodstream (for example, with hemolysis).
The most common form of anemia, iron deficiency, is detected in 80-90% of patients who have a reduced number of red blood cells and/or hemoglobin in the blood.
Iron deficiency develops gradually. Initially, a negative iron balance is created, in which the body's needs for it and its losses exceed the amount it receives from food. This may be due to blood loss, pregnancy, breastfeeding, growth spurts during puberty, malabsorption of micronutrients in the gastrointestinal tract, or insufficient intake of foods containing iron, as with vegetarianism.
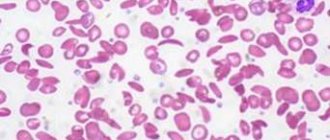
Normally, iron is absorbed in the small intestine, but in some chronic diseases of the stomach and intestines, malabsorption syndrome occurs with impaired absorption of nutrients and microelements from food. In the blood, iron is transported by the protein transferrin to sites of use or accumulation. With iron deficiency, the amount of free transferrin in the blood increases, and the level of serum iron decreases. Hemoglobin synthesis in the bone marrow occurs less actively, and iron deficiency anemia develops with clinical manifestations of anemia. In a general blood test, small pale colored red blood cells are detected, MHC (average hemoglobin content in an erythrocyte), MCV (average erythrocyte volume), MCHC (average hemoglobin concentration in an erythrocyte), and hemoglobin level and hematocrit decrease. Without treatment, the amount of hemoglobin decreases more and more, the shape of red blood cells changes, and the intensity of cell division in the bone marrow decreases. Due to a decrease in the amount of hemoglobin and red blood cells, the transport of oxygen and carbon dioxide in the tissues is disrupted, symptoms of anemia appear: pale skin, headache, memory impairment, drowsiness, spots before the eyes, dizziness, fainting, rapid heartbeat, decreased blood pressure, pain in the area heart, muscle weakness.
In addition to well-being, negative changes occur in appearance: dry skin (as a result, early wrinkles), brittle nails, hair loss.
Children susceptible to anemia are more likely than healthy peers to suffer from colds.
In addition, with iron deficiency, the patient may experience a disturbance of taste and smell: there is a desire to eat chalk, clay, raw cereals and inhale the smells of acetone, gasoline, and turpentine.
Often people do not pay attention to the main signs of anemia - constant fatigue, paleness, dry skin - considering them an insufficient reason to see a doctor. Of course, such symptoms do not always indicate a disease; it cannot be diagnosed only by their presence. Moreover, you should not start taking iron-containing medications on your own - this can lead to serious complications.
It is important to know what exactly causes anemia. For example, in older people it often results from internal bleeding due to a tumor in the gastrointestinal tract. There is a type of anemia associated with poor absorption of vitamin B12. But in order to identify it, you first need to make sure that there is enough iron in the body and that the red blood cells are saturated with it.
At the same time, simply donating blood for hemoglobin is not enough to fully diagnose anemia. For example, in smokers, the level of hemoglobin and red blood cells is often normal: carbon monoxide contained in cigarettes, combining with hemoglobin, forms the substance carboxyhemoglobin, this form of hemoglobin does not have the ability to carry oxygen, and to compensate for oxygen starvation, the level of hemoglobin increases. It turns out that a comprehensive analysis is needed, reflecting the true reserves of this microelement in the body: determination of the levels of serum iron, transferrin, reticulocytes, general blood test, leukocyte formula.
In addition, it is important that timely diagnosis of anemia makes it possible to identify diseases of which it is the first symptom: some malignant tumors, chronic inflammatory processes, helminthic infestations, etc.
What is the research used for?
- For the diagnosis of iron deficiency anemia.
- For differential diagnosis of anemia.
- For the evaluation of patients at high risk of developing anemia.
- To evaluate the effectiveness of treatment for iron deficiency anemia.
When is the study scheduled?
- For symptoms of iron deficiency in the body (pallor and/or yellowness of the skin, general weakness, fatigue, drowsiness, dizziness, tinnitus, flashing spots before the eyes, fainting, atrophy of the tongue mucosa, changes in the structure of the nails, abnormal taste preferences).
- When the number of red blood cells and/or hemoglobin decreases according to a clinical blood test.
- In the presence of risk factors for the development of anemia (pregnancy, breastfeeding, menstrual irregularities, malnutrition, vegetarianism, diseases of the stomach and intestines with impaired absorption of nutrients, chronic stress).
- When examining children during periods of intensive growth.
- When examining patients with asthenia of unknown origin and severe fatigue.
