February 28, 2020
According to the World Health Organization, hemorrhoids in various forms occur in almost 70% of the world's population
According to the World Health Organization, hemorrhoids in various forms occur in almost 70% of the world's population. This includes anyone who has ever experienced symptoms of this disease. Unfortunately, many people are embarrassed to see a doctor and self-medicate, because they believe that it is not customary to talk about such problems.
What are hemorrhoids?
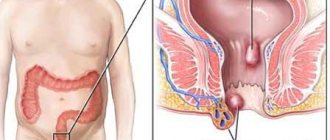
The rectum is the final point of the human digestive system, and therefore plays a very important role. It is surrounded by a double - external and internal, hemorrhoidal plexus of veins, which ensures a hermetic closure of the anus.
If the blood flows in too much or flows out too slowly, blood stagnation forms in the veins. As a result, the vessels swell, forming hemorrhoids (they are also often called lumps). This causes pain, a sensation of a foreign object in the anus.
Under the influence of constant pressure from large accumulations of blood, the walls of the veins become thinner and collapse. Bleeding occurs, particles of feces and other contaminants get inside the vessels, which leads to the formation of a focus of inflammation. As a result, the pain becomes simply unbearable, the person can neither sit nor lie down, and is afraid to go to the toilet.
Hepatrombin
Includes sodium heparin, which has an antithrombotic effect and the ability to relieve swelling and pain. The regenerative properties of the drug are ensured thanks to allontoin, a component that stimulates tissue healing and increases cellular metabolism. Prednisolone acetate allows you to treat inflammation, has an antiallergic effect, and reduces the release of fluid during inflammation (exudate).
Apply Hepatrombin to previously cleansed skin in a thin layer with light massaging movements. The course of therapy is from 7 to 10 days. It is prohibited to use the drug in patients who are allergic to the components of the product, in case of bleeding or during infection of wounds. The ointment is contraindicated for children under 5 years of age.
Symptoms of hemorrhoids
The disease progresses gradually over several years. The key to successful treatment is contacting a proctologist as soon as you notice the first symptoms of hemorrhoids.
All stages of the disease are characterized by the following symptoms:
- discomfort in the anus;
- pain during bowel movements;
- anal bleeding;
- traces of bright scarlet blood on linen, toilet paper, toilet;
- mucous or watery discharge;
- the formation of hemorrhoidal cones, their gradual increase in size.
In the initial form of the disease, there is a slight enlargement of the veins, but the person usually does not notice it. The only thing that indicates hemorrhoids is traces of bright scarlet blood on toilet paper after visiting the toilet. This is already a serious reason to consult a doctor, since bleeding may be a sign of a malignant tumor in the intestines.
When hemorrhoids enter the second stage, a person from time to time feels pain during bowel movements, itching, burning in the anus, and it seems to him that there is a foreign object inside. Hemorrhoidal cones sometimes fall out, but are easily adjusted by the patient on their own.
In the third stage, the symptoms described above intensify. Venous lumps increase significantly, narrowing the lumen of the anus and making defecation difficult. When visiting the toilet, a person experiences severe pain and bleeding often begins.
As the disease progresses to the fourth stage, the hemorrhoids enlarge so much that they cannot be moved inward by hand. The pain is very severe, each bowel movement is accompanied by bleeding. Blood clots – thrombi – form in the veins.
Hemorrhoids develop in two forms - external and internal. In the first case, the lumps are located close to the anus, so they often rupture and bleed during bowel movements. The pain is sharp and severe. In the second case, hemorrhoids can occur without pronounced symptoms, since the venous nodes are located inside the rectum, the mucous membrane of which is insensitive.
Troxevasin
Troxevasin ointment relieves the symptoms of hemorrhoids. In addition, it is a local anesthetic, astringent and anti-inflammatory agent. The drug combines troxerutin and magnesium stearate and is used externally:
- to relieve burning, itching around the anus;
- with inflammation of hemorrhoids;
- anal thrombophlebitis;
- inflammation of the rectum.
A local drug as an anti-inflammatory, decongestant. Troxerutin has a protective effect on veins, reduces the permeability of capillary walls, reduces swelling and exudation.
