HomeChildren's clinicCardiologyCongenital heart disease
Congenital heart defect
- a disease of the heart valves, in which the organ begins to malfunction. As a result of a congenital change in the structure of the valve apparatus, cardiac septa, walls, or large vessels extending from the heart, a disturbance in the blood flow of the heart occurs. The disease may progress. In some cases, death is possible.
Congenital heart defects occur with a frequency of 6-8 cases per thousand births, which is 30% of all developmental defects. They rank first in mortality of newborns and children of the first year of life. After the first year of life, mortality decreases sharply, and no more than 5% of children die between the ages of 1 and 15 years.
The earlier a congenital heart defect is detected, the greater the hope for its timely treatment.
General information
Acquired defects can manifest themselves in different forms. By origin:
- due to rheumatism, which is a general inflammatory disease of connective tissue that affects the heart; Source: A.N. Kalyagin Features of management of patients with rheumatic heart defects and chronic heart failure // Modern Rheumatology, 2009, No. 3, pp. 24-29
- against the background of syphilis;
- due to an inflammatory process on the inner lining of the heart (endocarditis);
- and due to other systemic diseases leading to damage to the heart muscle or complications to it.
According to the degree of defect, the acquired defect can be:
- local (when the defect is only in 1 valve);
- combined (more than 1 valve is affected);
- combined (both stenosis and insufficiency are observed in one valve).
The defect may be a stenosis due to inflammation, which led to the formation of scars, prolapse (eversion of the valves into the heart cavity), or failure (valve valves do not close completely). In this case, different valves may be defective (aortic, tricuspid, mitral, located on the trunk of the pulmonary artery).
An acquired defect can be expressed in different ways; it has three degrees:
- mild (minor effect on blood circulation);
- moderate;
- heavy.
This group of pathologies entails a number of complications:
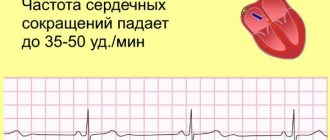
- heart failure;
- heart rhythm disturbances;
- blood clots
If left untreated or not detected early, heart disease can lead to disability and even death.
Patent ductus arteriosus
It is a vessel connecting the aorta (a large vessel that arises from the heart and carries arterial blood) and the pulmonary artery (a vessel that arises from the right ventricle and carries venous blood to the lungs).
Normally, a patent ductus arteriosus exists in utero and should close within the first two weeks of life. If this does not happen, they say there is a heart defect. The presence or absence of external manifestations (shortness of breath, tachycardia, etc.) depends on the size of the defect and its shape. External manifestations noticeable to the mother may not be present in a one-year-old baby, even with large ducts (6-7 mm).
Respiratory and heart rates are normal in children
| Age | Number of breathing movements per minute | Pulse per minute |
| Newborns | 40-60 | 140-160 |
| Infancy (up to 1 year) | 30-40 | 100-120 |
| Preschool age (from 1 year to 6 years) | 20-25 | 80-120 |
Patent ductus arteriosus has sound symptoms, and the doctor, as a rule, can easily listen to a heart murmur. The degree of its intensity depends on the diameter of the duct (the larger the duct, the louder the noise), as well as on the age of the child. In the first days of life, even large ducts are difficult to hear, since during this period the pressure in the pulmonary artery is normally high in children and, therefore, there is no large discharge of blood from the aorta into the pulmonary artery (which determines the noise), since the difference in blood pressure between vessels are small. Subsequently, the pressure in the pulmonary artery decreases and becomes 4-5 times less than in the aorta, the discharge of blood increases, and the noise intensifies. Consequently, doctors in the maternity hospital may not hear the noise; it will appear later.
So, as a result of the functioning of the patent ductus arteriosus, more blood enters the vessels of the lungs than normal; due to the increased load, over time, their walls irreversibly change, become less pliable, more dense, their lumen narrows, which leads to the formation of pulmonary hypertension (a condition when which increases the pressure in the blood vessels of the lungs). In the initial stages of this disease, when changes in the blood vessels of the lungs are still reversible, you can help the patient by performing surgery. People with the last stages of pulmonary hypertension have a short life expectancy and poor quality of life (shortness of breath, increased fatigue, severe limitation of physical activity, frequent inflammatory bronchopulmonary diseases, fainting, etc.). Pulmonary hypertension develops only with large ducts (more than 4 mm), and its irreversible stages usually occur in adolescence. With a small size of the duct, pulmonary hypertension does not form, but there is a risk of bacterial endocarditis - mainly due to the fact that a stream of blood under high pressure “beats” into the wall of the pulmonary artery, which changes over time under this influence and is more susceptible to inflammation than healthy tissue. Bacterial endocarditis is a special type of blood infection that affects the endocardium (the inner layer of the heart and blood vessels) and valves. Prevention of this disease consists of combating chronic foci of infection, which include: carious teeth, chronic tonsillitis (inflammation of the tonsils), chronic adenoiditis (inflammation of the nasopharyngeal tonsil), inflammatory kidney diseases, furunculosis, etc. Even with such interventions as, for example, tooth extraction, it is necessary to “cover” with antibiotics (these drugs are prescribed by the doctor).