- When monitoring the effectiveness of the use of drugs containing iron.
What do the results mean?
Reference values
- Serum iron
| Floor | Age | Reference values |
| Female | Less than 24 days | 17.9 - 44.8 µmol/l |
| 24 days – 1 year | 7.2 - 17.9 µmol/l | |
| 1-14 years | 9 - 21.5 µmol/l | |
| More than 14 years | 10.7 - 32.2 µmol/l | |
| Male | Less than 24 days | 17.9 - 44.8 µmol/l |
| 24 days – 1 year | 7.2 - 17.9 µmol/l | |
| 1-14 years | 9 - 21.5 µmol/l | |
| More than 14 years | 12.5 - 32.2 µmol/l |
- Leukocyte formula
- Leukocytes
| Age | Reference values |
| Less than 1 year | 6 - 17.5 *10^9/l |
| 1-2 years | 6 - 17 *10^9/l |
| 2-4 years | 5.5 - 15.5 *10^9/l |
| 4-6 years | 5 - 14.5 *10^9/l |
| 6-10 years | 4.5 - 13.5 *10^9/l |
| 10-16 years | 4.5 - 13 *10^9/l |
| More than 16 years | 4 - 10 *10^9/l |
- Neutrophils
| Age | Reference values |
| Less than 1 year | 1.5 - 8.5 *10^9/l |
| 1-2 years | 1.5 - 8.5 *10^9/l |
| 2-4 years | 1.5 - 8.5 *10^9/l |
| 4-6 years | 1.5 - 8 *10^9/l |
| 6-8 years | 1.5 - 8 *10^9/l |
| 8-10 years | 1.8 - 8 *10^9/l |
| 10-16 years | 1.8 - 8 *10^9/l |
| More than 16 years | 1.8 - 7.7 *10^9/l |
- Neutrophils, %
| Age | Reference values |
| Less than 1 year | 16 — 45 % |
| 1-2 years | 28 — 48 % |
| 2-4 years | 32 — 55 % |
| 4-6 years | 32 — 58 % |
| 6-8 years | 38 — 60 % |
| 8-10 years | 41 — 60 % |
| 10-16 years | 43 — 60 % |
| More than 16 years | 47 — 72 % |
- Complete blood count (without leukocyte formula and ESR)
- Leukocytes
| Age | Reference values |
| Less than 1 year | 6 - 17.5 *10^9/l |
| 1-2 years | 6.6 - 11.2 *10^9/l |
| 2-4 years | 5.5 - 15.5 *10^9/l |
| 4-6 years | 5 - 14.5 *10^9/l |
| 6-10 years | 4.5 - 13.5 *10^9/l |
| 10-16 years | 4.5 - 13 *10^9/l |
| More than 16 years | 4 - 10 *10^9/l |
- Red blood cells
| Floor | Age | Reference values |
| Less than 1 year | 4.1 - 5.3 *10^12/l | |
| 1-5 years | 4 - 4.4 *10^12/l | |
| 5-6 years | 4.1 - 4.5 *10^12/l | |
| 6-7 years | 4 - 4.4 *10^12/l | |
| 7-8 years | 4.2 - 4.6 *10^12/l | |
| 8-9 years | 4.1 - 4.5 *10^12/l | |
| 9-14 years | 4.2 - 4.6 *10^12/l | |
| 14-15 years old | 4.4 - 4.8 *10^12/l | |
| Female | 15-19 years old | 3.5 - 5 *10^12/l |
| More than 19 years | 3.5 - 5.2 *10^12/l | |
| Male | 15-19 years old | 3.9 - 5.6 *10^12/l |
| More than 19 years | 4.2 - 5.3 *10^12/l |
- Hemoglobin
| Age | Reference values |
| Less than 2 weeks | 134 - 198 g/l |
| 2 weeks – 2 months | 124 - 166 g/l |
| 2-12 months | 110 - 131 g/l |
| 1-2 years | 110 - 132 g/l |
| 2-3 years | 111 – 133 g/l |
| 3-4 years | 112 – 134 g/l |
| 4-5 years | 114 - 134 g/l |
| 5-6 years | 113 - 135 g/l |
| 6-7 years | 115 - 135 g/l |
| 7-8 years | 116 - 138 g/l |
| 8-9 years | 115 - 137 g/l |
| 9-10 years | 118 - 138 g/l |
| 10-11 years | 114 - 140 g/l |
| 11-12 years old | 118 - 142 g/l |
| 12-13 years old | 117 - 143 g/l |
| 13-14 years old | 121 - 145 g/l |
| 14-15 years old | 120 – 144 g/l |
| 15-16 years old | 130 – 168 g/l |
| 16-17 years old | 130 – 168 g/l |
| 17-18 years old | 120 – 148 g/l |
| Over 18 years old | 120 – 156 g/l |
- Hematocrit
| Floor | Age | Reference values |
| Less than 1 year | 33 — 41 % | |
| 1-3 years | 32 — 40 % | |
| 3-6 years | 32 — 42 % | |
