Local therapist
Ablyazov
Irshat Ravilevich
21 years of experience
Local therapist of the highest category. Member of the Russian Scientific Medical Society of Therapists.
Make an appointment
Thrombocytopenia is a separate disease or a symptom of another disease that is characterized by a low platelet count (less than 150,000 units per microliter). The condition is accompanied by high bleeding, as well as slow stopping of bleeding from small vessels.
Symptoms
Symptoms of thrombocytopenia include:
- Purpura. This is the name for hemorrhages in mucous tissues or skin. In fact, it looks like red spots - most often they can be seen in places of strong contact with clothing. The spots do not hurt, they can be pinpoint or quite extensive - including bruises of different colors (depending on the time of formation).
- Regular nosebleeds. Since small vessels are weakened, bleeding can begin due to a cold, sneezing, or minor injury. Bright red blood may flow for ten minutes or more, putting the patient at risk of losing a lot of blood.
- Bleeding gums, prolonged bleeding after tooth extraction. The mechanism is the same: due to weak blood vessels, the blood cannot stop quickly in case of small or large injuries.
- Bleeding of internal organs. For example, blood is found in the gastrointestinal tract, when the stool becomes colored, or in the genitourinary system - then the urine becomes colored. Both symptoms are very alarming and require immediate contact with specialists.
- Too heavy and long menstruation. Moreover, bleeding can be observed on other days of the cycle.
All of these symptoms may indicate other diseases - both concomitant with thrombocytopenia and independent. What complicates the situation is that there are a lot of reasons and mechanisms for the development of this condition. In medicine, there are several types of this disease.
Classification of thrombocytopenia
Let's talk about the causes of thrombocytopenia that underlie the different types of this disease.
Hereditary thrombocytopenias
These conditions are based on diseases of genetic origin. These may be May-Hegglin anomaly, Bernard-Soulier syndrome, Wiskott-Aldrich syndrome, TAR syndrome, as well as congenital amegakaryocytic thrombocytopenia.
Each of these diseases has many characteristics. For example, Wiskott-Aldrich syndrome occurs exclusively in boys and occurs in four to ten cases per million. Bernard-Soulier syndrome can only develop in a baby who has received the altered gene from both parents, and May-Hegglin anomaly can develop in 50% of cases, provided that only one parent has the prerequisites for this. As a rule, all of these diseases have among their symptoms not only a low level of platelets, but also a number of other pathological conditions, and therefore require special treatment.
How to avoid bleeding
Cancer and cancer treatments can cause low platelet counts. When your platelet count is low, you are at risk of bleeding. If your doctor has told you that you have a low platelet count, it is important to try to avoid injury.
We will list some general tips that can help you prevent bleeding. It is also very important to discuss your lifestyle with your healthcare professional. They may suggest other ways to prevent bleeding if your platelet count is low.
Personal care
- Do not use sharp objects such as straight razors, scissors or nail clippers. You can use an electric razor.
- Do not: manicure or pedicure;
- waxing;
- electrolysis;
- tattoos
- rectal suppositories (medicines that are inserted into the anus);
Dental care
- Use a brush with soft bristles.
- Consult your doctor before starting dental treatment.
Daily Activities
- Wear gloves when doing gardening, cooking, or making repairs at home.
- Avoid activities that could cause injury. These include: contact sports;
- climbing a stepladder;
- intense physical exercise;
- Biking;
- lifting weights.
- use lubricants if necessary;
Medicines
- Do not take: aspirin or medications containing aspirin;
- nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil®, Motrin®) and naproxen (Aleve®);
- vitamin E
to come back to the beginning
Productive thrombocytopenia
They are also caused by a huge list of reasons and factors of various origins. All of them are associated with the fact that platelet formation processes in the red bone marrow are disrupted.
For example, this includes some types of anemia, cancer metastases, acute leukemia, and taking cytostatic medications. There are even factors such as radiation or alcohol abuse.
For example, in acute leukemia, a disease of the circulatory system causes a mutation in the bone marrow stem cell. Because of this, it divides and begins to displace hematopoietic cells. As a result, the number of not only platelets, but also leukocytes, erythrocytes, and lymphocytes decreases. This condition has its own name - pancytopenia. That is, immune thrombocytopenia in this case is part of it.
