When hemoglobin breaks down in sideroblast cells, hemosiderin is formed - a pigment containing iron molecules. It is deposited in the structures of the bone marrow, in the liver, in the spleen, in the sweat and salivary glands and in other organs. The main function of the pigment is the deposition and transfer of oxygen, as well as iron molecules, and participation in the transformation of biochemical complexes. With certain changes in the body, the synthesis of iron-containing compounds is activated.
Hemosiderosis (capillaritis, hemorrhagic pigmentary dermatosis) is a disease from the category of pigmentary dystrophies associated with metabolic disorders and excessive accumulation of hemosiderin in tissues and blood vessels. The skin and internal organs are affected. Deposits of hemoglobinogenic pigment can be widespread or local. Establishing the nature of the disease is difficult. Treatment is carried out by dermatologists, pulmonologists, hematologists, immunologists and other specialists.
About the reasons for the development of hemosiderosis
Skin hemosiderosis can be primary or secondary, developing due to injuries and skin infections.
The causes of primary skin capillaritis may be the following factors:
- vascular changes due to the presence of hypertension, varicose veins, etc.
- various endocrine disorders - the patient has diabetes mellitus and other pathologies.
Secondary hemosiderosis of the dermis can be caused by:
- scratching the skin, damage, injuries;
- skin diseases – dermatitis, neurodermatitis, etc.;
- pustular skin diseases.
Risk factors that can provoke the development of the disease include:
- frequent hypothermia;
- stress;
- excessive physical activity;
- taking diuretic, anti-inflammatory and antibacterial drugs.
Generalized hemosiderosis develops against the background of previous diseases. Most often, the main causes are systemic blood diseases, autoimmune diseases, severe intoxications and exposure to infectious agents. Increased deposition of hemosiderin may be due to:
- leukemia;
- sepsis, malaria and other infections;
- the presence of Rh conflict;
- liver damage;
- constant blood transfusions;
- taking large doses of sulfonamides, drugs containing quinine or lead.
Why iron-containing pigment accumulates in the lungs is not entirely clear. Often the reasons lie in genetic predisposition, in congenital anomalies of the pulmonary capillaries, in existing heart diseases.
Principles of treatment
To date, it is believed that not a single drug has a 100% evidence base for its effectiveness in treating hemosiderosis. Thus, the treatment of these diseases is a problem and a challenge for doctors. However, some hemosiderosis can resolve on its own and then unexpectedly recur.
Corticosteroids are effective in reducing inflammation and suppressing itching in some hemosideroses. Antihistamines inhibit endogenous histamine production and also reduce the feeling of itching in patients.
The administration of griseofulvin, cyclosporine A, vitamin C and bioflavonoids has certain benefits. There is evidence of the positive effect of PUVA therapy (psoralen (P) + ultraviolet A (UVA) = PUVA or PUVA) - irradiation of the skin with ultraviolet light A with preliminary intake of a photosensitizer (psoralen) for greater effectiveness of light exposure.
hardware techniques can be used aimed at selective destruction of the pigment. For local destruction of hemosiderin for aesthetic purposes, IPL therapy can be used: a method in which high-intensity pulsed light destroys the pigment, making it more accessible for evacuation during phagocytosis.
Questions from our users:
- skin hemosiderosis laser treatment
- hemosiderosis of the skin after injections
- hemosiderosis of the skin in adults
- local and general hemosiderosis causes
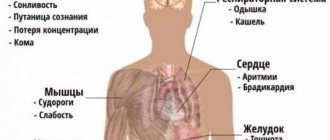
Characteristic symptoms
Clinical manifestations depend on where the hemoglobinogenic pigment accumulates.
Pulmonary hemosiderosis
Idiopathic (primary) pulmonary hemosiderosis is manifested by the following symptoms:
- moist cough;
- elevated temperature, fever;
- presence of shortness of breath and respiratory failure;
- cough with blood;
- chest pain, severe dizziness;
- pale skin;
- hypochromic anemia;
- skin cyanosis;
- enlarged spleen and liver;
- drop in blood pressure, heart rhythm disturbance.
Brown purpura of the lungs, usually found in children and young adults, is a serious disease. With a prolonged course of the disease, recurrent infarction-pneumonia and other pathologies very often develop.
At CELT you can consult a pulmonologist.
- Initial consultation – 3,500
- Repeated consultation – 2,300
Make an appointment
Skin hemosiderosis
The following symptoms are characteristic:
- the appearance of brown pigment spots in the lower extremities and other parts of the body;
- hemorrhagic rash on the skin of the hands, feet, forearms, etc.;
- slight itching in problem areas;
- formation of plaques, nodules and papules.
Chronic hemosiderosis of the dermis is usually diagnosed in men over 30 years of age. The disease occurs without damage to internal organs.
At CELT you can consult a dermatologist.
