Neutrophils - what kind of cells are they?
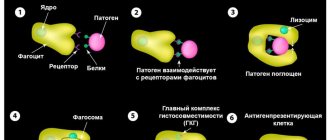
Neutrophils are a group of white blood cells that fight the spread of infection in the body. They are formed by bone marrow cells and are sent through the body tissues to the site of infection. Having detected foreign cells, neutrophils capture and engulf them. This process is called phagocytosis.
The lack of neutrophils has a scientific name - neutropenia. This is a condition in which blood cells break down too quickly, without having time to build a reliable defense. In some situations, we have to talk about disorders of the hematopoietic system, when the bone marrow does not produce enough protective cells or about the fact of a pronounced decrease in immunity.
To determine the number of neutrophils, two types of measurements are used:
- true;
- relative.
When determining the true number of cells, their content in the analyzed volume of blood is taken into account. When identifying a relative indicator, the total number of leukocytes is taken into account and the percentage that neutrophils make up of the total number is calculated.
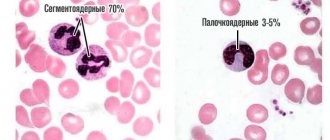
Neutrophils are very mobile blood cells; they have access to areas and tissues where the main leukocytes do not penetrate. All neutrophils, depending on their maturity, are divided into band and segmented. The second group is mature cells, their number increases significantly when an inflammatory process occurs. They are the main phagocytes filling the bloodstream, but when infection develops, they quickly migrate to the site of inflammation, overcoming the walls of blood vessels.
Functions and types of cells
Neutrophils are a type of leukocyte - white blood cells that are vital to the immune system. These cells are heterogeneous; in total there are 4 types of neutrophils, which differ in their narrow purpose:
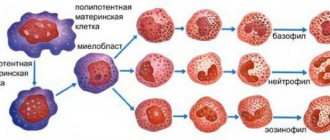
- myelocytes are preneutrophils, maximally immature cells without differentiation, which can eventually turn not only into a neutrophil, but into any blood element: from a platelet to an eosinophil;
- young neutrophils are an immature version of neutrophils, a conditional reserve of cells that begin to work in conditions of the body’s increased need for immune cells; in critical situations, a minimum number of such cells can be recorded in the bloodstream (no more than 1%);
- band neutrophils - make up no more than 5% of the total number of neutrophils, this is already a partially specialized cell of the immune system, it works in the bloodstream if the remaining neutrophils cannot cope with their functions;
- segmented neutrophils are the basis of neutrophil cells; up to 70% of the total number of structures constantly work in the bloodstream; they manifest themselves to the maximum during the infectious and inflammatory process in the body.
Thus, there are only two types of active, that is, capable of acting, neutrophils: segmented and band. They solve the main tasks that the body sets for neutrophils:
- lyse the cell membrane of the pathogen, killing viruses, bacteria, fungi, and other pathogenic microflora;
- enter into an antigen-antibody reaction with microbes, binding pathogenic flora, accelerating the relief of inflammation;
- absorb microbes and digest them (phagocytosis): one cell can destroy up to 30 “strangers”;
- inactivate viruses, reducing the rate of replication of pathogens, helping to stop inflammation of a viral nature.
How many neutrophils should there be?
The fact that there are not enough neutrophils is indicated by a blood test in which the content of phagocyte cells is below 1.6x10⁹. However, the normal options depend on the age of the patient. For example, children in the first year of life should have 30%-50% neutrophils in their blood relative to the total number of leukocytes, and by the age of seven their percentage increases and a figure of up to 55% is considered normal. At the same time, the lower threshold also increases - it starts from 35%. An adult can have from 45% neutrophils in relation to the total number of leukocytes, the upper limit of normal for this age category is 70%.
To make a diagnosis of neutropenia, the true value of the cell number is determined. Mild neutropenia is diagnosed when the level is from 1 to 1.5x10⁹ units per liter of blood. The degree is considered moderate when the content is from 0.5x10⁹, and severe neutropenia is observed when the level is below 0.5x10⁹, or the complete absence of phagocyte cells.
Neutropenia can be congenital or acquired. Blood cell levels may vary depending on your health. The lack of corpuscles can be a separate problem or manifest itself when a specific disease occurs. Congenital forms of neutrophil deficiency are inherited and may not clinically manifest themselves until the blood is taken for analysis for some other reason.
Interpretation of a general blood test
Below are the most basic indicators of the KBC, their functions in the body, and the reasons for deviations upward or downward.
Red blood cells
These are small elastic cells containing hemoglobin in their cytoplasm. Due to their elasticity, they easily pass through vessels of any caliber. They are produced in the bone marrow, the viability of one cell is about 3-4 months.