If we are talking about the effect of medications, then most often a decrease in platelet levels is caused by drugs from the following groups:
- antidiabetic,
- anti-inflammatory,
- antipsychotics,
- antithyroid,
- antibiotics,
- diuretics,
- anticonvulsants.
Of course, not all medications and not in all cases are capable of causing such a reaction, but this is another reason to think about the fact that you should not prescribe any medications yourself or take them without the supervision of your doctor.
Moreover, there is also such a factor as increased sensitivity to certain medications. Usually it is initially determined by a peculiar genetic predisposition, but this is quite rare.
When we talk about radiation, we are talking not only about a person’s presence in dangerous areas, but also about treatment with radiation therapy. When tumors are destroyed, the blood-forming cells of the red brain can be affected, so a condition where platelet levels drop can become a side effect of cancer treatment.
The development of symptoms of thrombocytopenia due to alcohol abuse most often occurs against the background of binge drinking and is associated with a high level of ethyl alcohol in the blood. It has negative and long-lasting effects on the bone marrow and usually causes a temporary decrease in platelets. If binge drinking becomes frequent and too long, there is a risk that the changes will be irreversible.
What does a low level of thrombotic cells indicate in an adult?
Unlike red blood cells, whose life cycle is approximately 120 days, thrombotic plates are destroyed on days 9-12 of their existence. Their quantity is continuously renewed by the bone marrow to maintain the physiologically necessary amount in the blood.
As with other blood cells, platelets have values called normal; they are defined in the range 180-320*10 9 units per liter, or 180-320 thousand units per microliter. If, according to the results of the analysis, it turns out that the number of thrombotic cells does not reach the normal level, this indicates the development of thrombocytopenia in an adult or child.
Thrombocytopenia (platelets significantly lower than normal) occurs due to the accelerated destruction of thrombotic cells or disruption of their production, which occurs in a number of diseases.
Thrombocytopenia destruction
Here we are talking about the active destruction of platelets, which is usually observed in the spleen. Such processes are also caused by a large number of factors. These include taking certain medications, some viruses, Fisher-Evans syndrome, etc.
Idiopathic thrombocytopenia deserves special consideration. This is the case when it is not possible to establish the cause even with a huge number of possible options. At the same time, doctors note that even in such a situation, the action of provoking factors is observed. For example, the problem appears after bacterial and viral infections, preventive vaccinations, use of a number of medications, hypothermia or prolonged exposure to the sun.
This condition also occurs in newborns. It begins to form in the womb, when antibodies in her body cause the destruction of platelets in the child.
Fisher-Evans syndrome is also not an independent cause, since it itself is a consequence of various systemic diseases. This syndrome occurs in systemic lupus erythematosus and rheumatoid arthritis, but in some cases it can be an independent deviation. As for viruses, rubella, chicken pox, measles, and influenza can lead to a decrease in platelet levels. Sometimes this is a reaction to vaccination, although such a mechanism is described quite rarely and almost never occurs.
What does this mean during pregnancy?
Among the physiological causes of low platelets in women, pregnancy is named, and for the early stages this is indeed a normal situation, if we are talking about acceptable low values. In the early stages, pregnant women experience an increase in the volume of circulating blood due to plasma, while the mass of red blood cells and platelets is produced at a less rapid pace. As a result, the effect of hemodilution is observed - blood thinning, accompanied by a reduced content of red blood cells and platelets.
Typically, this transient phenomenon does not have any significant impact on hemostasis. If platelets are reduced to a level of 50 units per microliter or lower, emergency measures may be required to stabilize the indicators. Especially if there are few platelets a couple of weeks before giving birth, this means that the body is not preparing for the upcoming blood loss and can suffer greatly during childbirth.
- Thrombocytopenia - symptoms and treatment
This is when the value of a general blood test becomes obvious - thanks to it, it is possible to promptly detect a low platelet count, suggest the reasons for the deviation and take action.
The range of conservative methods for increasing low platelets during pregnancy is limited, but the expectant mother will not be left without help, since the arsenal of medicine includes drugs with minimal effects on the fetus.
