Treatment tactics for spinal stenosis can be conservative (without surgery), interventional or surgical. Stenosis
is a chronic degenerative process in which the intervertebral foramen, central spinal canal, or lateral recess gradually narrows.
Ultimately, this leads to compression (squeezing) of the spinal cord roots and nerve endings. The patient experiences severe pain in the back or neck, numbness and weakness of the limbs, and other neurological symptoms listed below. The disease progresses due to the fact that fragments of growing cartilage or bone tissue (osteophytes) and hypertrophied soft tissue (ligaments and muscles) wedge into the space occupied by the nerve roots.
Degenerative spinal stenosis is caused by injuries, genetics, metabolic disorders, osteochondrosis, arthrosis or other diseases of the musculoskeletal system. In the initial stages of the degenerative cascade, symptoms of spinal stenosis may not bother you at all. However, if the situation worsens over time, then it is no longer possible to cure the disease without surgery. Removal of stenosis is possible only surgically. In this case, non-traumatic spinal surgeries are performed to decompress (and sometimes stabilize) the deformed segment.
Relative stenosis
The central spinal canal narrows to 12-10 mm.
Treatment of relative stenosis without surgery often gives good results.
The patient is prescribed complex therapy, which includes medications (NSAIDs, NSAIDs), physiotherapy, and exercise therapy. In our clinic, specialists from the Pain Treatment Center will help you choose an effective treatment strategy for central relative stenosis. Don't put off seeing a doctor. Degenerative stenosis does not go away on its own. Over time, the disease worsens and at the next stage causes back or neck pain, and sometimes also neurogenic intermittent claudication syndrome (for example, with lumbar stenosis L3, L4, L5
), paralysis of the limbs.
Causes of spinal stenosis
The pathology can be congenital, but most often it is a consequence of an incorrect lifestyle, mainly sedentary, or traumatic back injuries. Diseases that can lead to stenosis:
- Bone tuberculosis;
- Osteochondrosis;
- Arthrosis of the joints;
- Rheumatic joint pathologies;
- Neoplasms of the spinal cord - they can also fill the space and put pressure on the nerve endings, similar to cartilage and bone tissue.
Absolute stenosis
The central spinal canal narrows to 10 mm or less. Treatment of absolute stenosis with conservative methods sometimes no longer gives the desired effect. At this stage, pain in the limbs becomes a serious obstacle to an active life. Especially if the patient has neurological symptoms: pain radiates to the legs and hips, there is a feeling of muscle weakness, and the sensitivity of the limbs decreases. Unlike relative stenosis, absolute stenosis is characterized by pronounced clinical symptoms and may be an indication for spinal surgery. Expansion of the central spinal canal by surgery may be most appropriate, since there is a serious risk of complications without surgery. For example, irreversible paralysis of the limbs, which occurs due to vascular ischemia and circulatory disorders in the spinal root.
Diagnostics
- Studying the patient's complaints - the doctor asks about the location of the pain, its manifestation, and the presence of accompanying symptoms.
- Physical examination - the patient’s posture is studied, the presence of scoliosis, palpation and percussion diagnostics are performed.
- X-ray – X-ray will show bone formations and can also evaluate narrowing of the intervertebral canal to confirm the diagnosis of relative stenosis. If a narrowing of the lumen of less than 10 mm is detected, the patient is diagnosed with absolute stenosis.
- Multislice CT scan – detects degenerative processes of bone and cartilage tissue.
- A myelogram is an x-ray with contrast that allows you to evaluate the degree of pressure on the nerve roots.
- Magnetic resonance imaging – visualizes the condition of soft tissues and the spinal cord.
Lumbar stenosis
An extremely common type of degenerative stenosis, which is diagnosed in 85-90% of cases. Symptoms significantly reduce the patient’s quality of life, since lumbar stenosis is characterized not only by pain in the back and lower back, but also in the limbs. Very often manifests itself as a syndrome of neurogenic intermittent claudication. The patient feels weakness, numbness and pain in the legs. It is important to understand that paresis of the limbs is completely reversible only with timely treatment. The most common clinical cases include L3 - L4 or L5 - L4 stenosis (low back pain radiating to the leg). Another common variant is L5-S1 spinal canal stenosis. At this level, the lumbar region passes into the sacral region, that is, it is a fairly mobile and susceptible to load segment. With lumbar stenosis L5 - S1, the patient also suffers from pain that “radiates” to the legs.