In the first year of life, a decrease in large ducts and spontaneous closure of small ducts is possible. When it comes to surgery, parents are faced with a choice. Surgery can be of two types. In one case, the duct is ligated by opening the chest using artificial ventilation (that is, the machine “breathes” for the child). In the second case, the duct is closed endovascularly. What does it mean? A conductor is inserted through the femoral vessel into the open ductus arteriosus, at the end of which there is a closing device, and it is fixed in the duct. For small ducts (up to 3 mm), spirals are usually used, for large ducts - occluders (they resemble a mushroom or a coil in shape, depending on the modification). This operation is usually carried out without artificial ventilation, children are discharged home 2-3 days after the operation, there is not even a stitch left. And in the first case, discharge is usually made on the 6-8th day and a suture remains on the posterolateral surface of the back. With all the visible advantages, endovascular intervention also has disadvantages: it is usually not performed on children with very large ducts (more than 7 mm), this operation is paid for parents, since, unlike the first, the Ministry of Health does not pay for it, moreover, as and after any intervention there may be complications, primarily related to the fact that a device that is quite large in diameter needs to be passed through small children’s vessels. The most common of these is thrombosis (formation of a blood clot) in the femoral artery.
Diagnosis of acquired defect
The most important thing in diagnosis is taking an anamnesis. The doctor analyzes past and existing diseases, their severity, characteristics of the course, and the effectiveness of the therapy. The child’s complaints are examined with close attention, and the specialist asks about injuries in the chest area. The child’s parents are always asked about heart disease or pathologies in someone in the family, about cases of heart defects.
The child is examined. Using a stethoscope, murmurs and pulmonary wheezing are detected. The doctor measures blood pressure and taps to determine the boundaries of the heart and, accordingly, its size.
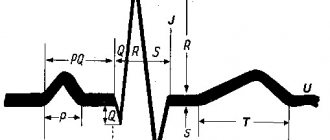
Knowing the type of murmur can help preliminarily determine the type of heart defect.
Based on a comprehensive history and examination, the patient may be prescribed various laboratory and instrumental tests.
- Determination of liver size.
- General urine analysis.
- Clinical blood test.
- Blood chemistry.
- FKG.
- ECG.
- ECHO-KG.
- .
- X-ray with contrast.
- MRI. Source: R.K. Georgikia, G.I. Kharitonov Modern aspects of diagnosis and treatment of acquired heart defects // Kazan branch of Apteka-Holding CJSC, 2003, No. 2, pp. 25-26
A year later - a healthy toddler
When surgery for a congenital defect is performed on a still healthy heart muscle, after timely and high-quality treatment, the patient turns from a disabled person into an absolutely healthy person. Complete rehabilitation takes only about a year. Therefore, if you perform surgery on your baby, in a year you will have a healthy, ruddy little one stomping around the house.
Many defects that were previously operated on with large incisions and artificial circulation are today corrected using a much less traumatic endovascular method (using catheters). The rehabilitation period after such an operation is at least half as long. New methods of anesthesia make it possible to awaken the patient and “turn on” his own lungs immediately after surgery. All this helps to better tolerate surgical treatment.
Treatment methodology
After the appearance of an acquired heart defect, the body compensates for the impaired circulatory function. That is, a sick child does not feel discomfort and does not feel the need for treatment.
Drug therapy is prescribed to stabilize the heart rhythm, reducing the risk of heart failure, relapses and complications of the disease that caused the defect.
The main method of treatment is surgery. During it, the heart valve can undergo changes, that is, the defect is corrected and proper function is restored. Or the damaged valve is replaced with an artificial one (prosthetics). Source: E.I. Kinoshenko Emergency conditions for acquired heart defects // Emergency Medicine, 2013, No. 4(51), pp. 9-24
Heart defect in a child - what is it?
This term refers to a group of diseases associated with pathological changes in the structure of valve tissue, interventricular septa of the heart, and adjacent vessels. Such abnormal changes lead to deterioration of blood circulation, and as a consequence of this, to insufficient oxygen supply to the internal organs and to congestion in the respiratory system.