Thrombocytopenia consumption
Here the mechanism is as follows: platelets, for some reason, begin to be activated in the vascular bed. In response to this, the red bone marrow begins to actively produce them - and as a result, its capabilities are slowly depleted. After this, the level of red cells begins to fall.
One of the causes of consumption thrombocytopenia is disseminated intravascular coagulation syndrome. It stands for disseminated intravascular coagulation syndrome. And it can develop against the background of severe tissue destruction during operations, burns, injuries, due to severe infections, chemotherapy, organ transplants, etc. That is, there are many underlying reasons that can cause a decrease in the level of platelets in the blood.
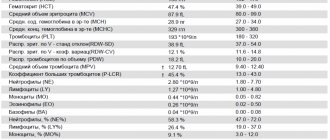
General clinical blood test
It is carried out as part of a general clinical examination of the patient and allows you to learn about the condition of the blood and the body as a whole. The main indicators of this analysis are: hemoglobin, the number of leukocytes (white blood cells), erythrocytes (red blood cells) and platelets (nuclear-free plates of blood responsible for clotting).
Due date and how to prepare
A general blood test is taken in the morning on an empty stomach, often from a finger, less often from a vein. You should not drink or eat 4 hours before the test.
Metrics collected
Now a general blood test is carried out on automatic hematological analyzers, which can simultaneously determine values from 5 to 24 parameters.
The main indicators collected are:
- Hemoglobin (HGB - hemoglobin)
- the main component that is involved in the transfer of oxygen in the blood from the lungs to organs and tissues, and carbon dioxide back to the lungs, is the blood pigment of red blood cells. - Red blood cells (RBC - red blood cells)
are red blood cells that carry oxygen in the blood to organs and tissues. - Leukocytes (WBC - white blood cells)
are white blood cells produced in the bone marrow that carry out immune control and protect the body from foreign cells. - Thrombocytes (PLT - platelets)
are nuclear-free platelets of blood responsible for clotting. - Lymphocytes (LYM - lymphocyte)
are cells of the immune system that respond to viruses and microbes. - Monocytes (MON - monocyte)
are large cells of the immune system. - Hematocrit (HCT - hematocrit)
is the volume of red blood cells in the blood. - Blood color index (BI)
, demonstrating the concentration of hemoglobin in red blood cells. - Erythrocyte sedimentation rate
, which, if deviated from the norm, may indicate a pathological condition of the body. - Various erythrocyte, leukocyte and platelet indices
.
Decoding the results: norm and deviation
The normal values of the blood parameters studied in each laboratory are different and depend on the gender, age and condition of the patient. Only a doctor can make a correct interpretation of the blood test results and make a diagnosis, taking into account all aspects of the patient’s health. Below are frequently examined blood parameters, their normal values, and what a deviation from the norm may indicate in the general case, and not in the specific case. To obtain an individual interpretation and diagnosis, you should consult a doctor.
Hemoglobin (HGB - hemoglobin)
Normal hemoglobin level in blood:
Men:
- from 12 to 15 years: 120 - 160 g/l;
- from 15 to 18 years: 117 - 166 g/l;
- from 18 to 45 years: 132 - 173 g/l;
- from 45 to 65 years: 131 - 172 g/l;
- over 65 years old: 126 - 174 g/l.
Women:
- from 12 to 15 years: 115 - 150 g/l;
- from 15 to 18 years: 117 - 153 g/l;
- from 18 to 45 years: 117 - 155 g/l;
- from 45 to 65 years: 117 - 160 g/l;
- over 65 years old: 120 - 161 g/l.
Children:
- up to 2 weeks: 134 - 198 g/l;
- from 2 to 4.3 weeks: 107 - 171 g/l;
- from 4.3 to 8.6 weeks: 94 - 130 g/l;
- from 8.6 weeks to 4 months: 103 - 141 g/l;
- at 4 to 6 months: 111 - 141 g/l;
- from 6 to 9 months: 114 - 140 g/l;
- from 9 to 1 year: 113 - 141 g/l;
- from 1 year to 5 years: 100 - 140 g/l;
- from 5 years to 10 years: 115 - 145 g/l;
- from 10 to 12 years: 120 - 150 g/l;
Deviation of hemoglobin in the blood from the norm may indicate:
when decreasing by:
- overhydration - increased water content in the body due to impaired water-salt metabolism;
- anemia - disruption of the oxygen transport function in the body and the development of hypoxia.
when increasing by:
- dehydration - loss of water in the body;
- polycythemia vera - increased blood viscosity and decreased blood flow;
- excessive smoking.
