Medical editor: M. Merkusheva, therapist. April, 2021.
Synonyms: Free thyroxine, free T4, Free Thyroxine, FT4.
An examination of the thyroid gland begins with a study of hormonal status, in particular, an analysis of the level of thyroxine (T4). Since this hormone performs many diverse and important functions in the body, laboratory data make it possible to assess the condition of the thyroid gland separately and the endocrine system as a whole.
Of all endocrine hormones, T4 accounts for about 90%. After production by the follicular cells of the thyroid gland, thyroxine is released into the blood, where it is bound by globulin proteins. Only 0.1-0.4% of the T4 hormone remains in a free (unbound) form, which determines their high biological activity. Thyroxine is a precursor to T3
Functions of T4 free
- Ensuring cellular metabolism (thermal, energy, protein, vitamin, etc.);
- Stabilization and regulation of physiological processes in the central nervous system;
- Stimulation of the secretion of retinol (vitamin A) in liver cells;
- Deactivation of triglycerides and “bad” cholesterol in the blood;
- Increased metabolism and bone resorption.
The concentration of the hormone T4 in the blood serum changes throughout the day and reaches its maximum at 8.00 -12.00. The lowest levels occur late at night. Also, fluctuations in thyroxine depend on the season of the year. Experts have found that in the autumn-winter period the level of the hormone increases and reaches maximum values, after which it decreases (summer levels are minimal).
The level of sex hormones in women (estrogen, progesterone) also affects the concentration of thyroxine. During pregnancy, T4 normally decreases by the 3rd trimester. In men, the T4 indicator is stable, but after 40-45 years it begins to gradually decrease.
Symptoms of impaired T4 secretion
If the thyroid gland does not produce enough thyroxine or the thyroid-stimulating hormone that regulates it, a person develops hypothyroidism. This disease is accompanied by clinical signs:
- dry skin and mucous membranes;
- excess body weight gain;
- weakness, lethargy, decreased performance;
- increased sensitivity to cold;
- menstrual irregularities in women;
- problems with bowel movements (constipation);
- hair loss;
- ischemic disease.
If the thyroid gland produces too much T4, the metabolism accelerates and the cells absorb energy faster. However, these changes cannot be considered positive - hyperthyroidism is also dangerous and is characterized by symptoms:
- increased heart rate (tachycardia);
- anxiety, nervousness, irritability;
- sleep disorders;
- tremor (trembling of limbs);
- redness and dryness of the eye mucosa;
- decreased visual acuity;
- sudden loss of body weight;
- puffiness of the face, swelling of other parts of the body;
- indigestion.
In most cases, the balance of hormones is disturbed due to autoimmune pathologies: Graves' disease (hyperthyroidism with high free T4), Hashimoto's thyroiditis (hypothyroidism with low T4).
What can affect the result
- Taking medications: iodine, thyroid hormones, thyreostatics (drugs that reduce the production of thyroid hormones), oral contraceptives (birth control pills), anabolic steroids, glucocorticosteroids, antibiotics, heparin, anticonvulsants, propranolol (a beta-blocker drug), diuretics (diuretics), etc.
- Recent thyroid surgery, radiotherapy.
- Increased body weight.
- Time to apply a tourniquet when drawing blood.
- Time of blood donation: the highest level of free thyroxine is recorded from 8:00 to 12:00, the lowest - from 20:00 to 03:00.
- Time of year: the level of free thyroxine in the autumn-winter period is lower than in summer.
- Pregnancy (free thyroxine levels fluctuate).
You can donate blood for free T4 at the nearest INVITRO medical office.
A list of offices where biomaterial is accepted for laboratory research is presented in the “Addresses” section. Interpretation of study results contains information for the attending physician and is not a diagnosis.
The information in this section should not be used for self-diagnosis or self-treatment. An accurate diagnosis is made by the doctor, using both the results of this examination and the necessary information from other sources: medical history, results of other examinations, etc. The thyroid gland is the largest gland of the endocrine system.