Red blood cells perform the following function: they carry oxygen from the lungs to all human tissues and organs, and on the way back from the tissues to the lungs they bring carbon dioxide. All this happens by adding gases to the hemoglobin of the red blood cell.
The norm of red blood cells when deciphering tests is on average from 3.8 to 5.0 1012/l
- An increase in red blood cells in a general blood test is possible with dehydration due to vomiting and diarrhea, diseases of the blood system (erythremia, Vaquez disease), cardiac and respiratory failure.
- their reduction can occur with blood loss, leukemia and lymphomas, congenital hematopoietic defects, hemolytic anemia, oncology, insufficient intake of protein, iron and vitamins.
It should be remembered that the norm of red blood cells, as well as other indicators, may differ in different laboratories. In which, moreover, errors are not excluded. Therefore, a borderline result does not always indicate a serious illness.
Hemoglobin
Hemoglobin is an iron-containing protein found in red blood cells. It is due to this that the function of gas exchange between the lung tissue and all cells of the body is performed. A deviation in hemoglobin levels from the norm can cause a person to feel unwell, weak, and easily fatigued. This is due to a lack of oxygen in organs, including the brain.
The normal hemoglobin content in a general blood test is on average 120-160 g/l, depending on the gender and age of the subject.
- An increase in hemoglobin can occur due to dehydration due to diabetes mellitus, vomiting and diarrhea, due to heart failure, overdose of diuretics, pulmonary failure, heart defects, diseases of the blood and urinary system.
- A decrease in hemoglobin in a general blood test is possible with anemia of various origins and other blood diseases, blood loss, insufficient intake of protein, vitamins, and iron
Leukocytes
These are white blood cells synthesized in the bone marrow. They perform the most important defense function in the body, aimed at foreign objects, infections, and foreign protein molecules. They are also able to dissolve damaged body tissue, which is one of the stages of inflammation. The viability of these cells varies from several hours to several years.
The norm of leukocytes in a general blood test corresponds to 4.0-9.0 109/l.
- An increase in leukocytes in the CBC is possible due to physiological errors (pregnancy, donating blood after meals, heavy physical activity, after vaccinations), inflammatory processes of a systemic or local nature, extensive injuries and burns, active autoimmune diseases, in the postoperative period, with oncology, leukemias and leukemias.
- If, when reading a blood test, leukocytes are reduced, the presence of viral infections, systemic autoimmune diseases, leukemia, radiation sickness, and hypovitaminosis is acceptable. Taking cytostatics and steroids may also affect this.
Color index
The color index (CI) is determined by a calculation method using a special formula. It shows the average concentration of hemoglobin protein (Hb) in one red blood cell.
Normally, the CPU is 0.8-1.0, without units of measurement.
- Its increase may indicate the presence of hyperchromic anemia (vitamin D deficiency).
- A decrease is possible in iron deficiency anemia, posthemorrhagic anemia, leukemia and lymphoma, and chronic organ diseases.
Hematocrit
This is an indicator reflecting the ratio of blood cells (leukocytes, erythrocytes, platelets) to the total blood volume. The analysis is carried out by centrifugation or using analyzers.
Normally, the hematocrit is on average 35-50%.
- An increase may indicate erythremia, respiratory failure, heart failure, dehydration due to diabetes mellitus and diabetes insipidus, diarrhea and vomiting.
- A decrease in hematocrit may be due to anemia, erythrocytopenia, renal failure, pregnancy (third trimester).
Reticulocytes
These are the precursors of red blood cells, their intermediate form. They perform the function of gas exchange, just like red blood cells, but with less efficiency. In a healthy person, reticulocytes, when deciphered, make up 0.2-1.2% of the total number of red blood cells.
- They may be increased during post-hemorrhagic restoration of hematopoiesis, when moving to a mountainous area or when treating anemia.
- Reticulocytes in the general blood test decrease with reticulocytopenia (slow hematopoiesis in the bone marrow, leading to anemia).
Platelets
These are small, flat blood cells that have no color. They perform several important functions - they participate in blood clotting, form platelet thrombus, regulate the tone of the vascular wall, and nourish capillaries.
In a general blood test, the normal platelet count is 180-320 109/l.
- An increase in platelets when deciphering the analysis is possible during splenectomy (removal of the spleen), exacerbation of chronic autoimmune diseases, anemia of various origins, inflammatory processes, in the postoperative period, the third trimester of pregnancy, in oncology, erythremia.
