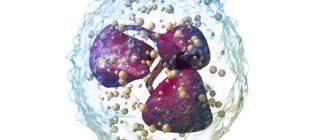
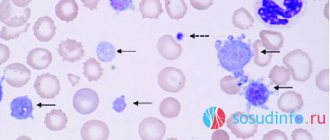
Segmented neutrophils in a child’s body perform the same role as in an adult—they participate in humoral and tissue immunity. This type of blood cell belongs to the leukocyte group and is part of the granulocyte family along with eosinophils and basophils.
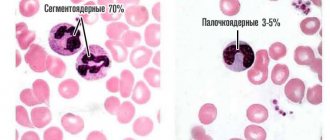
The division of neutrophils into 2 types (segmented and band) is determined by the structure of the nucleus. Early, underdeveloped forms have a rod-shaped nuclear structure. There are significantly fewer of them in the blood than mature segmented cells.
Tasks of neutrophils
Neutrophils, together with lymphocytes, are the main “attacking” link of the immune system. They can move freely not only along the bloodstream, but also pass through the vascular wall into the tissue. This ability to move is provided by false “legs” in the form of a protrusion of the wall.
When approaching a bacterium, the cells surround it with their protoplasm, draw it inside and dissolve it. In this case, the neutrophils themselves die. They are replaced in the bone marrow of children by millions of new ones, to whom information about the affected “enemy” is transmitted. Segmented cells can destroy bacteria and fungal infections, but are powerless to fight viruses.
An increase in the number of segmented leukocytes in a child’s blood test during an infectious disease indicates a good protective reaction of the baby, the ability to resist pathological organisms.
A decrease in cells relative to the norm causes concern for the doctor and indicates low immunity.
Where are neutrophils formed and what are they responsible for?
Leukocyte granulocytes participate in the body's immune defense against pathogenic environmental factors. Neutrophils are divided into “mature” – segmented and “immature” – precursor cells. In infectious diseases, segmented cells provide immune protection.
The main functions of neutrophil granulocytes:
- Destruction of pathogenic microorganisms (bacteria, fungi) and, to a lesser extent, viruses.
- Regulation of inflammatory processes.
- Control of proliferation of intestinal, epithelial and reproductive microflora.
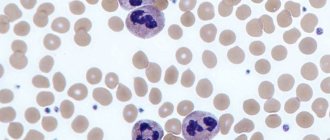
Before becoming mature neutrophils, cells go through developmental stages. Leukocyte granulocytes are synthesized by red bone marrow and then diffuse into the bloodstream. Stages of neutrophil differentiation:
- Myeloblasts and myelocytes are formed.
- After maturation, the myelocyte leaves the red bone marrow and begins to circulate in the bloodstream. There the further development of the cell continues. The myelocyte differentiates into band neutrophils.
- At the last stage of differentiation, segmented neutrophil granulocytes appear, which provide complete immune protection of the body.
Bone marrow
What quantity is considered normal?
Until the child grows up, his leukocyte count will differ from adults in the absolute and relative content of neutrophils. If in an adult the level of segmented cells is in the range of 47–75% of all leukocytes with the presence of “rods” from 1 to 6%, then in childhood it fluctuates, depending on the period of life.
Norms of segmented neutrophils in a child
| Age | Level of segmented cells in % |
| neonatal period | from 45 to 80 |
| up to 12 months | from 15 to 45 |
| from one year to 12 years | from 25 to 62 |
| in adolescence | from 40 to 65 |
At the same time, the number of band forms drops from 17% to adult norms.
Features of blood and hematopoietic organs in children
The entire hematopoietic system of a child is characterized by extreme functional instability (lability), easy vulnerability to the most insignificant exogenous factors.
A decrease in the amount of hemoglobin, red blood cells, the appearance of immature elements of red blood, leukocytosis with the formation of young cells are observed in children much more often and develop faster than in adults. The formation of foci of extramedullary hematopoiesis, and sometimes a complete return to the embryonic type, can be caused in children not only by severe anemia and leukemia, as in an adult, but often occur under the influence of various infections, intoxications and other harmful factors (bronchopneumonia, pyelonephritis, otitis media and etc.). Blood for infections, analysis - children's clinic "Markushka"
Peripheral blood of a healthy child
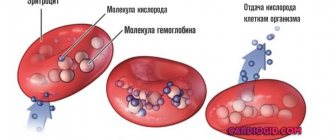
Erythrocyte system : erythropoiesis begins with a bone marrow stem cell that is sensitive to erythropoietin (a glycoprotein produced in response to tissue hypoxia in the fetal liver and the child’s kidney), and proceeds through its differentiation into an erythroblast, then into a pronormocyte, basophilic normocyte, polychromatophilic normocyte, oxyphilic normocyte, reticulocyte.