It accumulates iodine and produces iodine-containing hormones - thyroxine (tetraiodothyronine, T4) and triiodothyronine (T3). The synthesis of these hormones requires thyroglobulin (TG), a precursor to T4 and T3, the only source of which is the thyroid gland, but whose secretion is controlled by thyroid-stimulating hormone (TSH). TSH, in turn, is synthesized by the pituitary gland (pituitary gland), which is located at the base of the brain. The main function of the pituitary gland is to maintain a constant concentration of thyroid hormones.
Thyroid hormones are found in the blood both in free form and bound to special carrier proteins. Only free forms of hormones exhibit biological activity. Thyroxine (T4) is one of the two main thyroid hormones.
Thyroxine secretion is regulated by a feedback system that the body uses to maintain stable levels of thyroid hormones in the blood.
If the level of thyroid hormones in the blood decreases, the pituitary gland begins to produce more thyroid-stimulating hormone (TSH), which stimulates the thyroid gland, and the secretion of T4 and T3 increases.
If the level of T3 and T4 in the blood, on the contrary, increases, then the pituitary gland reduces the secretion of TSH, and the thyroid gland, in turn, produces less T4 and T3.
If the thyroid gland does not produce enough T4 and T3 due to thyroid dysfunction or insufficient TSH levels, a person will experience symptoms of hypothyroidism: weight gain, dry skin, cold intolerance, irregular periods and fatigue.
If the thyroid gland produces too much T4 and T3, a person may experience symptoms associated with hyperthyroidism: rapid heart rate, anxiety, weight loss, trouble sleeping, tremors in the hands, and dry, irritated eyes. In some cases, exophthalmos (bulging eyes) is a characteristic symptom.
Indications
- Confirmation of laboratory data when an increase or decrease in TSH levels is detected;
- For symptoms of hypo- and hyperthyroidism;
- Diagnosis and monitoring of the effectiveness of treatment of hypo- or hyperthyroidism (once every 3 months);
- Monitoring of hormone therapy for thyroid diseases (analysis is prescribed once a quarter);
- Identifying the causes of infertility in women of childbearing age.
- Examination of pregnant women with a history of thyroid disease. Impaired production of thyroid hormones can lead to miscarriage, disturbances in the physical or mental development of the fetus;
- Observation of infants born to mothers with diagnosed endocrine pathologies.
Indications for prescribing the study
Free thyroxine (T4 free, Free Thyroxine, FT4) is a fraction of the main thyroid hormone, thyroxine (T4), not bound to proteins.
The study is aimed at assessing thyroid function. The test is carried out:
- with clinical signs of increased or decreased activity of the thyroid gland;
- with an increase in the size of the thyroid gland (goiter);
- with a previously identified change in the level of thyroid-stimulating hormone;
- to monitor treatment for established thyroid diseases.
No. 55 Laboratory assessment of thyroid function
Free thyroxine (Free Thyroxine, FT4) In this study, the concentration of the free fraction of thyroxine, the dominant thyroid hormone, is determined in the blood serum. This study is advisable to carry out in the presence of signs of hypothyroidism or thyrotoxicosis, with a decreased or increased level of TSH, as well as with identified diffuse toxic goiter.
Up to 1 business day
580 RUR Add to cart
Norm of free thyroxine
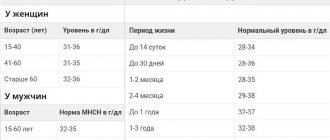
Reference values for thyroxine are not gender specific, but vary depending on the age of the patient.
Invitro laboratory standards for 2021:
| Age | Free T4 level, pmol/l |
| 5 days – 15 days | 13, 47-41,32 |
| 15 days – 30 days | 8,71-32,53 |
| 30 days – 6 months. | 11,42-21,89 |
| 6 months - 13 years | 10,80 -16,40 |
| 13 years – 18 years | 10,20 – 15,50 |
| over 18 years old | 9,00 – 19,05 |
Important! Standards may vary depending on the reagents and equipment used in each particular laboratory. That is why, when interpreting the results, it is necessary to use the standards adopted in the laboratory where the analysis was carried out. You also need to pay attention to the units of measurement.
