Hyperemia is
The definition of Hyperemia comes from the merger of two Greek words, where “hyper” means too much, and “haima” means blood. When blood accumulates in some part of the body or near some organ, we speak of hyperemia. Externally, it manifests itself as redness of the problem area, and sometimes the body temperature may rise locally. Sometimes a rush of blood causes tissue swelling.
There are several reasons that cause hyperemia. First of all, possible pathologies of the blood supply are identified: the inflow and outflow of blood in a specific area. If there are no problems in the circulatory system, then other possible causes are determined, including:
- temperature changes;
- stress;
- hormonal disorders;
- allergic reactions;
- infectious lesion;
- burn.
It is necessary to eliminate hyperemia from the diagnosis, since it is not a disease in itself, but is considered by medicine exclusively as a symptom.
Diagnosis of coronary heart disease
Usually, complaints and symptoms characteristic of coronary heart disease help to suspect the disease.
To confirm myocardial ischemia, instrumental and laboratory diagnostic methods are used. Tests for coronary heart disease may include:
- Leukocytosis and decreased hemoglobin in a general blood test.
- Increased cholesterol and glucose, changes in the lipid profile according to biochemical blood tests.
- An increase in specific enzymes formed during the destruction of cardiomyocytes - creatine phosphokinase (its special fraction - MB) during the first 3-4 hours of a heart attack (lasts 48-72 hours), troponin-I, troponin-T (their level increases 6 hours after a heart attack and remains elevated for 7-14 days), aspartate aminotransferase (AST) (exceeds the normal level 8-12 hours after the onset of pain, normalizes within 3-4 days), lactate dehydrogenase (begins to exceed the normal level 14-48 hours after the onset of symptoms, returns to normal on days 7-14), myoglobin (increases 2 hours after the onset of symptoms and normalizes within 24 hours) in the blood.
- Elevated C-reactive protein and homocysteine levels are a risk for sudden cardiovascular events.
- Increased blood clotting according to the results of a coagulogram may also increase the risk of developing certain forms of coronary artery disease.
Instrumental research methods can be invasive or non-invasive. In the latter case, the following is used to diagnose coronary heart disease:
- electrocardiography;
- ultrasound examination of the heart - Echo-CG;
- Holter ECG monitoring;
- stress ECG tests: treadmill and bicycle ergometry;
- PET/CT of the heart.
Functional load tests are widely used.
They are used, among other things, to detect the early stages of coronary artery disease or a painless form of the pathology, when the disorders cannot be determined at rest. Walking, climbing stairs, exercises on exercise machines (an exercise bike, a treadmill), accompanied by ECG recording of current indicators, are used as stress tests for suspected coronary heart disease. The standard and most accurate method for this is diagnostics using a treadmill (treadmill) and an exercise bike (bicycle ergometry). Positron emission tomography (PET) is used to diagnose viable cardiac muscle cells. Radiopharmaceuticals are used, the accumulation of which in heart cells reveals viable and necrotic areas.
Among the invasive techniques, coronary angiography is used - x-ray examination of blood vessels using a contrast agent.
Types of hyperemia
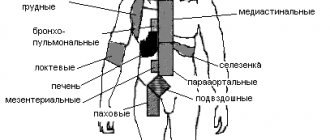
Hyperemia is primarily considered as a pathology of the circulatory system. There are two types of pathological hyperemia:
- arterial;
- venous.
Arterial is called excessive blood supply to an organ when the arteries supply large volumes of blood that the venous system does not have time to remove. Arterial hyperemia can be physiological when more blood begins to flow to the organ during increased load. And venous is called hyperemia, which occurs during normal blood supply, which the venous system cannot drain due to the resulting pathology. For example, with blockage, thrombosis, or atherosclerosis, the lumen of the vascular bed is significantly reduced, and the passage of blood flow is significantly hampered.
The cause of venous hyperemia may be low blood rheology. When it is thick, it is difficult for the heart to pump it throughout the body system. In such a situation, you need to undergo an examination to confirm the problem, and in case of really thick blood, the doctor will prescribe treatment. Most often, it is enough to buy a drug that thins the blood and reduces the risk of blood clots.
The neurotonic type of hyperemia is said to occur when the tone of the nerve conductors increases under the influence of certain factors. First of all, this is facilitated by emotional activity. The second factor that increases the tone of nerve fibers is infectious diseases affecting the nervous system.
Along with an increase in the conductivity of nerve fibers, there is also a reverse reaction - a decrease in tone. As a rule, this is a temporary phenomenon caused by many reasons, such as tissue compression, swelling, hypothermia. As soon as the obstacle to the passage of arterial blood is removed, the tissues are filled with biological fluid with increased intensity, which causes the effect of hyperemia.
Multiform exudative pathologies
The etiology is still not fully understood. The cause is believed to be an infection present in the body. The disease is usually chronic, with constant relapses. Symptoms of erythema multiforme exudative type are:
- slight increase in temperature;
- pain in muscles and joints;
- rashes with a central papule and clear boundaries of spots, located mainly on the bends of the limbs;
- uneven color of spots;
- symmetrical location of rashes on the body;
- tendency to grow with the formation of “garlands”;
- slight deterioration in general health.
The main difficulty is diagnosis, since the signs partially correspond to a number of other diseases. Before prescribing a course of therapy, differential diagnosis is carried out. Medicines are selected taking into account the age characteristics of the patient.
Facial hyperemia
Facial hyperemia can occur as a result of a complex of vascular problems. A similar situation occurs with high blood flow speed and increased pressure. In addition, a small difference in the oxygen content between arterial and venous blood forces the heart and lungs to work harder, which provokes redness.