- Platelets in the CBC decrease in hemophilia, drug-induced thrombocytopenia, systemic lupus erythematosus, viral and bacterial infections, aplastic anemia, Evans syndrome, autoimmune thrombocytopenic purpura, and renal vein thrombosis.
ESR
Erythrocyte sedimentation rate (ESR) is an indicator calculated during a laboratory test. Under the influence of anticoagulants, the erythrocyte sedimentation time is calculated, which depends on the protein composition of the plasma.
This is a highly sensitive indicator; normally it averages from 1 to 15 mm per hour.
- It increases during physiological conditions (pregnancy, menstruation), during infectious diseases, malignant neoplasms, systemic autoimmune diseases, kidney diseases, in the postoperative period, during injuries and burns.
- Decreased in astheno-neurotic syndrome, recovery from infection, cachexia, long-term use of glucocorticoids, blood clotting disorders, high concentrations of glucose in the blood, traumatic brain injury, use of NSAIDs, immunosuppressants, antibiotics.
Neutrophils
This is the largest subtype of leukocytes, which, depending on the maturity of the cells, is divided into the following groups - young neutrophils, band neutrophils and segmented neutrophils.
They perform an antimicrobial function, are capable of phagocytosis, and participate in the inflammatory response.
The normal range of neutrophils in a blood test is band 1-6%, segmented 47-67%.
- An increase in neutrophils when decoding a blood test is possible under physiological conditions (sun and temperature exposure, stress, pain, etc.), previous infections, bone marrow diseases, oncology, taking certain medications, ketoacidosis, poisoning with poisons and alcohol, and parasitosis , allergies, hyperglycemia.
- They decrease in the state after chemotherapy, with HIV/AIDS, aplastic anemia, long-term infectious disease, exposure to radiation, deficiency of vitamin B12 and folic acid.
Lymphocytes
This is also a subtype of leukocytes, presented in the form of T lymphocytes, B lymphocytes, K and NK lymphocytes.
All of them participate in acquired immunity, synthesize antibodies, destroy not only foreign, but also their own pathological cells (oncological).
The norm of lymphocytes when deciphered in the CBC is 18-40%
- An increase in the general blood test can occur with viral infections (mononucleosis, viral hepatitis and others), toxoplamosis, blood diseases (chronic and acute lymphocytic leukemia, lymphoma, leukemia), with arsenic, lead poisoning, taking levodopa, narcotic painkillers.
- Lymphocytes decrease in tuberculosis, HIV, blood diseases (lymphogranulomatosis, aplastic anemia), end-stage renal failure, cancer in the terminal stage and during treatment with radiotherapy and chemotherapy, taking glucocorticoids.
Monocytes
This is a type of the largest leukocytes, also synthesized in the bone marrow. They are able to phagocytose (absorb) viruses, bacteria, tumor and parasitic cells. Regulate hematopoietic function and participate in blood clotting.
The normal blood test for monocyte content is 3-11%.
- an increase in monocytes when deciphered indicates viral, bacterial (tuberculosis, syphilis, brucellosis), fungal and parasitic infections, inflammation in the regeneration stage, systemic autoimmune diseases (systemic lupus erythematosus, rheumatoid arthritis), leukemia.
- a decrease in monocytes in a blood test is possible during purulent-inflammatory processes, aplastic anemia, in the postoperative or postpartum period, and when taking steroids.
Segmented neutrophils are reduced - possible reasons
A decrease in the number of neutrophils in the blood most often indicates a protracted course of some disease of viral etiology. These cells do not stay in the bloodstream for long. As they mature, they transform from rod-nuclear to segmented, and within 2-3 hours they leave the bloodstream, concentrating in inflamed tissues.
If the human body has not been subjected to any complex or immune-suppressing procedures, then we can assume:
- severe viral infection, such as measles or rubella.
- allergic reaction;
- infection after a bite, for example, malaria;
- presence of helminths;
- hereditary pathology.
In addition, neutrophils in the blood decrease as a result of:
- radioactive exposure;
- taking a certain group of medications;
- undergoing chemotherapy;
- exposure to exotoxins, poisons and certain chemicals on the body.
To make an accurate diagnosis, it is necessary not only to donate blood for analysis, but also to obtain a conclusion from the doctor conducting the examination. The presence of helminths is easily determined using laboratory tests, and infection with malaria should be preceded by a trip to an exotic country and a local insect bite. Therefore, the results of a blood test are not a diagnosis, but a reason to undergo a more in-depth examination to identify or refute a low neutrophil count.