Red blood cells (RBC - red blood cells)
Norm of red blood cells in the blood:
Men:
- from 12 - 18 years: 4.5 - 5.3 * 10^12/l;
- over 18 years old: 4.0 - 5.0 * 10^12/l.
Women:
- from 12 - 18 years: 4.1 - 5.1 * 10^12/l;
- over 18 years old: 3.5 - 4.7 * 10^12/l.
Children:
- newborn: 3.9 - 5.5 * 10^12/l;
- from 1 to 3 days: 4.0 - 6.6 * 10^12/l;
- in 1 week: 3.9 - 6.3 * 10^12/l;
- in week 2: 3.6 - 6.2 * 10^12/l;
- at 1 month: 3.0 - 5.4 * 10^12/l;
- in the 2nd month: 2.7 - 4.9 * 10^12/l;
- from 3 to 6 months: 3.1 - 4.5 * 10^12/l;
- from 6 months to 2 years: 3.7 - 5.3 * 10^12/l;
- from 2 to 6 years: 3.9 - 5.3 * 10^12/l;
- from 6 to 12 years: 4.0 - 5.2 * 10^12/l.
Normal erythrocyte indices:
- MCV
: 80 - 95 fl - average erythrocyte volume; - MCH
: 27 - 31 pg - average hemoglobin content in an individual red blood cell; - MCHC
: 320 - 360 g/l - average hemoglobin concentration in the erythrocyte mass; - RDW
: 11.5% - 14.5% - red blood cell distribution width; - RDW-SD
: 37 - 54 fl - deviation of the distribution of red blood cells by volume; - RDW-CV
: 11.5 - 14.5% (adults), 14.9 - 18.7% (children up to 6 months) and 11.6 - 14.8% (children over 6 months) - deviation of red blood cell size from averages; - P-LCR
: 13 - 43% - large platelet ratio; - ESR
: 10 mm/hour (men), 15 mm/hour (women) - erythrocyte sedimentation rate, deviation of which from the norm may indicate a pathological or inflammatory process in the body.
Deviation of red blood cells from the norm may indicate:
when decreasing by:
- anemia;
- blood loss;
- pregnancy;
- overhydration;
- decrease in the intensity of red blood cell formation in the bone marrow;
- therapy with diuretics;
- accelerated destruction of red blood cells.
when increasing by:
- burn;
- diarrhea;
- hydrocele of the renal pelvis;
- true polycythemia;
- Cushing's syndrome;
- neoplasms;
- steroid use;
- the effect of corticosteroids;
- taking diuretics.
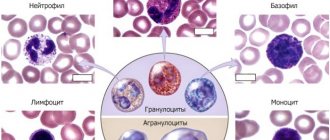
Leukocytes (WBC - white blood cells)
Norm of leukocytes in the blood:
Men and women:
- from 16 years and older: 4.0 - 9.0 * 10^9/l.
Children:
- up to 1 year: 6.0 - 17.5 * 10^9/l;
- from 1 year to 2 years: 6.0 - 17.0 * 10^9/l;
- from 2 to 4 years: 5.5 - 15.5 * 10^9/l;
- from 4 to 6 years: 5.0 - 14.5 * 10^9/l;
- from 6 to 10 years: 4.5 - 13.5 * 10^9/l;
- from 10 to 16 years: 4.5 - 13.0 * 10^9/l.
