Celiac trunk compression syndrome (CTCS) is a rare disease that is one of the causes of chronic abdominal ischemia [1]. Compression of the celiac trunk by the median arcuate ligament of the diaphragm occurs during ontogenesis. In 1965, the American physician J. Dunbar first described this syndrome, which later became known after him [2]. Diagnosis and treatment of SCS are a difficult task for the surgeon, since the presence of extravasal compression detected by instrumental examination methods often does not correspond to the clinical picture and patient complaints. The reasons why in some patients the blood circulation in the celiac trunk is completely compensated by collateral blood flow, while in others ischemia develops, are not fully understood [3]. The clinical definition of SCS can be formulated as follows: extravasal compression of the celiac trunk, confirmed by instrumental research methods, accompanied by clinical symptoms of abdominal ischemia, which cannot be associated with any other disease. The symptoms of this disease are varied: chronic abdominal pain, which occurs or intensifies after eating, can be accompanied by dyspeptic symptoms, neurovegetative disorders, and depressive asthenic-hypochondriacal syndrome.
For many years, the method of choice for SCS was dissection of the median arcuate ligament of the diaphragm using superomedian laparotomy or even thoracophrenolumbotomy, which was accompanied by a severe postoperative period with a large number of complications associated with access trauma [4]. With the beginning of the era of endoscopic surgery, the first reports of laparoscopic decompression of the celiac trunk began to appear [5].
However, since the introduction of this method into surgical practice, questions remain open to this day about indications and contraindications for this operation, surgical technique, intraoperative assessment of the effectiveness of decompression, as well as assessment of treatment results in the early and late postoperative periods.
The purpose of our study is to improve the surgical technique and evaluate the value of intraoperative laparoscopic ultrasound (US), as well as to evaluate and search for ways to improve the immediate and long-term results of laparoscopic decompression of the celiac trunk based on our own experience.
Briefly about the treatment method
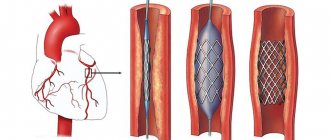
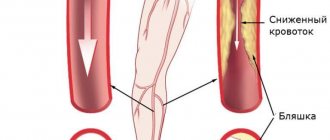
Angioplasty and stenting of the celiac trunk and mesenteric arteries is used to treat the syndrome of chronic intestinal circulatory disorder (angina abdomenalis) or for emergency surgery for acute intestinal circulatory disorder (mesenteric thrombosis).
Intestinal circulatory disorders are rarely diagnosed without a specific focus on certain complaints and are often diagnosed by an experienced clinician only after excluding other causes of abdominal pain.
Previously, when identifying narrowing of the celiac trunk or mesenteric arteries, surgeons adhered to a conservative wait-and-see approach, since open operations on these arteries are very complex and difficult for patients to tolerate. Now, thanks to the development of endovascular technologies, it has become possible to eliminate problems with visceral arteries in a low-traumatic manner.
Material and methods
Since 2005 at the Institute of Surgery named after. A.V. Vishnevsky we performed 21 laparoscopic interventions for extravasal compression of the celiac trunk. The results of treatment were monitored in the long term. Among the patients there were 8 women and 13 men. The age of the patients ranged from 28 to 72 years and averaged 44 years. The duration of the disease until diagnosis and surgical treatment varied from 3 to 20 years and averaged 6 years. The results of surgical treatment in the long-term postoperative period were studied in 17 of 21 patients. The characteristic clinical picture of the disease in the form of severe abdominal pain in the epigastric region, neurovegetative disorders, such as attacks of tachycardia, panic attacks, was observed to one degree or another in all patients. Dyspeptic symptoms in the form of nausea, vomiting, flatulence, and weight loss were observed in 9 patients. Astheno-hypochondriacal syndrome was present in 6 patients. It should be noted that the long course of any disease accompanied by chronic pain syndrome can lead to mental and behavioral disorders. Before making a verified diagnosis, a long history of the disease is accompanied by a diagnosis of irritable bowel syndrome, functional abdominal pain, refractory gastroparesis, aggravation due to drug addiction, and somatoform disorders of the autonomic nervous system in patients. The emergence of psychogenic factors is based on the patient’s prolonged suffering, the “helplessness” of doctors and the modern “diagnostic machine”. The result of this is the patient’s refusal to eat in order to exclude the development of possible abdominal pain, and a decrease in quality of life. Thus, when deciding whether to carry out surgical treatment for decompression of the celiac trunk, it is necessary to involve a psychiatrist both at the preoperative stage and after the operation in order to eliminate the possibility of developing a false relapse of the disease.