In mild cases, the defect may be asymptomatic or progress over time. In severe cases, the baby may require surgery immediately after birth.
Most often, a congenital (occurs in the fetus) defect is diagnosed, determined during an ultrasound scan for pregnant women, after birth or in the first year of a child’s life.
Disease prevention
The most important measure to prevent acquired heart disease is careful prevention of the diseases that lead to it. It is necessary to diagnose and treat sore throat in time, to prevent rheumatism and its relapses.
A correct regimen of physical activity and nutrition is necessary. At the same time, the sport should not be difficult or involve competition. You should lead an active lifestyle and do not overload your child with mental work. Morning exercises should be included in the daily “rituals,” which parents can do together with their child, setting an example of the correct lifestyle. The most favorable sports are swimming, cycling and walking.
Advantages of SM-Clinic
- Our pediatricians and cardiologists are among the best in St. Petersburg.
- Diagnostics are carried out using modern equipment.
- There are no queues.
- The diagnosis is made in a short time, and the most effective treatment in a particular case is prescribed.
Make an appointment at the first sign of acquired heart disease in your child. SM-Clinic will do everything to ensure that he quickly and permanently returns to a healthy life.
Sources:
- A.N. Kalyagin. Features of the management of patients with rheumatic heart disease and chronic heart failure // Modern Rheumatology, 2009, No. 3, pp. 24-29.
- R.K. Georgikia, G.I. Kharitonov. Modern aspects of diagnosis and treatment of acquired heart defects // Kazan branch of Apteka-Holding CJSC, 2003, No. 2, pp. 25-26.
- E.I. Kinoshenko. Emergency conditions for acquired heart defects // Emergency Medicine, 2013, No. 4(51), pp. 9-24.
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Ventricular septal defect
This is a communication between the ventricles (chambers of the heart), in which, unlike the atria, the pressure is high, and in the left ventricle it is 4-5 times higher than in the right. The presence or absence of clinical manifestations depends on the size of the defect and in what area of the interventricular septum it is located. This defect is characterized by a loud heart murmur. Pulmonary hypertension can develop quickly, starting in the second half of life. It should be noted that with the formation of pulmonary hypertension and increased pressure in the right side of the heart, the heart murmur begins to decrease, since the discharge through the defect becomes less. This is often interpreted by the doctor as a reduction in the size of the defect (its healing), and the child continues to be observed at the place of residence without being referred to a specialized institution. As pulmonary hypertension progresses to its irreversible stages, the pressure in the right ventricle becomes greater than in the left, and venous blood from the right parts of the heart (carrying blood to the lungs for oxygenation) begins to flow into the left (from which oxygen-rich blood is sent to all organs and tissues). The patient develops bluish skin (cyanosis), and physical activity decreases. In this condition, the patient can only be helped by a heart and lung transplant, which is not done for children in our country.
Advertising
On the other hand, ventricular septal defects are prone to spontaneous closure, which is associated with the growth characteristics of intracardiac structures in the baby, so they are usually not in a hurry to be eliminated surgically immediately after birth. In the presence of heart failure, the signs of which are determined by the doctor, drug therapy is prescribed to support the functioning of the heart and the dynamics of the development of the process are monitored, examining the baby every 2-3 months and conducting echocardiography. If the size of the defect decreases to 4-5 mm or less, then such defects, as a rule, are not operated on, since they do not affect health and do not cause pulmonary hypertension. If it comes to surgery, then ventricular septal defects are closed in the vast majority of cases using artificial circulation, cardiac arrest using a patch. However, over the age of 4-5 years, with a small size of the defect and its specific localization, endovascular closure is possible using an occluder passed through the vessels. It should be noted that it is better to be observed in a cardiovascular surgery center (the doctors there, including echocardiographers, which is very important, have more experience). If the size of the defect decreases to 4-5 mm or less, then such defects, as a rule, are not operated on, since they do not affect health and do not cause pulmonary hypertension.
Prices
| Name of service (price list incomplete) | Price |
| Appointment (examination, consultation) with a cardiologist, primary, therapeutic and diagnostic, outpatient | 1750 rub. |
| Prescription of treatment regimen (for up to 1 month) | 1800 rub. |
| Consultation (interpretation) with analyzes from third parties | 2250 rub. |
| Consultation with a candidate of medical sciences | 2500 rub. |
| Electrocardiography (ECG) | 1400 rub. |
| Echocardiography (ultrasound of the heart) | 3500 rub. |