Aortofemoral bypass surgery is a surgical procedure that involves installing a bypass - a shunt bypassing the blocked iliac arteries from the abdominal aorta to the femoral arteries in the groin area using an artificial vascular graft. It is the most common intervention on the vessels of the lower extremities for atherosclerosis.
The main indication for aortofemoral bypass is atherosclerosis of the aorta and iliac arteries (Leriche syndrome) with the development of severe circulatory failure of the extremities.
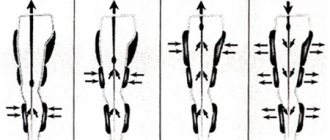
Unilateral aorto-femoral bypass involves performing a linear shunt from the aorta to one femoral artery, and with bifurcation aorto-femoral bypass - to two femoral arteries using a special Y-shaped shunt).
Aortofemoral prosthesis is used for blockage (occlusion) of the aorta and differs from bypass surgery in that the prosthesis is sewn end to end to the abdominal aorta, thereby all blood flow to the legs goes only through the prosthesis. During bypass surgery, the prosthesis is sewn into the side of the aorta and residual blood flow through the affected iliac vessels is maintained.
Aortofemoral bifurcation bypass surgery is highly effective and safe, but should be used with caution in elderly patients and with severe concomitant pathology. Surgeries on the abdominal aorta have a small risk to life (no more than 3%) and prevent the development of ischemic gangrene in patients with Leriche syndrome.
Features of the operation at the Innovative Vascular Center
Although aortobifemoral bypass surgery is one of the most common vascular operations and is performed in many vascular departments, our clinic uses certain approaches to improve the immediate and long-term results of the operation, especially in complex cases.
The main problem when performing ABBG remains the traumatic approach and associated early postoperative problems. In our clinic, a retroperitoneal approach is used to perform aortofemoral bypass surgery, without opening the abdominal cavity. This allows operations to be performed under epidural anesthesia without general anesthesia and ensures a comfortable postoperative period.
To perform repeated operations on the aorta in case of suppuration of vascular prostheses or thrombosis, our surgeons can use access to the thoracic aorta using an extended left-sided lateral approach. This approach made it possible to perform operations on patients who were refused by all other clinics.
Another important feature of surgical treatment in our clinic is the possibility of angiography during surgery. We definitely conduct a contrast study after aortofemoral bypass surgery in order to assess the hemodynamic correctness of the vascular reconstruction and identify possible problems. This approach increases the possibility of performing the operation and improves immediate results.
The use of intraoperative angiography makes it possible to operate on patients with severe calcification of the abdominal aorta, which does not allow the use of conventional methods of vessel clamping. To control bleeding, we use inflating a special balloon in the aorta, which allows us to block the blood flow while the vascular graft is sutured to the aorta. The balloon is passed through an access on the arm. The same technique allows us to successfully operate on ruptured abdominal aortic aneurysms.
The results of aortofemoral bypass surgery in our clinic are very good. Treatment success is achieved in 97% of patients with damage to the aortoiliac segment.
Advantages of treatment at the ISC
The Innovative Vascular Center is the only clinic in our country where unique microsurgical, endovascular and plastic methods are comprehensively used to treat patients with incipient gangrene and diabetic foot. Vascular surgeons at our clinic successfully use the method of restoring blood circulation in the limb using a microscope, developed at the University Hospital of Aachen (Germany), for patients with damage to the small arteries of the leg and foot. This is a microsurgical bypass of the arteries of the leg and foot using the patient’s own saphenous vein. Microsurgery allows the successful connection of vein grafts and the smallest vessels with high quality. This allows doctors at our clinic to save limbs for patients already sentenced to amputation.
Since 2011, our clinic has been a leader in Russia in the use of bypass surgery of the arteries of the leg and foot and has the best results in preserving limbs against the background of atherosclerosis of small arteries.
Preoperative preparation
Before surgery, a complete examination of all vascular beds is necessary. If ulcers or erosions of the stomach are detected, preliminary treatment is carried out. The oral cavity must be sanitized. Clarification of the picture of vascular damage is achieved using computed angiography (MSCT). If significant lesions of the carotid or coronary arteries are identified, the issue of preferential revascularization of these areas before surgery on the aorta is decided. Before surgery, it is necessary to correct all existing disturbances in protein and electrolyte metabolism and increase the level of hemoglobin in the blood. On the eve of the operation, it is necessary to cleanse the intestines with a special preparation and enemas. Dinner the night before surgery should be very light. The surgical field (abdomen, thighs) is carefully removed from hair. The patient is given sedatives to relieve anxiety before surgery.
How to prepare
General rules for preparing for surgery require giving up tobacco and alcohol at least 2 days before the procedure (ideally, completely). This measure will avoid respiratory complications after surgery and the risk of heavy bleeding.
In addition, you need to limit the use of hormonal drugs and certain medications, take tests (blood tests for general and special indicators), and undergo fluorography. Hair should be removed at the site of future surgery (if any). This will prevent infection.