Of the estimated 18 divisions that occur during the transformation of a stem cell into a mature red blood cell, erythropoietin significantly stimulates the final 8-10 divisions. The preceding cell divisions that give rise to erythropoietin-sensitive erythroid progenitor cells are largely erythropoietin-independent.
The lifespan of red blood cells is 100-120 days. With the help of phagocytic macrophages of the spleen, liver, lungs, and lymph nodes, an average of 1.4% of red blood cells are destroyed per day.
Composition of peripheral blood in a child
The composition of a child's peripheral blood undergoes significant changes in the first days of life after birth. Immediately after birth, red blood is characterized by an increased hemoglobin content and a large number of red blood cells. From the end of the 1st to the beginning of the 2nd day of life, a decrease in the content of hemoglobin and red blood cells occurs.
The blood of a newborn by a distinct anisocytosis, observed within 5-7 days, and macrocytosis (the diameter of erythrocytes is somewhat larger in the first days of life - up to 8.5-9 µm, the norm is 7.5 µm). The blood of a newborn contains many young red blood cells, which indicates the active processes of erythropoiesis. During the first few days of life, it is possible to detect nucleated forms of erythrocytes in the blood, most often normocytes and erythroblasts. The number of reticulocytes in the first hours of life ranges from 8 to 42%. The high content of erythrocytes and hemoglobin, as well as immature forms of erythrocytes in the peripheral blood in the first days of life indicates intensive erythropoiesis as a reaction to the lack of oxygen supply to the fetus during intrauterine development and during childbirth.
After birth, due to the establishment of external respiration, hypoxia is replaced by hyperoxia
After birth, due to the establishment of external respiration, hypoxia is replaced by hyperoxia . This causes a decrease in erythropoiesis and a drop in the number of red blood cells and hemoglobin levels. Red blood cells produced in utero have a shortened lifespan compared to that of older children and are more prone to hemolysis. The lifespan of red blood cells in children in the first days of life is 12 days, which is 10 times less than in adults and older children.
The erythrocyte sedimentation rate (ESR) depends on many chemical and physical properties of the blood. In a newborn, ESR is 2 mm/h, in young and older children - 4-8 mm/h, in adults - 5-8 mm/h. Slower erythrocyte sedimentation in newborns is explained by low levels of fibrinogen and cholesterol in the blood, as well as blood thickening, which is especially pronounced in the first hours after birth.
Leukocyte system
Leukocyte system : leukopoiesis begins with a bone marrow stem cell and proceeds through its differentiation into a myeloblast, then into basophilic, neutrophilic and eosinophilic segmented cells through the phases: promyelocyte - myelocyte - band cells.
Neutrophils are continuously supplied to the skin, mucous membranes and other peripheral tissues. Their daily turnover is about 100 billion cells. The lifespan of granulocytes is from 14 to 23 days. Neutrophils spend most of their lives in the bone marrow. On their way to peripheral tissues, neutrophils spend about 10 hours in the intravascular space, and at any moment only half of the intravascular cells are in motion, while the other reversibly adheres to the endothelial surface of the vessels (mural cells). The latter are a reserve pool of mature cells that can be called upon in case of infection or inflammation.
Features of the number of leukocytes
There are features and numbers of leukocytes . In the peripheral blood in the first days after birth, the number of leukocytes is 18-20 -109/l, with neutrophils predominating (60-70%). The leukocyte formula is shifted to the left due to a large number of band forms and, to a lesser extent, metamyelocytes (young).
With age, the leukocyte formula undergoes significant changes
This is reflected in a decrease in the number of neutrophils and an increase in the number of lymphocytes . On the 5th day of life, their number is comparable (the so-called first crossover), amounting to about 40-44% in the white blood formula with a ratio of neutrophils and lymphocytes of 1:1. Then there is a further increase in the number of lymphocytes (by the 10th day to 55-60%) against the background of a decrease in the number of neutrophils (approximately 30%). The ratio between neutrophils and lymphocytes will be 1:2.
Gradually, by the end of the 1st month of life, the shift of the formula to the left disappears, myelocytes completely disappear from the blood, the content of band forms decreases to 4-5%.
By the beginning of the 2nd year of life, the number of lymphocytes begins to decrease, and the number of neutrophils increases, respectively, by 3-4% of cells per year, and at 5 years a “second crossover” is observed, in which the number of neutrophils and lymphocytes is again compared (1:1 ratio) . After 5 years, the percentage of neutrophils gradually increases by 2-3% per year and by 10-12 years reaches values like those of an adult - about 60%. The neutrophil to lymphocyte ratio is again 2:1.