Norm of leukocyte indices:
- LYM% (LY%)
: 25 - 40% - relative content of lymphocytes; - LYM# (LY#)
: 1.2 - 3.0 * 10^9/l (1.2-3.0 x 10^3/μl) - absolute lymphocyte content; - MXD% (MID%)
: 5 - 10% - the relative content of a mixture of monocytes, eosinophils and basophils; - MXD# (MID#)
: 0.2 - 0.8 * 10^9/l - absolute content of a mixture of monocytes, eosinophils and basophils; - NEUT% (NE%)
: 40% - 75% - relative content of neutrophils; - NEUT# (NE#)
: 2 - 7.5 * 10^9/l - absolute content of neutrophils; - MON% (MO%)
: 4 - 11% - relative content of monocytes; - MON# (MO#)
: 0.1 - 0.6 * 10^9 cells/l - absolute content of monocytes; - EO%
: 1 - 5% - relative content of eosinophils; - EO#
: 0.4 * 109/l - absolute eosinophil content; - BA%
: less than 1% - relative content of basophils; - BA#
: 0 - 0.08 * 10^9/l - absolute content of basophils; - IMM%
: 1 - 5% - relative content of immature granulocytes; - IMM#
: 1.2 - 6.8 * 10^9/l - absolute content of immature granulocytes; - ATL%
: less than 5% - the relative content of atypical lymphocytes; - ATL#
: 0.06 - 0.15 * 10^9/l - absolute content of atypical lymphocytes; - GR% (GRAN%)
: 47 - 72% - relative content of granulocytes; - GR# (GRAN#)
: 1.2 - 6.8 * 10^9/l (1.2 - 6.8 * 10^3/μl) - absolute granulocyte content.
Deviation of leukocytes in the blood from the norm may indicate:
when decreasing by:
- typhus;
- viral diseases;
- bone marrow diseases and damage;
- anaphylactic shock;
- leukemia;
- viral diseases;
- radiation sickness;
- Addison-Biermer disease;
- collagenosis;
- myelodysplastic syndromes;
- hypersplenism;
- myelofibrosis;
- plasmacytoma;
- taking certain antibiotics and anti-inflammatory drugs;
- anemia.
when increasing by:
- the presence of inflammatory processes in the body;
- sepsis;
- purulent processes;
- tissue injuries;
- myocardial infarction;
- infectious diseases;
- the presence of malignant neoplasms;
- last trimester of pregnancy;
- period of feeding the baby with breast milk;
- great physical activity.
Thrombocytes (PLT - platelets)
Normal platelet count in blood:
Men, women and children:
- all ages - 180 - 320 * 10^9 cells/l.
Normal platelet indices:
- MPV (mean platelet volume): 7 - 10 fL - average platelet volume;
- PDW: 9 - 16% - width of platelet distribution by volume;
- PCT (platelet crit): 0.108 - 0.282% - the proportion of blood volume occupied by platelets.
Deviation of platelets in the blood from the norm may indicate:
when decreasing by:
- bronchial asthma;
- malaria;
- thrombocytopenia;
- malignant neoplasm;
- Sumter's syndrome.
when increasing by:
- essential thrombocythemia
Lymphocytes (LYM - lymphocyte)
Norm of lymphocytes in the blood:
Men and women:
- from 16 years and older: 20 - 40%.
Children:
- newborns: 15 - 35%;
- up to 2 weeks: 22 - 55%;
- from 2 weeks to 1 year: 45 - 70%;
- from 1 year to 2 years: 37 - 60%;
- from 2 to 5 years: 33 - 55%;
- from 6 to 7 years: 30 - 50%;
- from 8 to 9 years: 30 - 50%;
- from 9 to 11 years: 30 - 46%;
- from 12 to 15 years: 30 - 45%.
Deviation of lymphocytes in the blood from the norm may indicate:
when decreasing by:
- autoimmune diseases;
- diseases of the nervous system;
- HIV infection;
- side effects from taking medications.
when increasing by:
- viral diseases;
- bacterial infections;
- fungal diseases;
- toxoplasmosis;
- tuberculosis;
- whooping cough;
- vasculitis;
- malignant neoplasms;
- initial stage of HIV;
- excess carbohydrates in the body compared to fats and proteins;
- thyroid diseases;
- starvation.
Monocytes (MON - monocyte)
Norm of monocytes in the blood:
Men and women:
- from 16 years and older: 3 - 9%.