In all cases, the diagnosis was established using ultrasound duplex scanning data with measurement of blood flow velocity during respiratory tests, and was also confirmed by CT angiography data (Fig. 1, 2,
Rice. 1. Ultrasonic duplex scanning. Reduction of peak systolic blood flow velocity during inspiration to 150 cm/s.
Rice. 2. Ultrasonic duplex scanning. Increase in peak systolic blood flow velocity to 350 cm/s during exhalation. rice. 3, 4).
Rice. 4. Extravasal compression of the celiac trunk (CT angiography, 3D reconstruction).
Rice. 3. CT angiography. Extravasal compression of the celiac trunk. a — in the sagittal plane; b - in the axial plane.
Ultrasound criteria for extravasal compression of the celiac trunk are: angular deformation of the celiac trunk in the cranial direction in B-mode, acceleration of the peak systolic velocity of blood flow in the celiac trunk in the deep exhalation phase by more than 80% compared to the deep inspiration phase, as well as a decrease in peak systolic velocity blood flow For arterial stenoses, it is generally accepted that stenoses that reduce the lumen of the vessel by more than 50% in diameter are, as a rule, hemodynamically significant [6]. According to some authors, compression of the celiac trunk can be considered hemodynamically significant when the degree of narrowing of the vessel lumen is more than 50%, with a peak systolic blood flow velocity of more than 2 m/s and a blood pressure gradient in the celiac trunk of more than 15 mm Hg. at maximum inspiration [7].
In all patients, according to instrumental research methods, the indicators of blood flow along the celiac trunk were within the range of hemodynamic significance. According to duplex scanning, in the preoperative period the average degree of narrowing of the celiac trunk was 72.5%. Peak systolic blood flow velocity in the celiac trunk (Vs) was 312 cm/s, and the acceleration of peak systolic blood flow velocity in the deep expiratory phase compared to the deep inspiration phase (Vs exp - Vs inhalation) was 144.5 cm/s. Also, before the operation, all patients were comprehensively examined at the Institute of Surgery named after. A.V. Vishnevsky in the scope of ultrasound of the abdominal organs, esophagogastroduodenoscopy, consultation with a therapist and psychiatrist. Thus, the connection between the clinical symptoms of abdominal ischemia and other diseases was excluded.
All patients underwent laparoscopic decompression of the celiac trunk.
Operation technique
Patients were positioned on the table with their legs apart in the Fowler position. 5 trocars (5 and 10 mm) were installed: 10 mm (optical) - in the middle of the distance between the xiphoid process and the umbilicus along the midline, 10 mm - in the right and left hypochondrium along the midclavicular lines for the hepatic retractor and working instrument, respectively, 5 mm - under the xiphoid process in the midline and 5 mm along the anterior axillary line on the left for the clamp and working instrument, respectively.
At the first stage, all patients underwent topical diagnosis of the celiac trunk using laparoscopic ultrasound, which also determined the extent, degree of narrowing and deformation of the celiac trunk, and characteristic poststenotic dilatation.
Intraoperative ultrasound navigation allows you to quickly find and isolate the celiac trunk, which is especially important in the situation of an anatomical anomaly in the location of the vessels of the coelomesenteric region, which occurs in 45% of cases, as well as in conditions of severe abdominal obesity.