- Initial consultation – 3,500
- Repeated consultation – 2,300
Make an appointment
Purpurative pigmentary dermatosis of the liver is manifested by enlargement of the organ, its soreness, yellowness of the integument, and the presence of a pigmented rash on the hands, in the armpits, and on the face. If the kidneys are damaged, swelling in the legs, dyspepsia, changes in taste, lower back pain, etc. appear.
Pathogenesis
Macrophages, as well as histiocytes , epithelial cells , and endotheliocytes with the help of their sideroblasts are capable of synthesizing hemosiderin molecules. They are found in the spleen, liver, lymph nodes, bone marrow and other organs. The simplest example of local accumulation of pigment is a common hematoma .
Usually, the process of local hemosiderolysis is triggered by a massive hemorrhage or many diapedetic hemorrhages, where extravascular (extravascular) hemolysis occurs in the presence of oxygen molecules.
hemotoidin is formed , and hemosiderin is formed only in the periphery for about 2-3 days. Its presence in the tissue means that the hemorrhage is old.
Normally, the pigment accumulated in cells does not have a damaging effect on tissues or the structure and functioning of organs, but if hemosiderin accumulates against the background of sclerotic processes, this can lead to functional disorders and consequences. For example, the formation of a cyst in the brain: since hemosiderin is deposited between healthy tissues and blood clots at the site of hemorrhage, repeated hemorrhage leads to the formation of a cyst with brown edges.
The general excessive accumulation of hemosiderin in the body causes excess iron during intravascular (intravascular) hemolysis or it is associated with increased absorption of iron from consumed foods. In this case, siderophages do not have time to absorb hemosedirene and, as a result, fibers, intercellular substance and tissues leak iron and give the spleen, liver, bone marrow, and lymph nodes a brown color. Deposits of hemosiderin can be found in the epithelial cells of the sweat glands, salivary glands and kidneys. bilirubin accumulate . Due to increased bilirubin, patients may experience hemolytic jaundice .
Bone marrow hemosiderosis
A fairly common phenomenon is when pigment molecules do not damage parenchymal cells and there are no organ dysfunctions, but if an increased amount of iron has a damaging effect and causes atrophy of the parenchyma, sclerosis , which reduces and disrupts its functioning, then we are talking about a hereditary disease - hemochromatosis .
Diagnostics
A dermatologist examines the patient, examines the nature of the rash and the presence of characteristic signs. Laboratory tests are required - blood biochemistry with determination of iron levels, general urine tests, PCR tests. The content of sputum and urine is analyzed using a desferal test. To clarify the diagnosis, the affected segments are sent for a biopsy. Histological studies of the skin, bone marrow, lungs, lymphatic tissues, liver, and kidneys help detect pigment deposits. For diagnostic purposes, bronchoscopy with examination of lavage water can be performed, a chest x-ray, MRI, and computed tomography may be performed.
Classification
Hemosiderosis can be local - focal (with extravascular hemolysis) and general - generalized (hemolysis - intravascular). Local accumulation of hemosiderin can occur in lung tissue and epithelium.
General hemosiderosis is most often preceded by massive hemolysis , and it affects hepatocytes , macrophages of the spleen , bone marrow and other organs.
Pulmonary hemosiderosis
Chronic venous congestion in a closed vascular pathway of the pulmonary circulation as a result of heart failure leads to local hemosiderosis of the lungs ( brown induration of the lungs ). Prolonged venous stagnation and increased permeability of the vascular walls contribute to the release of red blood cells into the alveolar lumen, where they are captured by alveolocytes, in which hemosiderin is formed, thereby “swamping” the cavities of the alveoli. At the same time hypoxia , diapedesis hemosiderophages arise due to the collagen-synthetic activity of fibroblasts and the proliferation of connective tissues, and interstitial diffuse fibrosis and sclerotic small vessels of the lungs can also be detected.
In the etiopathogenesis of pulmonary hemosiderosis, both exogenous factors - dusting of the lungs with iron dust, and endogenous - secondary factors can play a role; development occurs against the background of heart defects.
The disease has exacerbations - for 3-5 days, as a result of which microcytic hypochromic anemia .
Idiopathic pulmonary hemosiderosis or Delen-Gellerstedt syndrome has an incompletely understood etiology and is usually accompanied by hemorrhages in the alveoli of a diffuse nature. By absorbing iron, macrophages are transformed into siderophages and can be found in the sputum of patients. Most often occurs in children 3-8 years old and is not caused by heart defects. Idiopathic hemosiderosis has not been fully studied, but in the etiopathogenesis a large role is assigned to the immunopathological stage of development, since the kidneys are also affected, causing the development of Goodpasture syndrome antibodies can be found in the bloodstream .
Hemosiderosis of the liver
Excessive deposition of hemosiderin in the liver is observed in general hemosiderosis, when pathological changes affect the reticuloendothelial system in the beams along the sinuses and hepatocytes directly in the parenchyma . With processes of a minor nature, timely therapy can lead to complete recovery, but with great severity and progression of sclerosis, pigmentary cirrhosis .