The doctor may also prescribe additional examinations based on the patient’s health. For example, in the presence of a number of chronic diseases. Such a measure makes it possible to obtain an accurate picture of the state of the body.
Pain relief during aortofemoral bypass surgery
In our clinic, surgery is usually performed under epidural anesthesia. A special catheter is installed in the back, through which an anesthetic drug is supplied. Complete pain relief and muscle relaxation for retroperitoneal access are achieved. For the purpose of sedation (calming), the patient is given mild sedatives. During operations on the thoracic aorta, general anesthesia is used. The anesthesiologist continuously monitors blood pressure and oxygen saturation. For adequate administration of drugs, a subclavian venous catheter is installed in the patient. The bladder is drained with a catheter to monitor kidney function.
Options for aortofemoral bypass surgery
Aortofemoral bypass surgery can be performed in two options:
- Bilateral aortofemoral bypass surgery (aorto-bifemoral). This option involves restoring blood flow to both legs when both iliac arteries are blocked. The main branch of the prosthesis is sutured to the aorta, the branches of the prosthesis are sutured to the femoral arteries. 3 accesses are performed, two of them in both groin areas, one large on the left side.
- Unilateral aortofemoral bypass surgery is performed when one of the iliac arteries is blocked. Accordingly, only two accesses are required. One is carried out in the groin area on the affected leg, the other on the left side to the aorta.
For the operation to be successful, it is necessary to ensure good blood flow from the prosthesis; sometimes the arteries in the thigh are severely affected. In these cases, our clinic uses two-story bypass methods, when a connection is created in the groin area between the prosthesis and the most suitable artery, after which a shunt is launched further from the prosthesis from the great saphenous vein into the underlying arteries on the leg. Thus, the blood flow from the prosthesis is distributed throughout the leg and there is no stagnation of blood, leading to thrombosis and blockage of the prosthesis. If there is severe damage to the arteries in the groin, it is possible to perform femoral artery replacement. This made it possible to restore blood flow in poor condition of the peripheral vascular bed.
Indications for surgery
Occlusion of the popliteal artery is often combined with narrowing and blockage of the femoral artery, which provokes the development of particularly severe symptoms. Pain suddenly appears in the limb, significant hyperemia and hyperthermia, intermittent claudication, and hair loss throughout the lower leg area are observed. Femoral-tibial bypass surgery is often used as a preventive measure when there is a risk of progression of lower extremity ischemia and the threat of gangrenous tissue changes. As a result of a correctly performed operation, a favorable outcome is observed in 90% of patients with the initial stage of necrosis against the background of critical ischemia. Almost all patients retain the ability to walk on their leg.
Main objectives of the operation:
- Elimination of pain in the affected limb;
- Prevention of tissue death and the formation of trophic ulcers;
- Prevention of gangrene;
- Therapy for intermittent claudication;
- Restoring proper blood supply to the legs.
In most cases, timely femoral-tibial bypass surgery helps avoid amputation.
Progress of aortofemoral bypass surgery
In our clinic, the preferred surgical approach is the Rob retroperitoneal incision; it has significant advantages compared to traditional laparotomy (access through the abdominal cavity). With the Rob approach, the lumbar nerves are not damaged and the intestines are not injured. This allows patients to begin feeding the very next day after surgery, and within a day they can already get out of bed.
After isolating the abdominal aorta, the degree of its damage by the atherosclerotic process is assessed. The operation involves isolating the aorta above the lesion through an incision on the side wall of the abdomen and the femoral arteries in the upper thighs. An artificial vessel made of an inert plastic material that does not cause a reaction in the surrounding tissue is sewn into a plaque-free area of the aorta. Then the branches of this vascular prosthesis are brought out to the femoral arteries and sutured into lesion-free areas. In this way, the blocked area is bypassed and the blood easily enters the legs.
Briefly about the treatment method
Vascular bypass (Bypass) is an operation to create a bypass when a vessel is blocked by atherosclerotic plaques or blood clots.
Arterial bypass surgery is used for severe forms of arterial circulatory insufficiency. Bypass surgery allows you to save a limb in case of gangrene. A shunt is placed from the artery above the blockage to the artery below the lesion, completely restoring blood supply to the affected organ. Most often, to bypass the arteries of the lower extremities, the patient's own saphenous veins are used, which are treated in such a way as to carry blood to the leg, and not back.
Possible complications of aortofemoral bypass surgery
Abdominal aorta surgery is a major surgical procedure. Correct determination of indications can reduce the risk of an unfavorable outcome of the operation. Mortality after reconstructive surgery on the aortoiliac arterial segment is about 3%. The main complications of aortofemoral bypass surgery:
- Bleeding during or after surgery
Bleeding is the most dangerous complication, since the abdominal aorta is the largest vessel in the body and blood loss can be very significant. The cause of bleeding is most often technical difficulties during surgery - the patient is too heavy, scar processes after previous interventions, atypical vascular anatomy. All bleeding that occurs during surgery must be reliably stopped. The surgeon cannot close the surgical wound if there is even the slightest doubt about the final stop of bleeding. After the operation, a drainage must be left in place for a day to control the bleeding situation. With proper surgical technique, the risk of bleeding during aortobifemoral bypass surgery is negligible.
