Prothrombin index (PTI) is one of the indicators of a coagulogram - a digital or graphic expression of a laboratory blood test for coagulation. The PTI is the ratio of the control (or normal) plasma PT to the plasma PT of a particular patient multiplied by 100%. PT (prothrombin time) is the period during which a thrombin clot is formed after calcium and thromboplastin are added to the plasma.
Thus, the prothrombin index shows how active the blood coagulation system is. A decrease in PTI indicates poor coagulation (hypocoagulation), that is, a tendency to bleeding. An increase in the indicator indicates increased coagulability (hypercoagulation) and a tendency to form blood clots.
What is the coagulation system
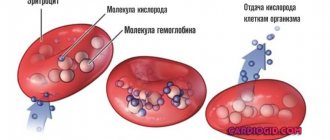
The hemostasis system is very complex, involving many tissue and serum factors. Its launch is really similar to a cascade: it is a chain of reactions, each subsequent link of which is accelerated by additional enzymes.
A simplified blood coagulation scheme looks like this: thromboplastin is released from the damaged endothelium, with the participation of calcium ions and vitamin K, it activates prothrombin. Prothrombin is converted to active thrombin, which in turn triggers the formation of insoluble fibrin from soluble fibrinogen. This process is completed by the stage of retraction of the blood clot, that is, its compaction and the actual blockage of the damage.
At each stage, many more factors are involved in this scheme. In total, there are 13 plasma and 22 platelet types.
References
- Zobova, D.A., Paramonova, T.K., Tyurina, N.A. et al. Pathology of the hemostatic system in very early premature birth. – Journal of scientific articles, health and education in the 21st century, 2021. - No. 8. — P.185-187.
- Ponizovich, E.V., Zolotavina, M.L., Chernyavskaya, O.V. Changes in blood hemostasis in patients suffering from viral hepatitis. — Scientific forum: medicine, biology and chemistry, 2021. — pp. 13-17.
- Haram, K., Mortensen, J., Mastrolia, S. et al. Disseminated intravascular coagulation in the HELLP syndrome: how much do we really know? — The journal of maternal-fetal and neonatal medicine, 2017. — Vol. 30(7). — P. 779-788.
What is prothrombin
This is a glycoprotein produced in liver cells, plasma coagulation factor II.
The synthesis of prothrombin requires vitamin K, so one of the reasons for its decrease is insufficient intake of this vitamin from food or a low level of its synthesis in the intestines.
Prothrombin is an inert protein, its activation occurs under the influence of coagulation factor XII (internal system) or when the endothelium is damaged (external mechanism of hemostasis).
The normal level of prothrombin in the blood is 0.1-0.15 g/l. However, its quantitative determination is not used in routine diagnostics. This is a rather unstable protein, easily destroyed and difficult to separate into a separate fraction and count.
In practice, qualitative tests for prothrombin are used, which reflect its content in the blood only indirectly. They are based on calculating the period of time during which the blood clots when thrombokinase activators are added to it (which in turn activates prothrombin, converting it into thrombin, and thrombin catalyzes the conversion of fibrinogen into fibrin).
Therefore, when we say “test for prothrombin”, “blood for prothrombin”, this does not mean determining its concentration in the blood, as, for example, glucose, hemoglobin or bilirubin are examined. And the result is given not in quantitative units, but as a percentage. This concept characterizes the external mechanism of hemocoagulation as a whole and reflects the activity of the entire prothrombin complex (factors II, V, VII, X).
How are prothrombin tests performed?
The essence of almost all methods for studying the activity of the prothrombin complex is to calculate the time of formation of a fibrin clot immediately after adding activators to the blood, as well as comparing this time with normal values.
Blood is drawn into a test tube with an anticoagulant (sodium citrate). The test tube with citrated blood is slightly heated in a water bath. A reagent consisting of thromboplastin and calcium chloride is added to it. The time of loss of fibrin fibers is measured using a stopwatch. This is prothrombin time (PT). Its normal value is 11-15 seconds.
Having determined the patient's PT, it is compared with the normal prothrombin time (PT). It is usually indicated on the reagent bottle and depends on the activity of the thromboplastin used. Usually this figure is from 12 to 18 seconds (it may be different in each new reagent sample). The ratio of PVN to PT of the subject, expressed as a percentage, is the prothrombin index (PI). Its normal value is 80-105%. The longer the blood clotting time (PT), the lower the PI, which will indicate hypocoagulation.
Prothrombin according to Quick
The test is also based on the ratio of the patient's normal prothrombin time to the patient's PT, expressed as a percentage. But the method is considered more accurate. For the study, several dilutions of plasma are used (1:2, 1:3,1:4) and the construction of a calibration graph. For each dilution, the PT is determined and marked on the graph.
Prothrombin rates according to Quick are from 75% to 140%.
Within the normal protein content, the Kwik and PTI results may be identical. At low contents, these indicators sometimes diverge.