| 6-9 years | 33 — 41 % | |
| 9-12 years | 34 — 43 % | |
| Female | 12-15 years | 34 — 44 % |
| 15-18 years old | 34 — 44 % | |
| 18-45 years old | 35 — 45 % | |
| 45-65 years | 35 — 47 % | |
| More than 65 years | 35 — 47 % | |
| Male | 12-15 years | 35 — 45 % |
| 15-18 years old | 37 — 48 % | |
| 18-45 years old | 39 — 49 % | |
| 45-65 years | 39 — 50 % | |
| More than 65 years | 39 — 50 % |
- Mean erythrocyte volume (MCV)
| Floor | Age | Reference values |
| Less than 1 year | 71 – 112 fl | |
| 1-5 years | 73 – 85 fl | |
| 5-10 years | 75 – 87 fl | |
| 10-12 years | 76 – 94 fl | |
| Female | 12-15 years | 73 – 95 fl |
| 15-18 years old | 78 – 98 fl | |
| 18-45 years old | 81 – 100 fl | |
| 45-65 years | 81 – 101 fl | |
| More than 65 years | 81 – 102 fl | |
| Male | 12-15 years | 77 – 94 fl |
| 15-18 years old | 79 – 95 fl | |
| 18-45 years old | 80 – 99 fl | |
| 45-65 years | 81 – 101 fl | |
| More than 65 years | 81 – 102 fl |
- Average hemoglobin content in erythrocytes (MCH)
| Age | Reference values |
| Less than 1 year | 31 - 37 pg |
| 1-3 years | 24 - 33 pg |
| 3-12 years | 25 - 33 pg |
| 13-19 years old | 26 - 32 pg |
| More than 19 years | 27 - 31 pg |
- Mean erythrocyte hemoglobin concentration (MCHC)
| Age | Reference values |
| Less than 1 year | 290 – 370 g/l |
| 1-3 years | 280 – 380 g/l |
| 3-12 years | 280 – 360 g/l |
| 13-19 years old | 330 - 340 g/l |
| More than 19 years | 300 – 380 g/l |
- Platelets
| Floor | Age | Reference values |
| Less than 1 year | 214 - 362 *10^9/l | |
| 1-2 years | 208 - 352 *10^9/l | |
| 2-3 years | 209 - 351 *10^9/l | |
| 3-4 years | 196 - 344 *10^9/l | |
| 4-5 years | 208 - 332 *10^9/l | |
| 5-6 years | 220 - 360 *10^9/l | |
| 6-7 years | 205 - 355 *10^9/l | |
| 7-8 years | 205 - 375 *10^9/l | |
| 9-10 years | 177 - 343 *10^9/l | |
| 10-11 years | 211 - 349 *10^9/l | |
| 11-12 years old | 198 - 342 *10^9/l | |
| 12-13 years old | 202 - 338 *10^9/l | |
| 13-14 years old | 192 - 328 *10^9/l | |
| 14-15 years old | 198 - 342 *10^9/l | |
| 15-18 years old | 165 - 396 *10^9/l | |
| 18-45 years old | 159 - 376 *10^9/l | |
| Male | 45-65 years | 156 - 300 *10^9/l |
| Female | 45-65 years | 156 - 351 *10^9/l |
| More than 65 years | 139 - 363 *10^9/l |
- Mean platelet volume (MPV)
| Age | Reference values |
| Less than 10 years | 8.3 - 10.9 fl |
| 10 – 18 years | 8.6 - 12.1 fl |
| 18 – 45 years old | 8.5 - 12.8 fl |
| 45 – 65 years | 8.6 - 12 fl |
| 45 – 65 years | 9 - 12.9 fl |
| More than 65 years | 8.8 - 12.4 fl |
- Reticulocytes
- Reticulocytes, % (RET%)
| Floor | Age | Reference values |
| Female | Less than 2 weeks | 0,15 — 1,5 % |
| 2 weeks – 1 month | 0,45 — 1,4 % | |
| 1-2 months | 0,45 — 2,1 % | |
| 2-6 months | 0,25 — 0,9 % | |
| 6 months – 2 years | 0,2 — 1 % | |
| 2-6 years | 0,2 — 0,7 % | |
| 6-12 years | 0,2 — 1,3 % | |
| 12-18 years old | 0,12 — 2,05 % | |
| Over 18 years old | 0,59 — 2,07 % | |
| Male | Less than 2 weeks | 0,15 — 1,5 % |
| 2 weeks – 1 month | 0,45 — 1,4 % | |
| 1-2 months | 0,45 — 2,1 % | |
| 2-6 months | 0,25 — 0,9 % | |
| 6 months – 2 years | 0,2 — 1 % | |
| 2-6 years | 0,2 — 0,7 % | |
| 6-12 years | 0,2 — 1,3 % | |
| 12-18 years old | 0,24 — 1,7 % | |