However, with the help of a blood test, it is easier for the doctor to determine the etiology of the disease if the patient comes with complaints about the severity of any symptoms. For example, if the transcript indicates that segmented neutrophils are lower and lymphocytes are higher than normal, this will indicate that the patient has contracted a viral infection and does not need antibacterial therapy.
Reasons for deviations from the norm
There are many reasons that can provoke deviations from the norm. The same factors can lead to low and high cell levels.
- Reduced neutrophils in the blood
Reasons for the increase
The human immune system reacts sharply to various external and internal factors. That is why there can be many reasons for the increase in the number of band cells.
The most common of them:
- Progressive type 1 diabetes mellitus.
- Long-term use of antibacterial medications, which provokes a weakening of the immune system.
- Viral and cold pathologists in the acute stage.
- Burns, cuts and other injuries to the skin, especially when a large area is affected.
- Gastric ulcer in the acute stage, gastritis.
- Bronchitis in acute and chronic form.
- Myocardial infarction, ischemic stroke.
- Poisoning by the breakdown products of ethyl alcohol.
- Allergic reaction to medications, food or other substances.
- Anemia of varying severity.
- Inflammatory pathologies of joints.
- Infection of the body with intestinal parasites.
- The presence of trophic ulcers on the patient’s body.
- Blood poisoning of the initial or advanced stage.
- The presence of malignant tumors in the body and their decay.
In addition, pathologies of muscles and nerve endings of inflammatory origin can provoke an increase in cell levels.
Reasons for the downgrade
Factors that influence an increase in indicators can also cause a decrease in them.
However, there are other reasons that can lead to deviation:
- Damage to the bone marrow by malignant neoplasms, spread of metastases in the body.
- Systemic diseases.
- Viral pathologies, such as hepatitis or rubella.
- Severe anaphylactic shock threatening the patient's life.
- Advanced tuberculosis.
- Endocarditis.
- Deficiency of folic acid in the body.
- Exhaustion of the body as a result of excessive stress and malnutrition.
- Bacterial pathologies of internal organs and skin.
One or more reasons lead to changes in indicators and aggravation of the patient’s condition.
How to increase neutrophils
It is impossible to buy a medicine that can increase neutrophil levels. However, it is still possible to influence their content in the blood. For example, if a decrease in phagocyte cells occurred while taking sulfonamide antibiotics, it makes sense to review the course of therapy with your doctor and replace the drugs.
In some cases, the production of neutrophils is affected by a pronounced imbalance of nutrients in the body. The most commonly reported levels of vitamin B9, known as folic acid, and B12 are significantly reduced. Therefore, often, if there is a lack of neutrophils, they additionally take an analysis for vitamin deficiency and prescribe a course of group B. 10-14 days after restoring the balance of nutrients in the body, an increase in the number of neutrophils is observed, which is fixed within acceptable values.
Pathological causes of growth
The norm of neutrophils in the blood changes in most cases due to pathological reasons, the main of which are:
- inflammation of infectious or autoimmune origin;
- endocrine pathologies;
- tumor growth, metastasis;
- physician error during surgery (iatrogenic factor).
There is an exception to the rule: neutrophils can remain normal against the background of a manifest pathological process, which indicates depletion of the immune system and requires immediate adequate treatment.
Reasons for the downgrade
A decrease in the number of neutrophils in the blood compared to the norm is called a shift in the leukocyte formula to the left. There are several reasons for this condition:
- HIV;
- aplastic anemia;
- severe infections;
- the period after a serious illness, prolonged fasting, cachexia;
- alcoholism;
- hepatitis;
- sepsis;
- radiation sickness;
- intoxication of various etiologies, taking medications (antibiotics, antiviral anti-inflammatory drugs, drugs for the treatment of hyperthyroidism, for chemotherapy);
- deficiency of minerals, B vitamins;
- bone marrow damage;
- enlarged spleen;
- metastasis of cancer of any location to the bone marrow or myeloproliferative processes;
- genetic predisposition;
- hyperglycemia;
- idiosyncrasy, when the reason for the decrease in the concentration of neutrophils in the bloodstream is unclear.
Special cases of decreased neutrophils
We are talking about genetically determined neutropenia, which is quite rare, but affects the result of a blood test. This:
- benign chronic neutropenia is asymptomatic, there is no danger to life, but when interpreting the analysis, this point is always taken into account;
- cyclic neutropenia occurs in one person per million, does not affect the quality of life, manifests itself in a periodic causeless decrease and then restoration of neutrophils to normal;
- Kostmann's syndrome is a condition when neutrophils are deprived of the opportunity to mature, as a result a person is deprived of natural protection and constantly suffers from all possible infections. Today, provided that the pathology is detected in a timely manner, patients are given courses of drug correction.