The gel should not be used if you have an individual intolerance to active substances or fillers, or an allergy to troxerutin. Like all medicines, Troxevasin ointment can cause side effects, such as hypersensitivity reactions and local skin irritation. Skin reactions may occur - rash, redness. However, the expected benefits are greater than the harm associated with the occurrence of undesirable effects.
Information on how to use the drug is in the instructions. The ointment is applied with uniform and gentle massage movements in a thin layer (approximately 2.5 g or half a teaspoon) twice a day (morning and evening) until completely absorbed. It is advisable to reapply to the affected area of skin after defecation.
Etiology of hemorrhoids
Varicose hemorrhoidal plexus occurs in men and women at any age. The causes of hemorrhoids are varied.
- Hereditary weakness of the walls of blood vessels, disruption of intestinal innervation.
- Lifting weights, excessive physical activity, as a result of which blood flows intensely to the rectal area.
- Prolonged standing or sedentary work, sedentary lifestyle
- lead to a slowdown in blood flow.
- Chronic constipation and diarrhea - feces irritate the mucous membrane and put too much pressure on the blood vessels.
- The habit of pushing hard during bowel movements leads to increased blood pressure on the walls of the veins.
- Poor nutrition, abuse of fatty spicy foods, alcoholic beverages, stress - negatively affect the regularity of bowel movements.
- Inflammatory and tumor processes in the liver and intestines.
- Smoking - under the influence of nicotine, the lumen of blood vessels narrows, and their walls become thin and fragile.
- Passion for anal sex and anal sex toys.
Hemorrhoids in women often occur after pregnancy (especially if it was multiple) or long, difficult labor, since pushing and the fetus create strong pressure on the blood vessels.
Proctosan
The ointment is based on bismuth subgallate and titanium dioxide. Proctosan promotes the healing of cracks, has a local astringent effect and dries out weeping in the anal area. The analgesic function is assigned to lidocaine, and bufexamak relieves inflammation. The ointment is indicated for use for hemorrhoids of any location; for ease of administration, an applicator is provided. The cost of the ointment is 250–300 rubles.
Prevention
The best measures to prevent the development and exacerbation of hemorrhoids, according to proctologists, are proper nutrition, improving bowel function, physical therapy, and careful hygiene.
In order for stool to be regular and have optimal consistency, it is necessary to monitor your diet.
- Consume fermented milk products.
- Eat raw vegetables and fruits rich in fiber.
- Eat small meals 5-6 times a day.
- Don't neglect oatmeal and bran bread.
- Take vitamins A, B, C, E, calcium, magnesium.
- Drink enough water, observing the daily norm of 1.5-2 liters.
- Avoid spicy, fried, fatty, smoked, alcohol.
Take laxatives only when absolutely necessary. Use teas and drinks with a laxative effect with caution, otherwise the intestines will literally “forget how” to work.
To strengthen the walls of blood vessels, take a course of phlebotonic drugs twice a year.
Therapeutic exercise and massage are also very useful because they help improve blood circulation and prevent congestion. If you find yourself in the same position for long periods of time, take regular small breaks to walk around or do at least a few squats. There are also special exercises for the anal sphincter and improving bowel function, but during an exacerbation they should not be done.
It is extremely important to carefully observe hygiene: wash your face every day, change your underwear, clean the anus with a damp cloth (without alcohol or fragrances) after each bowel movement.
What is this anal fissure? How to deal with it? How is it dangerous?
To better understand the essence of the disease and how to treat it, we will take a short excursion into the anatomy of this area.
If we mentally examine the anus (anus) from the outside, we will see folds of skin radially converging towards the center. Nothing else! Anything else you might find shouldn't be there.
The anus is compressed by a muscle called the sphincter. Then the anal canal goes about 2-2.5 centimeters deep, covered with almost the same skin as the surface of the body. Only this skin is thinner and without hairs. It's called anoderm. The anal canal is one of the most sensitive places in our body.
Then the anal papillae are located deeper - small, papilloma-like formations. Their size ranges from 1-2 to 5-8 millimeters. And immediately behind them is the internal hemorrhoidal venous plexus, from which internal hemorrhoids are formed.