Two types of access to the median arcuate ligament of the diaphragm were used: antegrade or retrograde, and the decision on the choice of access was made intraoperatively depending on the specific anatomical situation and the location of the anatomical structures relative to each other. Antegrade dissection consisted of dissection of the hepatogastric ligament in the avascular zone to create access to the right crus of the diaphragm, from which dissection continued in a caudal direction. To identify the muscle fibers of the chiasm of the diaphragm, dissection was performed in the retroesophageal space. The muscle fibers of the chiasm of the diaphragmatic crura were cut with a hook using monopolar coagulation to expose the anterior surface of the aorta. An important point when using both antegrade and retrograde approaches was the extensive dissection of the muscular chiasm of the diaphragmatic crura above the aorta up to 3-4 cm in order to prevent the occurrence of restenosis in the postoperative period due to scarring of the dissected structures.
In order to better visualize the median arcuate ligament, traction of the stomach downwards and to the left was performed with an atraumatic clamp. The intersection of the ligament fibers was performed with a hook using monopolar coagulation. Pulling the ligament fibers from the vascular wall using a hook made it possible to avoid electrical trauma to the aorta and celiac trunk. Particular importance was given to the complete dissection and dissection of all lymphatic and nerve fibers, as well as the nerve ganglia surrounding the mouth of the celiac trunk to achieve the maximum effect from the decompression performed. The procedure was considered complete when the celiac trunk was freed from any external stenotic structures up to its mouth, which was necessarily confirmed by intraoperative laparoscopic ultrasound data.
In most cases, a retrograde dissection was performed, which differed from the previous approach in that the arcuate ligament was accessed by dissecting the main branches of the celiac trunk in a retrograde direction to the orifice of the celiac trunk, with the left gastric or common hepatic artery most often identified and isolated. Delicate traction of the isolated trunks using vascular holds made it possible to obtain adequate exposure of the mouth of the celiac trunk and subsequent decompression.
Advantages of treatment at the ISC
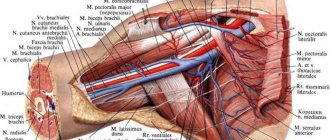
In case of pathology of the celiac trunk and superior mesenteric artery, our x-ray surgeons can perform angioplasty and stenting of narrowings of these significant arteries. The most commonly used approach is the brachial or radial artery.
In the presence of thrombosis of the mesenteric artery or celiac trunk, our clinic performs thrombectomy operations using a special Rotarex probe or selective thrombolysis. Once blood flow is restored, we perform angioplasty and stenting.
results
The average duration of the operation was 102±20 minutes. Intraoperative blood loss in each case did not exceed 50 ml. Technical feasibility was achieved in all cases, regardless of the option of access to the celiac trunk. There were no conversions, intraoperative complications, or complications in the early postoperative period in any of the 21 cases. The duration of hospital stay was 5.8±0.6 days.
Long-term results from 1 year to 12 years after surgery were monitored in 17 out of 21 patients. According to duplex ultrasound scanning, the average degree of narrowing of the celiac trunk before surgery was 72.5%, in the early postoperative period it decreased to 42.5%, and in the long-term period it decreased further to 33% (Fig. 5).
Rice. 5. The degree of narrowing of the celiac trunk according to ultrasound data before surgery and in the postoperative period.
The change in hemodynamic parameters of blood flow velocity in the celiac trunk after surgery also seems significant. Thus, before the operation, the average peak systolic blood flow velocity in the celiac trunk (Vs) was 312 cm/s, and the acceleration of the peak systolic blood flow velocity in the deep exhalation phase compared to the deep inspiration phase (Vs exhalation - Vs inhalation) was 144.5 cm/s. With. In the early postoperative period, these indicators decreased to 193.3 cm/s and 54 cm/s, respectively. In the long-term postoperative period, the peak systolic blood flow velocity in the celiac trunk (Vs) was 172 cm/s, and the acceleration of the peak systolic blood flow velocity (Vs ext - Vs inhalation) decreased further to 43.5 cm/s (Fig. 6).
Rice. 6. Hemodynamic parameters of blood flow before and after surgery.
In our study, intraoperative laparoscopic ultrasound was performed in all cases of celiac trunk decompression, which allowed, in addition to determining the anatomy of the celiac trunk, to objectively assess the adequacy of decompression and, accordingly, obtain good clinical results (Fig. 7).
Rice. 7. Intraoperative ultrasound scanning allows assessing the effectiveness of decompression.