If there are indications for surgery for lumbar stenosis, neurosurgeons at the Pirogov Clinic perform them using the latest endoscopic technology or microsurgical instruments. This eliminates the need for additional installation of implants and metal structures. Thus, patients recover in a short time - without heavy rehabilitation.
Risk factors
There is a category of people who are most susceptible to the disease absolute spinal canal stenosis at the level of the lumbar, chest and neck. This disease predominantly affects older people. This is caused by age-related changes and degenerative spinal diseases. In the age group (50 years and older), this figure is 1.8-8%.
Most often, acquired spinal canal stenosis occurs at the level of l5 s1 and l4 l5 of the last stage of spinal osteochondrosis, that is, when the bone tissue of the vertebral bodies and osteophytes actively grows.
Cervical stenosis
Less common than lumbar stenosis. However, due to the high mobility of the segment and its comparative fragility, spinal surgery (endoscopic or microsurgical) may require additional installation of an intervertebral disc implant or interbody cage. This is necessary to stabilize the spinal segment and prevent the development of degenerative complications in the future. With cervical stenosis, local pain occurs, radiating to the arms and atrophy of the muscles of the upper extremities. Neurosurgeons at the Pirogov Clinic prefer minimally invasive endoscopic operations and interventional pain treatment, which avoid traumatic operations with the installation of metal structures.
If you have been diagnosed with cervical stenosis and have been experiencing pain that is resistant to conservative therapy for more than 12 weeks, send the images to your neurosurgeon through a special form on our website to clarify which treatment would be most appropriate in your case.
Prevention
The most effective way to prevent the development of the disease is regular moderate load on the spine. This may be an exercise program developed specifically for you, or coordinated with doctors ( orthopedist
and vertebrologist) a course of classes in any sports club.
It is important to constantly monitor the position of the spine - correct posture should become habitual; it is important to remember this not only when sitting on a chair, but also while walking, lifting a load and even resting.
Symptoms of spinal stenosis
- Pathological compression of the nerve roots, which leads to their ischemia, causes specific symptoms of spinal stenosis:
- Back pain that occurs when walking and radiates to the legs (legs, front or back of the thigh);
- Numbness and discomfort in the legs occur with a certain position of the spine (bending the torso, walking down the stairs, prolonged static standing position);
- Back pain becomes less intense or disappears altogether with a certain position of the spine (for example, if the patient is sitting, bending or squatting);
- Muscle weakness, numbness and decreased sensitivity of the limbs are especially noticeable after physical activity;
- Problems with urination and bowel movements;
- Problems with potency and erectile dysfunction.
- If, along with severe pain and paresis of the limbs, the patient experiences the last 2 symptoms, emergency spinal surgery may be necessary.
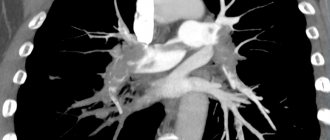
MRI images BEFORE
and
AFTER
surgery for foraminal spinal stenosis using the endoscopic method.
The roots are marked in red (dots and lines). Blue color shows the bone-ligamentous structures that compress the root. The green arrow, as well as the white color in the pictures, shows the free space for the spine. The goal of the operation has been achieved! Endoscopic decompression was performed by a neurosurgeon, a doctor of the highest category, candidate of medical sciences. Sciences Meredzhi Amir Muratovich
.
Complications
If timely treatment of lumbar, cervical or thoracic spinal canal stenosis is not started, pathological manifestations of this disease are possible. Complications are also observed if there have been other spinal injuries (sports injury, fall from a height, etc.). In this case, increased compression of the spinal cord occurs. The resulting hematomas, scars, fragments of the spine, and displaced vertebrae can put pressure on it.
The most severe complications are:
- paresis;
- paralysis of limbs;
- pelvic disorders that manifest themselves due to damage to the nerve roots of the spinal cord with a surgical instrument;
- a slowly and gradually progressing adhesive process, which additionally compresses the roots and the spinal cord itself.
The most rare inflammatory processes occur in nerve elements, membranes and vertebrae. This is due to the fact that after surgery for lumbar spinal stenosis, strong antibiotics are used. But it is still not uncommon that the consequences after surgery of spinal stenosis of the lumbar, cervical and thoracic region give more severe consequences than the disease itself.