So, an anal fissure is a rupture of the skin (anoderma) inside the anal canal at a depth of 2-2.5 centimeters.
The sizes of anal fissures vary - from 5-6 millimeters to 2 centimeters. Of course, the larger the crack, the more it bothers its owner.
However, the “cute” thing about fissures is that small, sharp (i.e., fresh) anal fissures often don’t hurt. The pain appears after several weeks, or even months. During this time, the crack becomes chronic and the patient cannot cope with it on his own.
What is the cause of anal fissures? The most common is dense feces. Not even constipation! A small crack that causes slight discomfort after stool is the most typical onset of the disease. Unpleasant sensations quickly pass without drawing attention to themselves. But the crack remains! At this time, treatment is most relevant and effective. But who is being treated at this time?
How to treat?
The main principle of treating anal fissures is to achieve soft, non-traumatic stools. Often this factor alone is enough for the crack to heal. Various drugs that promote accelerated wound healing are very appropriate here.
“Why don’t you give ready-made recipes, doctor? You beat around the bush,” you say.
Yes, because, my dear patients, I am a categorical opponent of self-medication! By diagnosing yourself and prescribing treatment, you can reach a sad ending! At the same time, almost any disease detected at the beginning of its development is often treated quite simply and thoroughly.
As an example from life, I can tell you about an incident in a pharmacy. And you yourself, most likely, have encountered similar situations, and maybe participated in them.
I stood in a small line at the pharmacy. In front of me, a guy, about 25 years old, was literally extorting an ointment for “sores” from a male pharmacist. To the pharmacist’s credit, he resisted quite a bit, not wanting to sell the guy anything. I sent this patient to a dermatologist, citing the fact that sores can be very different. Of course, after all, a “sore” is a mosquito bite, an allergy, and syphilis - it also manifests itself as a rash! What kind of ointment is this?
Why am I writing this? And just so you know, there are different “sores”, including in the anus. Often they present with exactly the same symptoms, but are treated completely differently!
Well, have you taken a break from medicine? Now let's go back to the crack. To the form that is most often encountered at a proctologist’s appointment – chronic anal fissure. Unfortunately, untreated acute anal fissure eventually becomes chronic. And this time can vary from 1-2 to 3-4 months or more.
What are the features of chronic anal fissure?
- First of all, persistent pain that persists after stool from several minutes to several hours. This pain can be very severe and difficult to treat. It mostly goes away on its own over time until the next bowel movement, when it resumes again.
- The next difference is that the sphincter (the muscle that compresses the anus) contracts strongly - it goes into spasms. As a result of the spasm, the pain intensifies, conservative treatment becomes almost hopeless. Time has passed.
- Another very important feature of chronic cracks is the formation of scars along the edges (the body tries to heal the crack). These scars are another obstacle to treatment. With massive scars, the crack does not heal on its own; they must be removed.
- And finally, another feature of chronic anal fissure is the formation of sentinel tubercles (skin outgrowths similar to papillae). They come in different sizes - from a few millimeters to 1-2 centimeters and are located at the inner and outer edges of the anal fissure.
All these factors, individually or all together, make up the chronic anal fissure complex. Such a crack almost never heals with conservative (medicinal) treatment, even very carefully selected ones.
Imagine, the crack is only 1–2 centimeters, such a small sore, but how many important features it has!
Drug and minimally invasive treatment
Treatment of hemorrhoids at the initial stage can be carried out at home, since no special measures are required yet. The doctor usually prescribes the following:
- a course of vascular-strengthening drugs;
- suppositories for hemorrhoids to relieve pain, itching and other unpleasant sensations, as well as to fight inflammation and reduce lumps, heal, stop bleeding;
- therapeutic diet and special physical training after the exacerbation is relieved;
- To relieve pain and itching, it is recommended to use cold compresses, ice packs, warm chamomile baths,
During the second and third stages, when conservative methods are ineffective, minimally invasive procedures are prescribed such as:
- Sclerotherapy - substances are injected into the node that seem to glue its walls together. As a result, the tissues stop receiving nutrition and die.