Helix laboratory data, 2021:
| Age | Reference values, pmol/l |
| < 4 months | 11,5 — 28,3 |
| 4 months - 1 year | 11,9 — 25,6 |
| 17 years | 12,3 — 22,8 |
| 7 – 12 years | 12,5 — 21,5 |
| 12 – 20 years | 12,6 — 21,0 |
| > 20 years | 10,8 — 22,0 |
| During pregnancy | |
| Gestational age | Reference values |
| Until the 13th week | 12,1 — 19,6 |
| 13-28 week | 9,6 — 17 |
| 28-42 weeks | 8,4 — 15,6 |
Important! The interpretation of the results is always carried out comprehensively. It is impossible to make an accurate diagnosis based on only one analysis.
T4 indicators in the female body
The T4 hormone plays a very important role specifically for the female body, as it significantly affects reproductive function. When the hormonal background of thyroid hormones is normalized in a woman’s body, eggs are formed correctly and ovulation occurs.
The T4 hormone also controls the following processes in a woman’s body:
- body weight regulation;
- removal of harmful cholesterol;
- speed of metabolic processes;
- prevents thrombus formation.
During pregnancy, the presence of this hormone plays an important role in the formation of the internal organs and systems of the embryo, and also contributes to the proper development of the fetus. In the first trimester, with the help of thyroxine, the embryo's nervous system is formed. And its quantitative indicators influence the further normalization of its development.
That is why in pregnant women the production of T4 increases significantly, and its deficiency in the blood is associated with the transfer of some enzymes into the child’s body. Lack of T4 in pregnant women leads to various pathological changes in the embryo, and in some cases to spontaneous abortion or miscarriage.
As menopause approaches, the concentrations of this hormone in the female body decrease. In addition, there are changes in the amount of T4 depending on the seasons or time of day. In the morning its level is highest, in the afternoon it decreases significantly, and at night the concentration of thyroxine in the blood is minimal. In the autumn-winter period, there is also a clearly expressed increase in the level of this hormone, and in the summer its concentration decreases.
Increase in free T4
- diffuse goiter (increase in the size of the thyroid gland);
- thyroid dysfunction after childbirth;
- therapy with synthetic hormone T4, incl. uncontrolled (self-medication);
- thyrotoxic adenoma or myeloma (thyroid tumors);
- hyperthyroidism (hyperfunction of the gland);
- TSH-independent thyrotoxicosis;
- nephrotic syndrome (kidney damage, generalized edema throughout the body);
- obesity;
- liver disease (chronic form);
- treatment with heparin, amiodarone, furosemide, danazol, valproic acid, tamoxifen.
According to a study that involved about 9,500 people over 65 years of age, high levels of free thyroxine at this age are directly associated with atherosclerotic cardiovascular disease.
Conditions associated with the balance of TSH, free T3 and T4:
| TSH | free T3 | free T4 | State |
| short | normal (moderately elevated) | elevated | Often:
Relatively often:
Rarely:
|
| short | normal | normal | Often:
Rarely:
|
| low (moderately reduced) | short | short | Often:
Rarely:
|
| high | short | short | Often:
Rarely:
|
| high | normal | normal | Often:
|
| normal (moderately elevated) | high | high | Rarely:
|
Increasing T4 levels in the body
An increase in this hormone in the body, not during pregnancy, can be caused by the following reasons:
- obesity;
- glomerulonephritis;
- taking artificial thyroxine preparations;
- presence of HIV;
- multiple myeloma;
- thyroiditis in the acute phase;
- postpartum disorders of the thyroid gland.