Children:
- newborns: 3 - 12%;
- up to 2 weeks: 5 - 15%;
- from 2 weeks to 1 year: 4 - 10%;
- from 1 year to 2 years: 3 - 10%;
- from 2 to 5 years: 3 - 9%;
- from 6 to 7 years: 3 - 9%;
- from 8 to 9 years: 3 - 9%;
- from 9 to 11 years: 3 - 9%;
- from 12 to 15 years: 3 - 9%.
Deviation of monocytes in the blood from the norm may indicate:
when decreasing by:
- use of immunosuppressants;
- hereditary diseases.
when increasing by:
- stress;
- diabetes;
- atherosclerosis;
- bacterial infections;
- malignant neoplasms;
- sepsis;
- collagenosis;
- sarcoidosis
Hematocrit (HCT - hematocrit)
Hematocrit norm:
Men:
- from 12 to 15 years: 35 - 45%;
- from 15 to 18 years: 37 - 48%;
- from 18 to 45 years old: 42 - 50%;
- from 45 to 65 years: 39 - 50%;
- over 65 years old: 37 - 51%.
Women:
- from 12 to 15 years: 34 - 44%;
- from 15 to 18 years: 34 - 44%;
- from 18 to 45 years old: 38 - 47%;
- from 45 to 65 years: 35 - 47%;
- over 65 years old: 35 - 47%.
Children:
- up to 2 weeks: 41 - 65%;
- from 2 to 4.3 weeks: 33 - 55%;
- from 4.3 to 8.6 weeks: 28 - 42%;
- from 8.6 weeks to 4 months: 32 - 44%;
- from 4 to 6 months: 31 - 41%;
- from 6 to 9 months: 32 - 40%;
- from 9 to 12 months: 33 - 41%;
- from 1 year to 3 years: 32 - 40%;
- from 3 to 6 years: 32 - 42%;
- from 6 to 9 years: 33 - 41%;
- from 9 to 12 years: 34 - 43%.
A hematocrit deviation from the norm may indicate:
when decreasing by:
- pregnancy;
- anemia;
- children's age;
- hypoproteinemia;
- overhydration.
when increasing by:
- true polycythemia;
- hypoxia;
- kidney hydronephrosis;
- kidney neoplasm;
- polycystic kidney disease;
- peritonitis;
- burn disease;
- leukemia;
- dehydration.
Blood color index (BC)
Normal blood color index:
Men, women and children:
- all ages: 0.9 - 1.1.
A deviation of the blood color indicator from the norm may indicate:
when decreasing by:
- anemia;
- purulent infections;
- cirrhosis of the liver;
- tuberculosis;
- Iron-deficiency anemia;
- iron-saturated hypochromia;
- malignant neoplasms;
- thalassemia;
- microcytosis.
when increasing by:
- lack of vitamin B12;
- lack of folic acid;
- dysbacteriosis;
- chronic pancreatitis;
- stomach diseases;
- diseases of the small intestine;
- cirrhosis of the liver;
- long-term treatment with glucose-lowering drugs;
- long-term treatment with anti-tuberculosis drugs;
- poor nutrition.
When to take it
A general clinical blood test must be taken:
- As prescribed by a doctor;
- As a preventative measure to assess general health;
- As part of routine medical examinations and examinations.
Thrombocytopenia redistribution
If we explain this mechanism very simply, it looks like this: due to some reasons, the patient’s spleen enlarges. And if under normal conditions it stores up to 30% of platelets, then in an enlarged state it retains up to 90% of these cells. At the same time, the system does not see that there are not enough platelets and does not trigger a compensatory mechanism.
The mechanism is also based on various causes: cirrhosis of the liver, some infections such as tuberculosis, autoimmune diseases (systemic lupus erythematosus), tumors of the circulatory system, alcoholism.
What to do in case of bleeding
If you start bleeding at home, take the following measures:
- Apply direct pressure to the bleeding area. If you have a nosebleed, pinch the bridge of your nose and apply ice to it.
- After applying pressure to the bleeding area, call your Memorial Sloan Kettering (MSK) doctor. If you cannot reach your doctor and are unable to stop the bleeding, go to your nearest emergency room.