After a walk in the frosty air, hyperemia also occurs. It is caused by a sharp narrowing of the thin capillaries of the facial skin in response to low temperatures, which is replaced by a sharp increase in blood flow. This is how the body understands that there are areas of the body that are not protected by clothing, which need to be ensured vitality by being warmed by the bloodstream.
But there is also other redness caused by an allergic reaction to frost. This is the body's pathological response to cold. Such redness does not go away for a long time, even after returning to a warm room. This reaction indicates a decrease in immunity and the body’s inability to protect itself from adverse external factors.
Allergic facial hyperemia can be distinguished from physiological hyperemia by several signs. For allergies:
- redness occurs on all open areas of the body;
- hyperemia may take the form of urticaria;
- skin itching appears;
- the mucous membrane swells;
- there is a flow from the nose or tear duct;
- headache appears.
The temperature rarely rises during an allergic reaction.
Nodular pathologists
The causative agent of erythema nodosum is usually streptococcus, and less often - some other infections. It often occurs against the background of tonsillitis, scarlet fever, and tuberculosis. You can recognize it by the following signs:
- rashes of bright red color, with bulges forming in the subcutaneous layer;
- asymmetrically located spots;
- gradual bluing of the spots, then yellowing, similar to the resorption of bruises;
- presence of fever;
- painful sensations and itching in the affected areas of the skin;
- the presence of multiple seals on the legs.
The patient is prescribed a course of antibiotics, antihistamines, as well as external treatment with antiseptics.
Manifestations of violation
If the gastroscopy conclusion indicates that hyperemic gastric mucosa is observed only in some places, that is, focally, then this indicates the initial stage of inflammation in the walls of the stomach.
It is important to understand that this is not an independent disease. The cause of hyperemia of the gastric mucosa is the development of one or another pathology in the epigastric region. Under no circumstances should you leave your well-being to chance if you begin to be bothered by painful sensations in the upper stomach, nausea and heartburn. Contact your doctor immediately. Hyperemic focal gastric mucosa is one of the symptoms of many diseases of this organ, but they can only be identified with a thorough examination.
In a normal state, the gastric mucosa has a pink tint, a smooth surface, and reflects the shine of the corresponding equipment. The thickness of the folds of the mucosa is 5-8 mm. When straightened with air, the folds should completely disappear and expand.
Signs of the disease
There are the following signs of venous hyperemia:
- a decrease in the temperature of the tissue or organ in the area of venous stagnation;
- cyanosis (cyanosis) of the skin and mucous membranes as a result of filling the superficial vessels with blood, which contains reduced hemoglobin;
- cyanosis appears more on the lips, nose, and fingertips;
- slowing down and stopping blood flow in microvessels;
- increased blood pressure in venules and capillaries;
- increased diameter of venules and capillaries;
- increased volume of tissue, organ, their swelling;
- initially a short-term increase, and then an increasing decrease in working capillaries;
- variability in the nature of blood flow (first - jerky, and then pendulum-like);
- hemorrhages in tissue, internal and external bleeding;
- a decrease in plasma current in microvessels until its complete disappearance;
- initially an increase, and then a developing decrease in lymph formation;
- increased swelling of a tissue or organ;
- development of hypoxemia and hypoxia;
- disruption of tissue or organ metabolism;
- decreased performance of cell-tissue structures.
How dangerous?
In order to cope with gastric hyperemia, it is necessary to eliminate the root cause of its occurrence. After which the swelling and redness will go away on their own. If the pathology is not stopped in a timely manner, serious complications arise:
- formation of multiple benign tumors on the organ wall;
- internal bleeding;
- cancerous tumor;
- lack of iron in the body, leading to anemia;
- chronic hypertrophic polyadenomatous gastritis;
- chronic inflammation of the pancreas;
- cholecystitis.
As inflammation of the mucous membrane progresses, an ulcer of the digestive organ may develop.
As gastritis progresses, a stomach ulcer often develops, which in severe cases leads to the death of the patient. The development of hyperemia of the organ mucosa has a negative impact on the condition of the nail plates, skin and hair. It is possible to prevent serious consequences if you consult a doctor in a timely manner and eliminate the causes of the disorder.
Return to contents
Nutrition and hygiene for redness
During treatment for skin hyperemia, doctors recommend that patients adhere to the principles of proper nutrition:
- Avoid foods and drinks high in sugar, salt, and spices.
- Minimize coffee consumption.
- Avoid alcoholic drinks and fast food.
- Make sure that foods you eat are not hot.
- Include as many vegetables, fruits, fresh berries and lean meats in your diet as possible.
- Steam or bake food in the oven.
- Refuse flour products in favor of cereals.
In addition to normalizing the functioning of the gastrointestinal tract, in order to normalize the appearance of the skin, the patient should follow the rules of personal hygiene.
Features of the procedures for existing areas of affected skin are:
- The need to wash only with warm water, while avoiding friction during the process.
- Do not use cosmetics with a high content of fragrances and fragrances.
- Regularly wipe the skin with soothing and protective creams, lotions, and ointments. When applying the product to the redness, avoid applying pressure or vigorously rubbing the injured area.
- Avoid prolonged exposure to the sun or outdoors during gusty cold winds.
Skin hyperemia is not a disease in itself, but its consequences may require drug treatment. Redness of various types is a reaction of the body to an internal failure, which must be identified immediately after detecting the symptoms of the phenomenon in question.
This is the only way to not only eliminate the disease at its initial stage, but also minimize the risk of maintaining skin defects for life.
Article design: Oleg Lozinsky