Another indicator is the INR (international normalized ratio). It is mainly used to assess the effectiveness of anticoagulants. This indicator is calculated using the formula:
INR = (patient's PT/normal PT)*value of the international thromboplastin sensitivity index (ISI).
This index is indicated on each package of the reagent. INR allows standardization of the results of PT and IPT performed in different laboratories. The INR value in healthy individuals is 0.8-1.2.
The numbers of prothrombin according to Quick and INR are inversely proportional to each other: if prothrombin according to Quick is increased, then the INR is reduced and vice versa.
Decoding INR
The international normalized ratio is a classic technique. Only one test tube is used, which reduces accuracy, but at the same time allows for rapid research.
The indicator, in contrast to the more detailed method (according to Quick), deviates insignificantly. At least not to the extent that the changes are critical and do not allow clinically correct conclusions to be drawn. That's why this variation is used more often.
The INR can be calculated as a percentage or as a coefficient. The first option was discussed in the table above, and in the latter case it is determined by a decimal fraction, and the range from 0.82 to 1.15 is considered normal. For diseases of the cardiovascular system and lungs, it is possible to increase the level to 3.0.
When is prothrombin tested?
A coagulation test (coagulogram) is not a routine examination; it is not prescribed to all patients in a row. The test is carried out in the following situations:
- The presence of symptoms indicating problems with clotting: frequent nosebleeds and other bleeding, bruising for no apparent reason, bleeding gums when brushing teeth, hemorrhagic rash on the skin.
- Thrombophlebitis of the veins of the lower extremities.
- Examination of the patient before any surgical interventions.
- Pregnant women must be examined.
- Control during treatment with anticoagulants. They are prescribed to patients with arrhythmias, after valve replacement, and for thrombophlebitis. The purpose of these drugs is to increase blood clotting time, but keep it within a safe range. In this case, PT will be increased by 1.5-2 times, PTI and prothrombin according to Quick will be reduced, INR will be increased (safely up to 2-3).
- For liver diseases to clarify its functional insufficiency.
- Before prescribing estrogen-containing hormones, as well as during their use.
In what cases is it necessary to take the test regularly?
Monitoring the INR is necessary when taking Warfarin, Phenilin and other representatives of this group of anticoagulants. The INR norm when taking these drugs is in the range of 2.0-3.5. It must be maintained to adequately maintain the balance between the coagulation and anticoagulation systems.
When the INR exceeds 3.5, hypocoagulation and the risk of bleeding should be considered. When the INR falls below the recommended level, the dose of the drug should be increased. At first, the frequency of the study should be approximately once a week. But when the target INR values are reached, the analysis can be performed once a month.
IPT is needed for monitoring when using Heparin. This is carried out in a hospital setting.
INR and PTI are necessary for screening for disorders in the hemostatic system, as well as for dynamic monitoring when taking Warfarin and Heparin. The norm for women is different from men, and there are also special features for pregnant women. There are also differences in age within this group. For ease of assessment, there are tables.
Prothrombin norms in different groups of patients
The levels of this glycoprotein in the blood vary somewhat among different age groups. In children under 18 years of age, its normal content ranges from 80 to 110%, in adults – from 78 to 145%.
The norms for adult men and women are no different. A moderate increase in prothrombin may occur in women before childbirth.
Prothrombin index
This indicator is determined in all coagulograms. What does prothrombin index mean?
The normal prothrombin index is 80-105%. The greater the patient’s PV compared to normal, the lower his PI will be and vice versa. Accordingly, a low index indicates poor coagulability, and a high index indicates hypercoagulation (propensity for thrombosis).
The prothrombin index test is prescribed in the same situations as the Quick prothrombin test. Basically, both of these values are in direct correlation and in the range of normal content can be the same.
The norm of the prothrombin index during pregnancy differs slightly by trimester:
- I trimester – 80-119%
- II – 85-120%
- III – 90-130%.
Additional examinations
{banner_banstat9}
Auxiliary techniques are used to confirm the diagnosis and identify the causes of deviations from the norm. That is, the primary disorder. An approximate list of procedures is as follows.
- Ultrasound of the liver. Necessary for identifying organic disorders. It is most actively used as a routine technique.
- Scintigraphy is also used. This is already a method of functional research. When there are no structural changes, at least at first glance.
- MRI of the digestive tract is available upon request.
- Blood biochemistry, general analysis.
- ECG, ECHO-KG.
In most cases, this is enough.
How to decipher a coagulogram
This analysis is carried out in order to obtain answers to the questions:
- does the blood clot normally?
- is there a risk of postoperative or postpartum hemorrhage;
- what is the cause of frequent bleeding and bruising;
- what dose of anticoagulants is safe if their use is necessary.
Blood hypocoagulation and tendency to bleeding will be indicated by:
- reduced prothrombin according to Quick (less than 75);
- decreased prothrombin index (less than 80);
- increased prothrombin time (more than 18 seconds);
- increased INR (more than 1.3).