At high concentrations of the thyroid hormone T4 in the human body, some characteristic symptoms are observed. Among them are heart rhythm disturbances, tachycardia, increased temper and irritability, increased sweating, tremors of the upper and lower extremities. weight loss, increased fatigue, loss of strength. An overestimation of T4 levels often accelerates the breakdown of fat and leads to an excess of energy, which negatively affects various internal organs, complicating their work and accelerating their wear and tear.
This condition also has a negative effect on the nervous system, which entails frequent mood swings, negative emotional coloring, and trembling throughout the body.
When the level of thyroxine in the human body increases for a fairly long period of time, calcium is washed out from bone tissue, which leads to osteoporosis and frequent fractures.
Decreased free T4
- hypothyroidism (mainly congenital);
- endemic goiter (pathology of the thyroid gland);
- thyroiditis;
- cancer tumors localized in the thyroid gland;
- operations in the gland area, amputation of its individual parts;
- thyrotropinoma (pituitary tumor);
- iodine deficiency in the body;
- inflammatory processes in the pituitary gland and hypothalamus, traumatic brain injury;
- Sheehan syndrome (death of pituitary tissue after childbirth, accompanied by bleeding and hypotension);
- a sharp decrease in body weight;
- use of heroin and other drugs (hormones, oral contraceptives, anticonvulsants, lithium, steroids, etc.).
- lead poisoning.
Interpretation of results in children and adults
The main reasons for the increase in the concentration of free thyroxine
- Hyperfunction of the thyroid gland with:
- diffuse toxic goiter. The development of the disease is preceded by disturbances in the activity of the thyroid gland of genetic, autoimmune or inflammatory origin. Unfavorable factors (stress, respiratory infections) can activate the thyroid gland and provoke the development of the disease;
- thyroiditis – inflammation of the thyroid gland of an infectious or autoimmune nature;
- postpartum thyroiditis. The pathology is considered a variant of autoimmune thyroiditis. The classic manifestation is temporary thyrotoxicosis, which occurs in three phases (thyrotoxicosis, hypothyroidism, recovery).
- Taking synthetic thyroid hormones.
- Excessive intake of iodine into the body (including with radiocontrast agents).
- Pathologies affecting the level and ability of specific proteins to bind hormones (hepatitis and cirrhosis lead to a decrease in the level of thyroxine-binding globulin).
- Tumors of the pituitary gland, accompanied by an increase in the level of thyroid-stimulating hormone.
The main reasons for the decrease in the concentration of free thyroxine
- Weakening of thyroid function in primary hypothyroidism, after removal of a lobe of the thyroid gland, and in case of thyroid cancer.
- Taking thyreostatic drugs.
- Iodine deficiency.
- Secondary hypothyroidism, in which the pituitary gland produces little thyroid-stimulating hormone. Causes: inflammation or neoplasm in the pituitary gland.
- Tertiary hypothyroidism, caused by a decrease in the production of thyrotropin-releasing hormone by the hypothalamus due to traumatic brain injury, inflammatory, autoimmune, and vascular disorders.
If the indicator deviates from the norm, the following studies are additionally carried out: total triiodothyronine (T3 total, Total Triiodthyronine, TT3), free triiodothyronine (T3 free, Free Triiodthyronine, FT3), total thyroxine (T4 total, total tetraiodothyronine, Total Thyroxine, TT4), thyroid stimulating hormone (TSH, thyrotropin, Thyroid Stimulating Hormone, TSH).
Pregnancy and thyroxine
During pregnancy, the female body produces a large amount of sex hormones (estrogens, progesterone), which, in turn, stimulate the activity of the thyroid gland. At the same time, the secretion of transport globulins that bind thyroxine increases, so its concentration gradually decreases.
T4 directly affects the physical and mental development of the embryo. It is free thyroxine that is responsible for the formation of the fetal nervous system. Therefore, if an infant lacks this hormone, the risk of congenital pathologies increases.