Diagnosis of stenosis
You should not guess about the disease based on the symptoms. Diagnosis of spinal canal stenosis is only possible using MRI results. The quality of the images must be at least 1.5 Tesla so that the doctor can accurately determine the specifics of the degenerative change, its location, and then prescribe effective treatment. The patient is also prescribed a survey spondylography with functional tests, which allows one to determine the mobility of the cervical, thoracic or lumbar segment. If there is a possibility of facet syndrome, CT and selective blockade of intervertebral joints may be additionally prescribed. If there are indications for spinal surgery or interventional pain treatment, diagnosis and treatment tactics are prescribed individually, depending on the clinical picture.
Causes of occurrence and development
Before starting treatment for lumbar or cervical spinal stenosis, you should find out what causes the onset and development of the disease.
A congenital or primary type of stenosis is formed during the intrauterine development of the human embryo. This happens in the period from 3 to 6 weeks of development. The genetic factor plays a role here. But absolute spinal canal stenosis can also develop due to infectious, toxic factors that affect the fetus.
Also the cause of congenital stenosis is:
- chondrodystrophy or achondroplasia (chronic). This manifests itself in intrauterine bone growth disorder. In this case, the spinal canal narrows due to shortening or thickening of the vertebral arches, fusion of the vertebrae themselves;
- Diastematomyelia. It is characterized by bifurcation of the spinal cord, separation of the spinal canal by a septum (it consists of either bone or cartilage tissue).
Secondary spinal stenosis appears and develops in childhood or in adulthood.
The following reasons may contribute to this:
- traumatic displacement of the vertebrae or intracanal hematomas;
- changes in the intervertebral joints, which manifest themselves in the growth of bone tissue inside the spinal canal. These changes are degenerative-dystrophic in nature;
- anatomical defect of the spinal arch;
- intervertebral hernia;
- inflammation in ankylosing spondylitis (in this case, the capsules of the intervertebral joints thicken);
- Forestier's disease;
- cysts and tumors that appear inside the spinal canal.
Regardless of the cause, treatment for spinal stenosis should begin as soon as the disease is detected.
Surgery for spinal stenosis
Doctors at the Pirogov Clinic treat degenerative stenoses both conservatively and surgically. All spine surgeries are performed using the latest endoscopic or microsurgical technology, as well as X-ray or radiofrequency equipment.
In most cases, preference is given to endoscopic operations for spinal stenosis
. They allow you to avoid the installation of implants - with the exception of cervical stenosis and cases where spondylolisthesis and instability of the spinal segment are also observed. In addition, such operations are characterized by maximum controllability, minimal risks, and for patients, rapid recovery after endoscopic surgery for spinal stenosis is tolerated most comfortably. The pain in the legs goes away immediately after the operation, and hospitalization in the clinic is only 1 day.
Find out more about endoscopic spine surgeries.
Stenosis surgery performed using microsurgical method
, also refers to minimally traumatic interventions. It is advisable (and may even be the only solution) if, along with expansion of the spinal canal and decompression of the spinal roots, stabilization of the spinal segment is necessary. Such operations show good clinical results and, unlike traditional open spinal surgeries, allow the patient to recover quickly and avoid the risk of disability.
Unfortunately, sometimes it is impossible to do without the installation of metal structures and endoscopic surgery is impossible. A difficult case from the practice of neurosurgeon Mereja Amir Muratovich
. The patient developed stenosis complicated by spondylolisthesis due to displacement of the vertebrae, which caused acute compression of the roots of the spinal canal. To avoid destabilization of the L4-L5 spinal segment and avoid severe consequences in the future, it was decided to fix the segment with screws and install an interbody cage. The operation was performed with pinpoint precision—the pain and weakness in the patient’s legs disappeared immediately after the intervention. The case was difficult and exceptional, but thanks to the experience and skill of our specialists, the patient was able to recover within 1 day.
Find out more about microsurgical operations on the spine.
Recovery after surgery for stenosis
After surgical decompression of the nerve endings and spinal roots, the pain in the limbs goes away immediately. Associated neurological symptoms (numbness and weakness) may take a little longer to resolve, depending on how long the patient has endured the symptoms and how much the disease has progressed. For several hours after surgery, the patient can stand and walk around the room. For 1-2 days (depending on the chosen method of surgery for stenosis), the patient is under the supervision of a doctor and medical staff. The doctor can then send him home with recommendations for the recovery period. After a month, it is advisable to come for a follow-up examination with a neurosurgeon - the doctor is always in touch and guides his patients until the recovery is successfully completed. The patient may be indicated for correction of motor habits. As a rule, no further additional restoration measures are required.