However, 2 out of 21 patients required repeat surgery. In the first case, repeated surgery was required due to incomplete restoration of blood flow along the celiac trunk after laparoscopic decompression. The operation was performed through an open approach a year after laparoscopic decompression, with a positive effect. This case was the first experience of performing laparoscopic decompression of the celiac trunk at the Institute of Surgery named after. A.V. Vishnevsky. Thus, the need for reoperation may be associated with inadequate decompression during the development of the technique.
In the second observation, laparoscopic decompression of the celiac trunk was performed with a pronounced positive effect, which was confirmed by ultrasound data in the early and late postoperative periods. Due to the persistence of the patient's complaints and the presence of instrumentally confirmed hemodynamically significant compression of the celiac trunk, a decision was made to repeat laparoscopic decompression. Repeated laparoscopic decompression was performed successfully, blood flow was completely restored: according to ultrasound examination in the early postoperative period, blood flow in the celiac trunk was laminar in nature, the linear speed of blood flow was 180 cm/s. However, the patient continued to complain of abdominal pain. In this case, we are probably talking about a psychosomatic disorder.
We consider the main criteria for the effectiveness of surgical intervention to be postoperative improvement in hemodynamic parameters of blood flow in the celiac trunk (these parameters go out of the range of hemodynamic significance) in combination with relief of symptoms and improvement in the patient’s quality of life.
The effectiveness of the performed intervention in the long-term postoperative period was assessed clinically, according to postoperative instrumental examination, as well as using a questionnaire using the SF-36 quality of life assessment system. According to the SF-36 questionnaire, 17 out of 21 patients were surveyed twice: in the preoperative period and one year after the intervention. Before the operation, the average value of the physical component of health was 38 points, psychological - 31 points, pain intensity was 28.7 points. In the postoperative period, the studied criteria were assessed with a large number of points, which indicated an increase in the quality of life and a decrease in pain intensity: the physical component of health was 41.5 points, the psychological component was 35.8 points, the pain intensity criterion was 40.2 points (Fig. 8 ).
Rice. 8. Assessment of quality of life according to the SF-36 questionnaire.
Indications and contraindications for the treatment method
Indications:
Celiac stenosis more than 60% with chronic abdominal ischemia syndrome
Stenosis of the superior mesenteric artery more than 60% (symptoms of intestinal vascular insufficiency are not a mandatory indication, the fact of stenosis is sufficient)
Stage of endovascular treatment of acute mesenteric obstruction (mesenteric thrombosis)
Contraindications:
- Allergy to iodine
- Thoracoabdominal aortic aneurysm (without aneurysm surgery)
- Stage of intestinal necrosis with mesenteric thrombosis
Clinical picture
Dunbar syndrome can occur for a long period of time without any symptoms. In the initial stages, the only sign of celiac stenosis is the appearance of causeless pain in the abdominal cavity. Unpleasant sensations usually occur after eating and are present for several hours. When the celiac trunk is compressed, the pain is predominantly localized in the epigastrium. It can be paroxysmal, constant, aching.
Increased symptoms of compression stenosis of the celiac trunk of the abdominal aorta occur under the influence of the following factors:
- intense physical activity;
- eating;
- stress;
- prolonged absence of bowel movements;
- wearing tight or uncomfortable clothing;
- lifting weights;
- prolonged sitting.
To alleviate their condition, patients are forced to limit themselves in food. The pain intensifies when eating sweet, cold or spicy foods. The appearance of discomfort is preceded by even performing simple household chores - cleaning, washing, ironing.
Gradually, as the disease progresses, additional symptoms appear - nausea, flatulence, diarrhea combined with constipation, a feeling of fullness in the stomach, heartburn. Typically, patients lose weight, experience an increase in body temperature to low-grade levels, and experience a loss of strength. Many patients complain of excessive sweating and tachycardia.
Preparing for treatment
Standard examination before surgery:
- Clinical blood and urine tests, biochemical blood test.
- Coagulogram, platelet aggregation
- Gastroscopy (examination of the stomach)
- X-ray of the lungs
- ECG
- ECHO cardiography
- Ultrasound of the abdominal organs, aorta and arteries of the extremities
- Multislice computed tomography with contrast of the aorta and its branches
Before surgery, you must abstain from eating for 8 hours and liquids for 2 hours. No other preparation activities are required.