This parallelism of changes in neutrophils and lymphocytes can be explained by the commonality of their functional properties, which play a role in immunity. The lifespan of lymphocytes is 100-300 days.
Absolute and relative neutrophilia in the first days after birth is explained by the entry of maternal hormones into the child’s body through the placenta, thickening of the blood in the first hours of extrauterine life, resorption of interstitial hemorrhages, and adaptation of the body to external conditions.
The content of eosinophils, basophils, and monocytes practically does not undergo significant changes during the growth of the child. The number of leukocytes further decreases to (7.6-7.9)x10(9)/l.
Platelets
Platelets , like all other blood cells, originate from a bone marrow stem cell with subsequent differentiation: thrombopoietin-sensitive cell - megakaryoblast - promegakaryoblast - megakaryocyte - platelet. About 35-40% of circulating platelets are destroyed daily due to aging and the body's ongoing clotting process.
Platelets are directly involved in the process of hemostasis. The activity of platelet coagulation factors in newborns and infants is reduced. The duration of bleeding is not changed, the clotting time may be prolonged, especially in children with severe jaundice (over 6-10 minutes).
Hematocrit number , which gives an idea of the percentage ratio between formed elements and blood plasma, varies depending on age. The hematocrit value increases in cyanotic congenital heart defects, in a state of dehydration, etc. A decrease in hematocrit is observed in anemia and diseases accompanied by hydremia.
Peripheral blood in premature infants
The red blood of a healthy premature baby at birth is characterized by erythroblastosis, reticulocytosis, increased red blood cell and hemoglobin counts, as well as anisocytosis and poikilocytosis. Soon after birth, there is a gradual drop in the content of red blood cells and hemoglobin, and by the 2-3rd month of life, most preterm infants develop anemia, known as “early anemia of prematurity.” Its pathogenesis is based on increased hemolysis and functional immaturity of bone marrow hematopoiesis. The cause of intense hemolysis is the predominance of unstable red blood cells containing fetal hemoglobin in the blood of premature babies.
Thus, in healthy premature infants, anemia in the 2-3rd month of life can be considered as a manifestation of adaptation when replacing extramedullary hematopoiesis with bone marrow. In sick children, early anemia is often accompanied by more pronounced changes in the content of red blood cells and hemoglobin and has a long course.
By the beginning of the 4th month, there is a spontaneous increase in the level of red blood cells and hemoglobin, but a month later there is a repeated decrease in levels and late anemia of prematurity develops, caused by a lack of iron in the body. Unlike early, late iron deficiency anemia can be prevented and effectively treated with iron supplements.
Blood in children after one year of age
Blood in children over the age of one year also has its own characteristics. The amount of hemoglobin in children over 1 year of age clearly increases, gradually approaching the figures of an adult, although at this age there are significant individual fluctuations. The number of red blood cells also increases in parallel; their absolute quantities and growth rates in children of different ages are subject to fairly wide individual fluctuations. The number of erythrocytes with supravital granularity gradually decreases, reaching by school age the figures characteristic of adults, that is, about 2%. The color index ranges from 0.85 to 0.95.
It should be noted that recently, in both children and adults, some changes : a trend towards a decrease in the number of leukocytes is definitely emerging (in children aged 2 to 15 years).
When neutrophils are elevated in children
The condition of increased neutrophil levels is called neutrophilia or neutrophilosis. Elevated values in a child may be associated with a reaction to a recent vaccination or the use of medications (steroid hormones).
Conscious toddler
The growth of neutrophilia is possible with the following pathology:
- bacterial infections (angina, inflammation of the middle ear, pneumonia, acute appendicitis, peritonitis, septic condition);
- the presence of pustules (abscesses, phlegmon);
- in case of severe skin burns;
- with hemolytic anemia;
- for acute and chronic leukemia.
Norms for the number of neutrophils in the blood in children of different ages
The normative volume of neutrophils depends on the age of the child; after 15 years, adolescents correspond to adult values. Normally, in children, blood from a finger does not contain young cells; their appearance indicates a shift in the leukocyte formula to the left. The normal content of mature neutrophils (band and segmented) is shown in the table.
| Age | Segmented, % | Bands, % | Total number of neutrophils per liter of blood (x109) |
| After birth | 47-70 | 3-12 | 1,5-8 |
| 2 weeks | 30-50 | 1-5 | 1,8-8,5 |
| Up to a year | 15-45 | 1-5 | 1,8-8,5 |
| 1-2 years | 30-45 | 0,7-5 | 2-6 |
| 2-5 years | 30-55 | 0,7-5 | 2-6 |
| 6-7 years | 40-60 | 0,7-5 | 2-6 |
| 9-11 years | 45-60 | 0,7-5 | 2-6 |
| 12-15 years | 50-70 | 0,7-5 | 2-6 |
READ ALSO: band neutrophils in the blood of a child: what to do if their content is increased?