Stenosis of the internal carotid artery, vertebral artery
January 6, 2016
In the body, arteries carry oxygen-rich blood from the heart throughout the body. The carotid arteries (one on each side of the neck) deliver blood to the brain. The vertebral arteries, which pass through the spine, supply blood to the back of the brain (brain stem and cerebellum). Carotid artery stenosis is a narrowing of the carotid artery, which usually develops as a result of atherosclerosis. Atherosclerosis is an extremely complex degenerative disease. Today, scientists do not know the main cause of atherosclerosis, however, many components are known that contribute to the development of atherosclerotic lesions. One of the most popular theories states that atherosclerosis occurs as a response to injury to the arterial wall. Factors known to contribute to arterial wall injury include mechanical factors such as hypertension and low wall elasticity, as well as chemical factors such as nicotine, hyperlipidemia, hyperglycemia, and homocysteine. Lipid accumulation begins in vascular smooth muscle cells and macrophages as a result of the inflammatory response to injury. These lipid deposits can narrow or block the carotid artery, thereby increasing the risk of stroke. Factors that increase the risk of developing stenosis include: - Family history of atherosclerosis (any location); - Age. The risk of developing atherosclerosis increases with age, in particular, men under the age of 75 years have a greater risk of developing carotid atherosclerosis than women, but after 75 years of age, women have a higher risk than men; - High levels of low-density lipoprotein (LDL, “bad cholesterol”) and triglycerides in the blood. However, this factor is less pronounced than for coronary heart disease; — Smoking; — High blood pressure (hypertension); — Diabetes; — Obesity; - Sedentary lifestyle
As a rule, carotid artery stenosis develops several years later than the coronary arteries are affected. People with coronary artery disease or other atherosclerosis (eg, peripheral artery disease) are at higher risk of developing carotid artery stenosis. There are no symptoms of carotid artery stenosis, but there are warning signs of a stroke. Transient ischemic attacks (called "mini-stroke") are one of the most important warning signs of stroke. Transient ischemic attacks occur when a “blood clot” briefly blocks an artery supplying blood to the brain. The following symptoms of transient attacks, which are temporary in nature, can last from a few minutes to several hours: - Sudden loss of vision or blurred vision in one or both eyes; - Weakness and/or numbness on one side of the face, or in one arm or leg, or on one side of the body; - Slurred speech, or difficulty understanding what others say; - Loss of coordination; - Dizziness or confusion; - Difficulty swallowing. Transient attacks are a medical emergency because it is impossible to predict whether the condition will progress to an ischemic stroke. If you or someone you know experiences these symptoms, call an ambulance immediately. Immediate treatment may save your life or increase your chances of a full recovery. Transient attacks, to some extent, are harbingers of a future stroke; a major stroke is 10 times more likely to develop in people who have survived transient attacks. An ischemic stroke occurs when a blood vessel in the brain becomes blocked for one reason or another. The brain is unable to accumulate and store oxygen, and functions as long as the network of blood vessels provides it with arterial, oxygen-rich blood. A stroke causes a lack of blood supply, causing the surrounding nerve cells to be deprived of nutrients and oxygen. If brain tissue is not supplied with oxygen for more than 3 to 4 minutes, the brain begins to die. A stroke can occur if: - the artery becomes significantly narrowed as a result of a blood clot; - part of the blood clot breaks off and moves to a smaller-caliber cerebral artery; - A blood clot blocks a narrowed artery.
Stroke can also occur as a result of other diseases, such as bleeding in the brain (intracerebral hemorrhage), subarachnoid hemorrhage, atrial fibrillation, and cardiomyopathy. Diagnostic tests include:
— Doppler ultrasound of neck vessels. This is a vascular test that uses ultrasound waves to study the presence of narrowing of the carotid arteries. This is the most common test used to evaluate the condition of the carotid arteries;
— Angiography of the carotid arteries. During this invasive procedure, a catheter is inserted into a blood vessel in the arm or leg and connected to the carotid artery. At the next stage, a contrast agent is injected into the catheter and an X-ray of the carotid artery being studied is taken. This test can determine the extent of narrowing or blockage of the carotid artery, determine the risk of stroke, and assess the need for further treatment, such as carotid stenting or surgery;
— Magnetic resonance angiography (MRA) is a scan using a contrast agent that uses a magnetic field and radio waves. MRA provides images of the carotid arteries. In many cases, MRA can provide information that cannot be obtained during X-ray and ultrasound examinations. This test can provide important information about the carotid and vertebral arteries and the degree of their stenosis.