How the treatment method works
The operation is performed under local anesthesia in the access area. Perhaps access will be on the thigh or in the elbow area. The surgical field is treated with an antiseptic and covered with sterile sheets.
The surgeon performs local anesthesia at the puncture site, after which the artery is punctured with a special needle and a short tube is installed - an introducer.
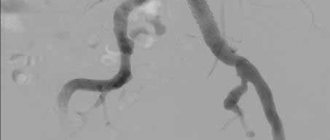
All further work with the vessels is carried out through the introducer. A special guide is inserted into the abdominal aorta, then a catheter is passed through it, through which a contrast study of the celiac trunk and mesenteric artery is performed. This stage is called selective angiography. It is the definitive diagnostic method. If narrowing of the arteries is confirmed, then the guidewire is inserted below the narrowing site. A balloon with a stent is passed through the guidewire. By expanding this balloon, the narrowing of the artery is eliminated, and the stent strengthens the arterial wall.
After stent implantation, control angiography is required to exclude possible complications. The catheter and introducer are removed from the access site, and bleeding is stopped by pressing or using a special Angiosil suturing device.
Discussion
Despite the fact that a number of authors, both domestic and foreign, recommend open decompression of the celiac trunk as the “gold standard”, nevertheless, as in other areas of surgery, minimally invasive technologies are finding more and more supporters.
Jimenez et al. (2012) in his work collected 7 clinical series of 121 patients who underwent laparoscopic decompression of the celiac trunk, with clinical improvement in 116 patients. The laparoscopic approach was preferable to the open approach due to a significantly lower incidence of postoperative complications and faster recovery. However, during laparoscopic decompression, as the author notes, in the presence of serious technical difficulties, such as bleeding (7.4%) and the development of pneumothorax (2.5%), the risk of conversion is high (9.1%). The same author notes that repeated decompressions were required in the laparoscopic group in 5.7% of cases, and in the open group in 6.8% [8].
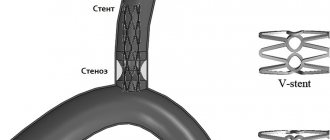
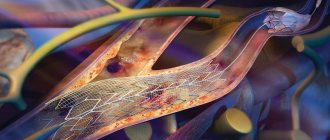
There are few reports in the literature on the use of endovascular methods for the treatment of CSCS - balloon dilatation and stenting of the celiac trunk with extravasal compression of the celiac trunk. Often, the use of interventional radiology methods as monotherapy for SCS leads to the appearance of restenosis above the stent installation site, as well as between stents in cases of endovascular restenting. The literature describes cases of stent displacement from the area of stenosis, as well as cases of stent fracture in the lumen of the celiac trunk (Fig. 9)
Rice. 9. K.T. Fragmented stent in the lumen of the celiac trunk. [9].
Thus, the isolated use of endovascular techniques for Dunbar syndrome has proven to be an ineffective method.
At the moment, there is interest in the possibility of an integrated approach to the treatment of this disease, namely the addition, if necessary, of laparoscopic decompression of the celiac trunk with balloon dilatation or stenting [10].
Regarding the surgical technique, it should be remembered that inflammatory-sclerotic changes in the paravasal and perineural connective tissue in the area of the celiac trunk and celiac plexus can become an additional cause of compression of this vessel, and the development of ganglioneuritis, described by some authors, can cause or aggravate abdominal pain [4 ]. In this regard, one should remember the need to excise the nerve ganglia of the celiac plexus, which, according to some authors, can lead to extravasal compression of the celiac trunk. Thoolen et al. note that the development of clinical manifestations characteristic of SCS is sometimes associated not only with compression of the celiac trunk, but also with a neurogenic factor. The authors draw attention to the fact that relief of the manifestations of SCS can be achieved not only by dissecting the median arcuate ligament and restoring blood flow along the celiac trunk, but also by dissecting the nerve ganglia of the celiac trunk [11].