- Cardiovascular failure
In weakened patients with severe concomitant diseases, the inclusion of a large volume of the vascular bed, which occurs with successful aortofemoral bypass, can lead to increased demands on cardiac activity. The heart must pump a larger volume of blood, for which it is not always ready. To correct cardiac weakness in the early postoperative period, drugs that stimulate cardiac activity are used. Patients after aortofemoral bypass surgery require intensive monitoring in the first 2-3 days after surgery to prevent the development of myocardial infarction.
- Effect of turning on ischemic limbs
If aortofemoral bypass surgery was performed for critical ischemia, then the leg tissues were in a state of half-life, the processes of protein breakdown, pre-gangrenous and gangrenous changes began. A sudden start of blood leads to the leaching of incomplete metabolic products from the tissues, which can have a toxic effect on the body. Most often this is manifested by changes in the activity of liver enzymes and kidney tests. There may be an increase in body temperature, increased breathing and heart rate.
- Deep vein thrombosis and pulmonary embolism
Lack of blood circulation, which has existed in the legs for a long time, leads to the formation of blood clots in the small and large veins of the legs. Restoration of blood circulation can cause increased blood flow in the veins and lead to the “washing out” of small blood clots with their transfer to the lungs with the development of thromboembolism. To prevent this complication, heparin is prescribed and the patient is mobilized as quickly as possible.
- Formation of lymphatic collections and lymphatic drainage
A rare complication that develops when the lymph nodes in the groin areas are damaged, when large accumulations of lymph form in the subcutaneous tissue. The complication is unpleasant, but if managed correctly it is low-risk. It is necessary to persistently puncture lymph accumulations, preventing them from becoming infected. Gradually, the accumulation of lymph will decrease and the problem will be resolved.
- Suppuration of postoperative wounds
A complication that can develop due to poor surgical technique, technical difficulties due to scar processes, violation of asepsis rules, and the presence of an infectious process in the inguinal lymph nodes. Suppuration of postoperative wounds is dangerous due to the possibility of suppuration of vascular prostheses. If it is superficial, it must be drained immediately. If a vascular prosthesis is involved in the purulent process, then it should be removed as much as possible and replaced with another, bypassing the purulent wound. In general, suppuration of vascular prostheses is the most difficult complication in vascular surgery and requires great courage and resourcefulness from surgeons in treatment.
- Vascular prosthesis thrombosis
It usually develops either in the first days after surgery or after several months or years. The main cause of thrombosis after aortofemoral bypass surgery is a violation of the outflow of blood from the prosthesis. This happens when the size of the prosthesis is inadequately selected for the efferent artery, or the receptive bed is underestimated. In our clinic, a mandatory ultrasound assessment of blood flow through the shunt and the outlet artery is performed. If a discrepancy between inflow and outflow is detected, additional methods of unloading the shunt are performed. Most often these are additional shunts to the arteries of the leg. Late thrombosis can develop due to the development of scar tissue in the anastomoses of vessels with the prosthesis. To identify such narrowings, all patients after ABBS need to undergo ultrasound examination of vascular reconstruction twice a year. If signs of impaired blood vessel patency are detected, additional vascular correction is necessary.
Surveillance program
Repeated examinations by a vascular surgeon and ultrasound are performed 3 months after discharge, and then annually. During follow-up examinations, the function of the shunt, the adequacy of blood flow in the legs, and whether the patient is taking the prescribed antithrombotic therapy are assessed correctly.
The most commonly prescribed medications are antithrombotic drugs - Plavix, ticlopidine, aspirin. Of the physical therapy methods, the most effective is therapeutic walking 3-5 km per day or cycling. It is important to protect your legs from various microtraumas and abrasions, especially if you have diabetes.
The basis for a successful life after aortofemoral bypass surgery is physical activity, taking antithrombotic drugs and regular examination by the attending physician with ultrasound monitoring of the function of the shunt. If narrowing of the shunt is detected, endovascular correction must be performed. When you follow these instructions, you will forget about the risk of gangrene from atherosclerosis.
After the procedure
Upon completion of the surgical intervention, the patient is transferred to the recovery room for one day. At this time, he is observed by doctors (anesthesiologist and surgeon). Prevention of intestinal paresis is prescribed. Then the operated patient is transferred to the general ward, where he remains for up to 7 days. After this period, the sutures are removed and the patient is prepared for discharge.
The reliability and lifespan of the shunt depend on compliance with medical prescriptions. First of all, you should stop smoking and see a doctor regularly and undergo periodic ultrasounds. To prevent the development of atherosclerosis, from time to time they normalize metabolic processes and reduce cholesterol levels.