Hemosiderosis of the liver
Skin hemosiderosis
Skin hemosiderosis
Excessive hemosiderin deposition usually occurs in the form of post-traumatic hemosiderosis, pigmentary capillaritis, hemorrhagic pigmentary dermatoses and pigmented purpuric dermatoses. The cause most often is soft tissue injuries - bruises and injections with subsequent development of hematomas, in more rare cases - systemic disorders of iron metabolism.
Mechanical impacts cause ruptures in the capillary network; macrophages cannot always have time to utilize all the “subcutaneous” blood, so its breakdown product, hemosiderin, accumulates. As a result, fairly persistent local changes in color and pattern are formed on the skin, which can cause aesthetic discomfort (as in the photo of skin hemosiderosis).
Hemosiderosis of the cornea
Hemosiderin molecules can be deposited in corneal epithelial cells at the basal level and form so-called Fleischer rings . Their color is usually yellowish or dark brown and they may be torn. They can be detected using a slit lamp along with cobalt blue light.
Such iron deposits are observed in 50% of patients with keratoconus and other degenerative diseases of the cornea. Whereas the formation of the Hudson-Staley line (a layer of deposited iron in the thickness of the corneal epithelium) is typical for healthy people over 50 years of age. Moreover, they can fade away by the age of 70.
Gouty bump
With gout, foreign compounds periodically fall out into the small joints of the arms and legs, tendons, and periarticular tissues, which is accompanied by necrosis and inflammation, the development of connective tissue, which is very reminiscent of the picture of hemosiderosis . This leads to the formation of gouty bumps, which deform the joints.
Foreign body giant cells in a gouty lump
Gout bumps are deposits of urates (compounds with uric acid) in soft tissues. If you examine a microscopic specimen of a gouty lump, you can see areas of necrosis, amorphous masses and deposits of sodium urate crystals. The description also includes the identification of connective tissue, an inflammatory infiltrate with giant multinucleated cells resembling “foreign bodies”.
Therapeutic tactics of hemosiderosis
Treatment is prescribed by a dermatologist and depends on the clinical manifestations and severity of the disease.
Conservative therapy:
- Prescription of glucocorticosteroids. These are first-line drugs that suppress inflammation, restore physiological processes, stop autoimmune processes and stabilize cell walls. In 50% of cases, drugs cure hemosiderosis.
- Immunosuppressants in combination with plasmapheresis. Cytostatics and other immunosuppressants suppress the immune system, including at the cellular level, and prevent the formation of new antibodies. The blood is filtered using a special apparatus. Toxins, accumulated antibodies and immune complexes that increase vascular permeability are removed from tissues, vessels and cells.
- Vitamin complexes containing vitamin C, rutin, calcium, etc.
- Iron supplements in the presence of anemia and other complications.
- Hemostatic drugs.
- Medicines to eliminate symptoms of the disease. If necessary, bronchodilators, angioprotectors, anticoagulants, antiplatelet agents, etc. are prescribed.
- Corticosteroid ointments are prescribed locally.
- Inhalations with oxygen.
- Cryotherapy.
In severe cases, doctors perform a splenectomy, and patients have their spleen removed to achieve stable remission. They resort to blood transfusion, PUVA therapy, and prescribe drugs that help remove iron from the body.
Complications
If a patient with capillaritis does not receive proper treatment, dangerous complications develop that can lead to disability and death. Advanced forms of pulmonary hemosiderosis, when the pathological process affects the alveoli, are especially difficult to treat.
Possible complications:
- extensive pulmonary infarction;
- acute respiratory failure;
- multiple internal hemorrhages;
- constant overload of the heart and the formation of cor pulmonale;
- persistent increase in blood pressure;
- spontaneous pneumothorax.
Hemosiderosis of the skin has a favorable course. In advanced forms of the disease, cosmetic defects appear that require proper correction.
General information
Hemosiderosis is usually called a condition of tissues with a pathologically increased content of dark yellow, brownish pigment - hemosiderin , deposited in the thickness of the cytoplasm as amorphous grains that strongly refract light. Its molecule is iron hydroxide , formed during the breakdown of hemoglobin (an iron-containing oxygen-carrying protein). Then denaturation and deproteinization of ferritin , a complex protein complex that is the main iron depot in the body.
The greatest importance in the occurrence of hemosiderosis is attributed to increased breakdown of red blood cells , disruption of the process of utilization of hemosiderin in erythrocytopoiesis , increased absorption in the gastrointestinal tract, impaired metabolism of pigments containing iron, various diseases, for example, aceruloplasminemia , and the development of pathology may be associated with intake of excess doses of iron supplements (for example, Venofer or Likferr ).
What is hemosiderin?
Hemosiderin is a brown pigment whose main component is iron oxide.
It is formed in the biological process of fermentation (breakdown) of hemoglobin and subsequent synthesis in sideroblasts (nucleated cells).
Normally, the body of each person contains approximately 4-5 g of this iron-containing pigment.
Excessive accumulation of it can lead to structural changes inside the body.