As for intraoperative diagnostics, the most accessible today is the use of ultrasound of the celiac trunk. For the first time, intraoperative ultrasound began to be used in 1992 by Mayo Clinic surgeons for open decompression of the celiac trunk. Intraoperative ultrasound is necessary to determine the anatomy of the vessels of the coelomesenteric region and to diagnose the anomaly of the origin of the vessels of the celiac trunk in an anatomical region that is difficult to navigate in limited space, as well as to assess blood flow after decompression [12].
An important aspect of the treatment of patients with SCS is the psychological component.
According to a study that assessed the long-term results of celiac axis reconstruction in 44 patients, the best effect was achieved in patients with postprandial pain, aged 40 to 60 years and significant weight loss - more than 9 kg. Clinically unfavorable prognostic factors when assessing long-term outcomes were atypical pain with periods of remission (43%), a history of mental illness or alcohol abuse (40%), age over 60 years (40%), and weight loss not exceeding 9 kg ( 52%). When comparing groups of patients with different development of collateral blood flow, the worst results were obtained in the group with good development, which may indicate the absence of only ischemic pain in this group of patients.
Thus, when deciding on surgical treatment, it is necessary to involve a neuropsychiatrist both at the preoperative stage and after the operation in order to eliminate the possibility of developing a “false relapse” of the disease.
Possible complications during treatment
Complications of the operation itself:
- Rupture of a narrowed artery with bleeding requires emergency open surgery or installation of a special covered stent (stent graft). Fortunately, it is very rare.
- Thrombosis of the reconstructed artery is a rare complication that occurs with increased blood clotting. If preoperative preparation is carried out using antiplatelet preparation, then the risk is minimal. If thrombosis is observed during the intervention, then thrombectomy or thrombolysis (administration of drugs that resolve the clot) is performed. If signs of intestinal circulatory disorders are observed after surgery, the patient is taken back to the operating room and blood clots are removed using Rotarex or special aspiration catheters.
Complications of vascular access:
- Hematoma in the puncture area
- Arterial thrombosis in the puncture area
- Damage to nerves in the puncture area
These complications are extremely rare and can be easily eliminated if detected early.
Therapy methods
Treatment of an aortic defect is carried out surgically. Indications for the operation include the presence of pain in the patient and weight loss. The presence of angiographic signs of pathology must be taken into account. Without surgery, treatment of celiac stenosis, aimed at eliminating disturbing symptoms, is carried out if a person has serious concomitant diseases.
Surgical intervention is performed to release the celiac trunk from compression. It can occur in the traditional open way or using endoscopic techniques. In the latter case, several small incisions are made in the patient's body through which surgical instruments are inserted. The progress of the operation is monitored using a video camera. It is located on an endoscope, which is also inserted into the human body. The use of minimally invasive techniques makes it possible to prevent common complications of operations - hernias, adhesions, inflammatory processes.
If the patient’s medical history contains concomitant pathologies (gallbladder stones), if possible, the surgeon removes them as well. In case of severe stenosis, the patient undergoes artificial expansion of the aorta with the installation of a vascular prosthesis.
Rehabilitation after surgery
After laparoscopic surgery, the patient is observed in the hospital for 3 days, after which he is discharged home. When performing abdominal surgery, the patient requires long-term therapy, the use of antibiotics, and painkillers.
For a month, the patient is prohibited from lifting weights; it is recommended to limit physical activity. The patient may be prescribed enzyme replacement therapy and antispasmodics for a short period. If there is a high concentration of cholesterol in the blood, the patient is recommended a special diet and drug treatment.
The condition of the celiac trunk is monitored one month after the operation. If there are no abnormalities, the patient is recommended to visit his doctor every six months to monitor blood flow in the aorta.
Observation program after treatment method
The results of angioplasty and stenting of visceral arteries are monitored using ultrasound control after 3 months and then annually.
One year after the intervention, it is advisable to perform multislice computed tomography with contrast of the abdominal aorta and its branches.
After treatment, the patient is prescribed antithrombotic drugs. Most often these are aspirin and clopidogrel (Plavix). These medications must be taken regularly, and doctors must be notified before performing any other interventions.