- Computed tomography (CT) of the brain may be performed if a stroke or transient attack is suspected. This test can identify areas of damage in the brain.
— Computed tomography with angiography is a study that uses advanced CT technology to obtain high-resolution 3D images of the carotid arteries. CT angiography allows doctors to determine the degree of stenosis in the carotid and vertebral arteries, as well as evaluate the blood vessels leading to these arteries.
Lifestyle changes.
To prevent the progression of carotid artery stenosis, the National Stroke Association (USA) makes the following recommendations: - Stop smoking; — Control of high blood pressure, cholesterol, diabetes and coronary artery disease; - Eating foods low in saturated fat, cholesterol and sodium; — Achieving and maintaining the desired weight; - Regular exercise - at least 30 minutes of exercise most days a week. — Limiting alcohol consumption; — Find out if you have heart rhythm problems such as atrial fibrillation, which increases your risk of blood clots, which can lead to stroke. If you have atrial fibrillation, you must take anticoagulant medications.
Medications.
Antiplatelet drugs. All patients with carotid artery stenosis should take antiplatelet medications to reduce the risk of stroke and other cardiovascular complications. In some cases, anticoagulants may be prescribed to reduce the risk of blood clots. Tissue plasminogen activators can be used to treat ischemic stroke to dissolve blood clots. Tissue plasminogen activator is effective if given within three hours of the onset of stroke symptoms.
Therapeutic manipulations
Therapeutic procedures such as carotid endarterectomy or carotid artery stenting are used if there is severe carotid artery stenosis and are aimed at preventing a possible stroke.
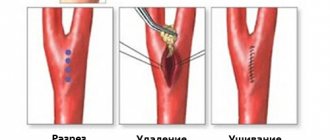
The vascular surgeon at our clinic, based on the studies mentioned above, will give you recommendations on which treatment method is best in your situation. Carotid endarterectomy is the traditional surgical treatment for carotid artery stenosis. Carotid endarterectomy has been shown to be recommended for symptomatic patients with stenosis of 50 percent or more, as well as for asymptomatic patients with stenosis of 60 percent or more. Carotid endarterectomy can be performed under general anesthesia or local anesthesia with intravenous sedation. During the operation, the surgeon makes an incision in the neck in the projection of the blocked carotid artery. After removing the blood clot or atherosclerotic plaque, the surgeon sutures the vessel and then sutures the skin. Blood flow to the brain is restored through the normal pathway. Carotid angioplasty and stenting are recommended as treatment for some patients (eg, those at high risk for surgery) with carotid artery stenosis. Carotid angioplasty and stenting are performed without general anesthesia, but using sedation. During the manipulation, a balloon catheter is inserted into a blood vessel and, under the control of an angiograph (a special X-ray machine), is directed to the site of blockage or narrowing of the carotid artery. Once in place, the balloon is inflated within a few seconds to open or widen the artery. During stenting, instead of a balloon, a stent (a small mesh tube) corresponding to the size of the artery is placed in the narrowed area. The stent remains in place permanently and, by supporting the walls of the arteries, the lumen of the vessel remains open. Studies have shown that carotid artery stenting, when used with an embolic protection device, is safe and effective. Both carotid endarterectomy and carotid angioplasty and stenting usually do not require a long hospital stay. Patients often return to normal activities within one to two weeks.
Why is it worth having surgery for stenosis at the Pirogov Clinic?
The Pirogov Clinic has accumulated 20 years of experience in minimally invasive spine surgeries. The clinic is equipped with modern endoscopic technology, as well as radiofrequency equipment, which in the world practice of spinal neurosurgery is the “gold standard” for the treatment of degenerative diseases of the musculoskeletal system. The operations are performed by a candidate of medical sciences. Sciences, leading neurosurgeon in St. Petersburg and leader of positive reviews from patients on independent platforms (for example, Napopravku.ru). In addition, we can offer our patients:
- Free remote consultation with a neurosurgeon (second opinion) on your disease;
- Availability of all highly specialized medical specialists in one place, as well as our own diagnostic laboratory;
- Service under VHI policies;
- Affordable prices, as well as assistance in obtaining a loan for treatment.
If you have any questions, leave a request for a call back through our website or call (812) 320-70-00 - we are always happy to help you!
Make an appointment