| Over 18 years old | 0,67 — 1,92 % |
- Reticulocytes (absolute count, RET#)
| Floor | Reference values |
| Female | 17 - 63.8 *109/l |
| Male | 23 - 70 *109/l |
- Immature reticulocyte fraction (IRF)
| Floor | Reference values |
| Female | 3 — 15,9 % |
| Male | 2,3 — 13,4 % |
- Transferrin
| Age | Reference values |
| Less than 11 years old | 2.03 - 3 g/l |
| More than 11 years | 2 - 3.6 g/l |
Serum iron
Reasons for the increase:
- anemia (aplastic, hemolytic, pernicious), thalassemia;
- polycythemia;
- acute hepatitis, liver damage;
- hemochromatosis;
- hemosiderosis;
- nephritis;
- lead poisoning;
- excessive intake of iron supplements.
Reasons for the decline:
- chronic inflammation;
- Iron-deficiency anemia;
- blood loss;
- burns;
- malignant neoplasms;
- rheumatoid arthritis;
- myocardial infarction;
- nephrosis;
- malabsorption;
- pregnancy;
- uremia.
General blood analysis
1) Red blood cell count
Reasons for the increase:
- erythremia;
- chronic heart and pulmonary failure;
- stress, physical activity, staying at high altitudes;
- Itsenko-Cushing syndrome.
Reasons for the decline:
- anemia of various origins;
- acute and chronic leukemia;
- lymphomas;
- myelodysplastic syndrome;
- radiation sickness;
- renal failure;
- hypothyroidism;
- taking cytostatics.
2) Hemoglobin
Reasons for the increase:
- erythrocytosis;
- polycythemia;
- dehydration;
- burns;
- Cushing's syndrome;
- kidney cysts;
- liver cancer;
- heart failure;
- chronic lung diseases with respiratory failure.
Reasons for the decline:
- anemia of various origins;
- blood loss;
- myelodysplastic syndrome;
- Addison's disease;
- overhydration;
- acute and chronic leukemia, lymphoma;
- multiple myeloma;
- cirrhosis;
- chronic infection;
- hypothyroidism;
- kidney disease;
- pregnancy;
- autoimmune diseases;
- deficiency of vitamins B6, B12.
3) Mean erythrocyte volume (MCV)
Causes of increased (macrocytosis):
- megaloblastic anemia;
- myelodysplastic syndrome;
- liver diseases;
- pregnancy;
- hypothyroidism;
- alcoholism;
- treatment with estrogens, barbiturates.
Reasons for decrease (microcytosis):
- anemia (microspherocetary, iron deficiency, sideroblastic, thalassemia);
- anemia in chronic diseases;
- hypohydration;
- aluminum intoxication.
4) Dispersion of red blood cell distribution by volume (RDW)
Reasons for the increase (anisocytosis):
- anemia (hemolytic, iron deficiency, megaloblastic);
- osteomyelofibrosis.
5) Average hemoglobin content in erythrocytes (MCH)
Causes of increase (hyperchromia):
- megaloblastic anemia;
- cirrhosis of the liver;
- neonatal period.
Reasons for decrease (hypochromia):
- Iron-deficiency anemia;
- thalassemia;
- sideroblastic anemia.
6) Mean erythrocyte hemoglobin concentration (MCHC)
Reasons for the increase:
- megaloblastic anemia;
- microspherocytosis;
- prolonged hypohydration;
- neonatal period.
Reasons for the decrease (absolute hypochromia):
- Iron-deficiency anemia;
- thalassemia;
- sideroblastic anemia;
- hydremia.
7) Hematocrit usually decreases with anemia of various etiologies.
 The number of platelets can be increased in iron deficiency anemia and hemolytic crisis, decreased in aplastic or megaloblastic anemia.