Decreased neutrophils
A decrease in the number of cells in a row is called neutropenia. The level of segmented neutrophils decreases in three cases of the pathology mechanism:
- if too many cells die in a protective reaction;
- if their production in the bone marrow is blocked;
- when cells are destroyed during diseases of the hematopoietic organs.
Similar conditions in children are possible:
- with severe anaphylactic reaction;
- for viral infectious diseases (measles, influenza, rubella, respiratory diseases, mumps, viral hepatitis) that suppress general immunity;
- for various anemias;
- after radiation therapy;
- when painkillers and anticonvulsants are used in treatment.
A decrease in the indicator is observed in cases of poisoning with household chemicals.
Particular diagnostic importance is attached to the condition when neutrophils are low and lymphocytes are high. Lymphocyte cells respond to viral infection. A similar combination is found in the child’s blood:
- during a viral disease;
- for tuberculosis;
- if there is hyperfunction of the thyroid gland;
- in HIV-infected children;
- for malignant blood diseases (lymphocytic leukemia, sarcoma).
If such deviations do not last long and return to normal on their own as you recover, you can think about completely restoring the immune system. Long-term changes require repeated tests and additional examination of the child.
We are trying to recover as quickly as possible
There is a rare genetic blood disease that is detected in childhood - Kostman neutropenia. There are no neutrophils in the body. A child deprived of protection is susceptible to frequent infections and pustular diseases. The first year of a baby’s life is especially dangerous. Subsequently, the protective function is carried out by compensatory growth of monocytes and eosinophils.
Why does the number of neutrophils decrease?
A decrease in the number of cells (neutropenia) may be hereditary.
If you know about such characteristics in one of the baby’s parents, you should inform your doctor about it. Other factors that can cause neutropenia:
- deficiency of B vitamins, copper, iron, and other microelements;
- long-term use of analgesics, antispasmodics, cytostatics and some other drugs;
- long-term physical activity;
- stress (usually due to a family situation or difficult living conditions, but can also be caused by school workload);
- bacterial and fungal infections;
- viral diseases (measles, chickenpox, rubella, influenza, HIV, herpes, etc.);
- bone marrow pathologies (bone marrow aplasia or hypoplasia, or hereditary diseases affecting the synthesis of cells and their release into the bloodstream).
How does neutropenia manifest in a child?
If the cause of neutropenia is a long-term infection or taking medications, correction of the treatment of underlying diseases is required. If there is no active pathological process, the stages of treatment depend on the child’s well-being:
Chronic moderate neutropenia or a decrease in the number of neutrophils in children under 3 years of age may not manifest itself. In this case, you should focus on the child’s condition and the pace of his development. In most cases, no special treatment is required.
If the cell level has not stabilized after 3 years, or the child is developmentally delayed, gets tired quickly, has a runny nose, or often suffers from colds for a long time, this is a reason for additional examination and treatment. Perhaps the problem can be solved by vitamin therapy, changing the child’s diet and daily routine.
If the cause is stress or school and extracurricular workload, you need to find a way to get rid of them. You may have to give up some clubs during primary school age. The child will be able to return to them when he grows up and gets stronger.
If a decrease in the number of less than 500 in 1 ml of blood is diagnosed, most doctors consider it appropriate to prescribe antibiotic therapy, even if additional examination does not reveal the causes of the disease.
This measure allows both to extinguish a hidden pathological process and protect the child from possible bacterial infection against the background of decreased immunity. As a rule, such therapy gives a positive result.
How to prepare your child for a blood test for neutrophils
An analysis for segmented neutrophils is done from capillary blood, which is taken from a finger in children, and from a toe or heel in newborns.
You need to bring your child in the morning on an empty stomach, without even giving him tea. Breastfeeding is allowed on a schedule. The baby should be reassured. After the analysis, do not rub your finger or treat it with an apple or banana.
Since your cell levels can be affected by the medications you are taking, it is best to ask your doctor in advance whether you need to stop taking them and for how long.
If the cause of a change in the level of segmented neutrophils is detected in a child, treatment is directed to the underlying disease. In any case, parents are required to comply with the basic requirements for the daily routine and nutrition of their children.
What are neutrophils?
Neutrophils in the blood are one of the types of white blood cells - leukocytes and granulocytes. Being in the blood, they occupy about 75% of the total number of white blood cells.
Neutrophil granulocytes are a very significant component of leukocytes. Their number will necessarily be recorded in the leukocyte formula of the blood, and is designated as neut .
A neutrophil count that does not fall outside the established range indicates that the child’s immune system is functioning correctly. It quite effectively protects the child’s body from bacteria and viruses entering it.