When should you call your doctor?
Call your doctor right away if you have any of the following:
- black stools, blood in the stool, or bleeding from the rectum;
- blood in urine;
- persistent headache;
- blurred vision;
- dizziness;
- any persistent bleeding, including coughing up blood, vomiting blood, or bleeding from the nose.
to come back to the beginning
Thrombocytopenia dilution
This condition is usually observed in people who receive a large number of transfusions of various liquids: for example, plasma, plasma substitutes, etc. As a result, the level of platelets decreases due to the banal dilution of the blood.
Considering the huge number of reasons that can cause immune thrombocytopenia (and we have not named all the options), a patient with its symptoms should immediately consult a doctor who will find the essence of the problem and prescribe effective treatment.
Drugs that affect platelet levels
Long-term use of these drugs may change platelet levels:
- aspirin
- pain relievers such as ibuprofen and naproxen
- antihistamines
- asthma medicine
- sildenafil (Viagra)
- drugs used to prevent blood clots, such as clopidogrel
- antibiotics
- antidepressants and antipsychotic drugs
- Cholesterol-lowering drugs (statins)
- calcium channel blockers (verapamil).
Diagnostics
Since there are so many reasons, it is not possible to name diagnostic measures in detail - everything will depend on the specific situation. But we can highlight the main components of diagnosis:
- General blood analysis.
- Checking bleeding time (Duke test).
- Determining the time it takes for blood to clot.
- Red bone marrow puncture. The method allows you to identify quantitative and qualitative changes in cells.
- Determination of antibodies in blood.
- Research for genetic diseases.
- Ultrasound of internal organs. Most often, the liver and spleen are studied immediately, but this list can be very large.
- MRI. Used to study internal organs and blood vessels.
Diagnosis of the disease begins with a visit to a general practitioner, who, based on a survey, initial examinations and tests, prescribes visits to other specialists.
Treatment and severity
Treatment of thrombocytopenia most often comes down to identifying the primary disease and its treatment, as well as eliminating various unpleasant symptoms. In the process, it is also important to take into account that the severity of thrombocytopenia varies:
Mild degree. It assumes that the platelet concentration is from 50 to 150 thousand units per microliter. The condition of the capillaries is usually normal, bleeding does not develop. Usually, treatment is not necessary at this stage - doctors recommend waiting and monitoring the development of the patient’s condition.
Average degree. In this case, the concentration is 20-50 thousand platelet units per microliter. Under this condition, bleeding gums and nosebleeds are observed. If injuries and bruises occur, serious hemorrhages form in the skin. At this stage, drug therapy may be prescribed.
Severe degree. The platelet concentration is below 20 thousand, hemorrhages are spontaneous and severe. At the same time, the patient himself may feel quite comfortable, does not complain of feeling unwell, but tests show that he needs help.
Since the treatment of thrombocytopenia requires the most thorough and detailed diagnosis, it is important to choose a modern clinic that will help you. JSC "Medicine" in Moscow is just the place where you can get qualified help from the best specialists. The clinic has everything necessary for both examination and treatment of each patient.
Prognosis and prevention
Thrombocytopenia is a dangerous disease that poses a huge threat to the life and health of the patient. Anemia often develops, and vision loss can occur due to hemorrhages in the retina. Advanced forms can provoke hemorrhages in the internal organs and in the brain. In most cases this leads to death.
Thrombocytopenia has no specific prevention. Experts give the following recommendations:
- Take a general blood test every year and undergo a general medical examination;
- Eat properly and nutritiously: eat as much meat and fresh vegetables as possible;
- Play sports and lead an active lifestyle;
- Avoid self-medication: taking aspirin and steroid drugs should be under the strict supervision of a doctor;
- Try to avoid any procedures where there is a risk of cutting (shaving, manicure);
- Treat any infectious processes in a timely manner;
- Take precautions when working with chemicals;
- Give up bad habits: drinking alcohol slows down platelet production.
Thrombocytopenia is a disease that requires constant medical supervision. If you suspect you have it or know about the pathology and want to get rid of it, contact the Medscan medical center. Experienced doctors will perform the necessary diagnostics and develop an individual treatment plan.