The number of platelets can be increased in iron deficiency anemia and hemolytic crisis, decreased in aplastic or megaloblastic anemia.
9) The number of leukocytes decreases with megaloblastic or aplastic anemia, severe forms of iron deficiency anemia.
Reticulocytes
Reasons for increase (hyperregeneration):
- anemia (hemolytic, acute post-hemorrhagic);
- effective treatment of anemia caused by deficiency of iron, folic acid, vitamins B12 and B6 (on the 6-10th day);
- recovery from the state of bone marrow hypoplasia after cytostatic therapy;
- splenectomy;
- malaria.
Reasons for decrease (hyporegeneration):
- anemia (hypo- or aplastic, megaloblastic);
- anemia of chronic disease;
- myelodysplastic syndrome;
- acute leukemia;
- radiation sickness;
- regeneration crisis in hemolytic anemia;
- kidney pathology;
- taking cytostatics.
Transferrin
Reasons for the increase:
- Iron-deficiency anemia;
- pregnancy;
- taking estrogen.
Reasons for the decline:
- acute inflammation;
- anemia in chronic diseases;
- hypoproteinemia (with chronic infections, chronic kidney diseases, liver diseases, neoplasms, burns and malnutrition);
- genetic defects;
- hemochromatosis;
- oversaturation of the body with iron.
What can influence the result?
- Transfusion of blood and its components.
- Use of intravenous radiopaque agents shortly before the examination.
- Hemodialysis.
- Alcoholic liver disease, acute and chronic inflammatory diseases, neoplasms.
- Taking medications containing iron.
- The use of certain hormonal drugs, as well as other drugs that affect certain test indicators.
Important Notes
- Iron deficiency anemia is often a complication of other diseases, so it is important to find out the primary cause of iron loss. Diagnosis must be comprehensive, taking into account clinical data and the results of additional instrumental methods.
- Incorrect diagnosis of the type of anemia leads to inadequate treatment and progression of the disease. In difficult diagnostic cases, bone marrow puncture and myelogram are recommended. Only a doctor can evaluate the results of the study and select therapy.
Also recommended
- Laboratory diagnosis of iron deficiency anemia
- Laboratory diagnosis of anemia
- Bilirubin and its fractions (total, direct and indirect)
- Laboratory examination of the kidneys
- General urine analysis with sediment microscopy
- Fecal occult blood test
- Erythrocyte sedimentation rate (ESR)
- C-reactive protein, quantitative (highly sensitive method)
- Total protein in whey
- Serum albumin
- Ferritin
- Iron binding capacity of serum
- Latent iron binding capacity of serum
- Vitamin B9 (folic acid)
- Vitamin B12 (cyanocobalamin)
- Erythropoietin
Who orders the study?
Therapist, pediatrician, general practitioner, obstetrician-gynecologist, hematologist.
Literature
- Harrison's Principles of Internal Medicine. 16th ed. NY: McGraw-Hill; 2005: 2607 p.
- Fischbach FT, Dunning MB A Manual of Laboratory and Diagnostic Tests, 8th Ed. Lippincott Williams & Wilkins, 2008: 1344 p.
- Wilson D. McGraw-Hill Manual of Laboratory and Diagnostic Tests 1st Ed. Normal, Illinois, 2007: 666 p.
- Internal medicine: Textbook in 3 volumes. T1/Ed. prof. E. N. Amosova. – K.: Medicine, 2008 – P. 907-938.
Elimination of B12 deficiency and treatment of anemia
To compensate for vitamin B12 deficiency, intramuscular injections are prescribed. Treatment lasts at least six weeks. The dosage of the drug is determined based on test results. Be sure to monitor the effectiveness of treatment with blood tests 2-3 times a week.
The identified causes of anemia are eliminated if the diseases are amenable to drug or surgical treatment. If the deficiency is caused by nutritional reasons (poor nutrition), a diet with a high content of animal proteins is developed.
If the patient's chronic disease cannot be treated, maintenance therapy with injections is carried out on an ongoing basis to prevent the development of anemia. By controlling B12 levels, people live to a ripe old age. If life is threatened (severe anemia or anemic coma), blood transfusions are used.
Under no circumstances should you self-medicate or take B12 - an excess in the body can lead to thrombosis, disruption of the gastrointestinal tract, loss of vision, increased excitability, and heart failure.
For consultation, for examination with suspected B12 deficiency anemia, cobalamin deficiency, or for a preventive examination, contact a medical specialist in Anapa. You can make an appointment with specialists by phone.