Determining the total T4 level during pregnancy is impractical, because During this period, the production of binding proteins in the body is increased. In the test results of a pregnant woman, total thyroxine will always be higher than the reference values, which should be considered the norm.
In healthy women expecting the birth of a child, a slight increase in free T4 concentrations may be observed. Special treatment is not prescribed until the level exceeds the upper limit of normal. Hormone therapy is carried out extremely carefully, constantly monitoring T4 levels, so as not to harm the fetus.
What is the hormone T4 (thyroxine)?
T4 – thyroid hormone
produced by cells of thyroid follicles. Thyrocytes synthesize thyroglobulin from amino acids and iodine, which is a precursor to thyroxine. Thyroglobulin accumulates in the follicles, and, if necessary, thyroxine is formed from it by dividing into fragments.
The main action of the hormone T4
is to accelerate catabolism - the process of obtaining energy from energetically significant metabolites (glycogen, fat). Excessive concentration of thyroxine in the blood leads to rapid heartbeat, irritability, and weight loss. But this does not mean that the hormone is harmful, these are only symptoms of its overdose. Normally, tetraiodothyronine maintains the tone of the nervous system, heart rate and adequate metabolism.
T4 hormone is not the most active thyroid hormone,
for comparison, its activity is almost ten times lower than triiodothyronine. The latter is also called the T3 hormone, since its formula contains 3 iodine atoms. T3 can be formed in the cells of the gland itself, as well as in the cells of the body from its predecessor, thyroxine. Essentially, it is a more active metabolite of T4.
Hormones T3, T4 are also called thyroid hormones
, since they are secreted by the thyroid gland, called “thyroid” in Latin. TSH is also sometimes referred to as thyroid hormone, but this is erroneous, because it is produced by the pituitary gland, located in the brain, and controls the hormone-forming function of the gland.
Often, together with a blood test for the hormones TSH, T3, T4, antibodies to TPO and thyroglobulin are simultaneously determined. Typically, endocrinologists use these indicators to diagnose thyroid pathologies. Sometimes thyroid hormones are studied during the treatment of the disease to determine its dynamics and the effectiveness of the prescribed therapy. This article will provide information about what the T4 hormone is, what functions it performs in the body, and how the analysis of its content is interpreted.
The T4 hormone belongs to the group of iodine-containing thyroid hormones. Its chemical formula contains two residues of the amino acid tyrosine and four halogen atoms of iodine. Synonyms for the T4 hormone are tetraiodothyronine and thyroxine. The substance received its name due to the number of iodine atoms contained in the molecule. Due to its simple structure, the concentration of tetraiodothyronine can be easily determined in the laboratory. For the same reason, the hormone can be synthesized artificially, which is used in hormonal therapy.
Preparing for analysis
- It is better to take blood from a vein in the morning (before 12.00) and only on an empty stomach (the last meal was 8 or more hours ago). You can drink regular water without gas.
- Smoking and/or using nicotine substitutes is prohibited 2-3 hours before the procedure.
- The day before the test, you must adhere to a diet: exclude fatty, fried, smoked and fast food from your diet. It is strictly forbidden to consume energy and tonic drinks and alcohol.
- Intense physical activity, sports and anxiety can also affect the concentration of thyroxine (increasingly). Therefore, during the day (at least) before the test, you need to protect yourself from any stress and physical strain.
- 48 hours before the test, it is advisable to discontinue steroid and thyroid hormones (in consultation with the endocrinologist). You may need to stop taking other medications.
Sources:
- Rui-ting Ma. Influence Factors on Serum Thyroid Hormone Level in Healthy People, - data from the US National Library of Medicine PubMed, 2015.
- Data from the independent laboratory Invitro, 2021.
- Data from Helix Laboratory, 2021.
- Fran Lowry. High Thyroid-Hormone Levels Linked to Increased CVD Mortality, - English-language database of current medical data Medscape, 2021.
- Muhammad Bader Hammami, MD. Thyroxine, - English-language database of current medical data Medscape, 2021.