- Infrared photocoagulation, electrocoagulation - the essence of the method is that the leg of the node is cauterized, and its tissues are deprived of nutrition, stick together and die.
- Ligation with latex rings is used for internal hemorrhoids of stages 1-3. Using an anoscope, a ring is placed on the leg of the node, which compresses the small vessels feeding the node. After about two weeks, the dead node is brought out along with the ligature.
- Cryotherapy is a short-term exposure of the node to liquid nitrogen. The goal is the same - to stop the blood supply to the tissues of the node. After that it disappears on its own.
The listed remedies for hemorrhoids are effective for small bumps, but they cannot be used for thrombosis, anal fissures, acute inflammation, and injuries.
How to choose the right ointment?
To treat hemorrhoids, the following therapeutic regimens are used depending on the type and severity of the disease:
- To relieve pain, the following pain-relieving ointments for hemorrhoids, containing lidocaine and anesthesin, will be effective: Procto-Glivenol, Relief Advance, Proctazan, Emla, Irobin and others;
- You can overcome the relatively mild initial degree of hemorrhoids with the help of heparin ointments, as well as rectal suppositories containing benzocaine and heparin, for example, Nigepan;
- If the inflammatory process from hemorrhoids has spread to nearby tissues, antimicrobial and antibacterial agents are prescribed, such as Vishnevsky Ointment, Levomikol, Ichthyol (ichthyol ointment), Mafenide acetate;
- When the disease progresses rapidly, doctors typically prescribe nonsteroidal anti-inflammatory drugs (NSAIDs for short), such as Diclofenac, Piroxecam, and Ibuprofen;
- For rectal bleeding, combined medications (hemostatics) are used, which contain both anti-inflammatory and vasoconstrictor components, as well as anesthetic and venotonic substances, for example, Adroxon in the form of a solution, as well as Procto-Glivenol and Relief.
Below we will move on to a more detailed consideration of inexpensive and effective ointments for hemorrhoids.
4 Aurobin
Aurobin
An ideal remedy for the treatment of advanced hemorrhoids. If the patient does not start treatment in the early stages of the disease, then the doctor usually prescribes this very expensive drug. The ointment is considered by people with the third stage of the disease. However, it may be suitable even when the first symptoms of the disease appear, however, it will not be as effective, and rather even unnecessary. The product is used to treat external hemorrhoids. Panthenol in the composition will promote rapid healing of mucosal cracks, and lidocaine will relieve pain. For the exact dosage and number of daily applications, the manufacturer recommends consulting a proctologist.
Reviews after using the medicine are mostly positive. If the drug is not suitable for the patient, it is solely due to individual intolerance to the components. In some cases, it results in the appearance of even more cracks. Therefore, you cannot “prescribe” Aurobin ointment for yourself.
Terms of use
There are several rules for applying ointment for external hemorrhoids. To achieve maximum effect, you should adhere to the following recommendations:
- before applying the cream, you should perform hygiene procedures (take a bath or shower);
- When applying the product, do not rub it in, as this may damage the hemorrhoids. The smear should be rubbed in with gentle, slow movements, the nails should be cut short;
- After application, you should lie down for a while, this will allow the ointment to be well absorbed;
- if it is necessary to use the drug in the form of a compress, the product is applied to a sterile bandage or bandage and secured for 15 - 20 minutes;
- There is no need to wash off the ointment, except when indicated in the instructions.
Following simple rules will help prevent unwanted consequences and enhance the effect of drugs.
Other means
Microlax, which is available in a solution for rectal administration using microenemas, will help cure hemorrhoids that are bleeding.
This drug is a combination drug that has a laxative effect. The components included in the medicine help soften stool during constipation, which often causes bleeding.
In addition, Microlax affects the receptors of the intestinal mucosa, as a result of which peristalsis is stimulated. Thanks to this action, bowel movements are improved.
Thus, there is a large selection of pharmaceutical agents for the treatment of internal or external bleeding due to hemorrhoids. They are available in the form of tablets, injection solutions, microenemas, ointments, creams and rectal suppositories.
However, it is important to remember that some of them have adverse reactions or may be contraindicated in various conditions. Therefore, it is necessary that such drugs be prescribed by a qualified specialist.