Hypercoagulability and tendency to form blood clots is characterized by:
- increased prothrombin index (more than 110);
- increased prothrombin (above 145);
- shortening of PT (less than 10 s);
- decrease in INR value less than 0.8.
Plasma coagulability index
An equally important indicator is the plasma coagulability index. This is the ability of blood to transform from a liquid state to a thick one. Using this value, the doctor can evaluate the functioning of the digestive organs and excretory system.
Under normal conditions, blood flows in liquid form in the vessels. This helps it fulfill its main purpose and functions, namely the transportation of vital substances to all organs and systems.
Damage to the outer skin or internal tissues provokes bleeding. It is at this moment that the body starts the clotting process, making the fluid in the vessels thicker and thereby creating a blood clot that clogs the wound.
The main reasons for the decrease in prothrombin
We remember that prothrombin is a protein that is formed in liver cells with the participation of vitamin K. It becomes active with the help of several tissue and plasma clotting factors. The gene responsible for normal prothrombin synthesis is recessive and is located on chromosome 11.
In addition, there are also anticoagulant factors in the blood, the increased activity of which can inhibit the components of the prothrombin complex.
The main causes of low prothrombin and IPT (PT and INR are increased) follow from this physiological mechanism:
- Congenital pathology - changes in the genes responsible for the synthesis of prothrombin (quite rare).
- Liver diseases accompanied by decreased function or death of hepatocytes: chronic hepatitis, cirrhosis. The insufficiency of structural units for synthesis leads to the fact that prothrombin in the blood is reduced.
- Vitamin K deficiency. This happens both when there is insufficient intake from food, and when its absorption and synthesis in the intestines is impaired. Therefore, gastrointestinal diseases accompanied by dysbiosis and impaired fat absorption can also lead to its deficiency.
- Reduced levels of blood clotting factors V, VIII, X.
- Autoimmune diseases, including the production of antibodies to prothrombin (more precisely, to the phosphatidylserine-prothrombin complex).
- Low fibrinogen levels.
- 2nd phase of DIC syndrome (exhaustion phase).
- Increased activity of the anticoagulant factor antithrombin III.
- Treatment with anticoagulants (heparin, fraxiparin, warfarin, neodicoumarin).
Reasons for increased prothrombin and PTI
An increase in PTI indicates hypercoagulation and is dangerous for the development of thrombosis (heart attacks, strokes, thrombosis of the veins in the legs, pulmonary embolism). This condition is especially unfavorable after operations and after childbirth.
- Last weeks of pregnancy.
- DIC – syndrome (1st stage).
- The use of estrogen-containing hormones by women (and sometimes men).
- Congenital thrombophilia.
- Excess vitamin K.
- Mutation of the prothrombin gene G20210A (carriers of the defective gene are 2-3% of the population).
- The period after severe operations, burn disease.
- Postpartum stage.
- Malignant tumors.
- Antithrombin III deficiency.
- Antiphospholipid syndrome.
What to do with indicators that do not fit into the norm?
Prothrombin is increased or decreased, what to do?
First, you need to see a doctor. Many people think that the answers to all questions can now be found on the Internet. In fact, this is far from the case. This is especially true for the coagulation system. The information presented on the Internet about this matter is very confusing and 50% of it is completely wrong. This indicates the high complexity of this issue.
Which doctor should I contact?
To the one who ordered the analysis. If you took a coagulogram on your own, first we go to a therapist.
What should you definitely tell your doctor?
- You must list all medications that you are taking or have taken recently, including dietary supplements. Many medications tend to affect coagulogram parameters, and this applies not only to anticoagulants. Thus, Nevigramon, Streptomycin, Tetracycline, Levomycetin, L-thyroxine, vitamin A, and Aspirin in high doses can reduce prothrombin.
The following can increase PTI: contraceptive hormonal drugs, caffeine, antihistamines, high doses of vitamins C, K, corticosteroid hormones.
- Long-term alcohol abuse can also reduce PTI.
- An excess of foods rich in vitamin K in the diet can lead to an increase in prothrombin, and insufficient consumption of them can, on the contrary, lead to a decrease. These are foods such as greens, green vegetables and fruits, liver.
- Women must be informed about their pregnancy.
What additional examinations can be prescribed?
- Liver function test (advanced biochemical analysis with determination of bilirubin, liver transaminases, total protein, albumin).
- Ultrasound of the liver and biliary tract.
- Fibroelastography of the liver for suspected cirrhosis.
- Determination of antibodies to viral hepatitis.
- Extended examination of the coagulation system (APTT, fibrinogen, thrombin time, D-dimers, plasminogen, antithrombin III, plasma fibrinolytic activity, lupus anticoagulant, etc.)
- Intestinal examination (stool analysis for dysbacteriosis, colonoscopy).
How to lower or increase the prothrombin index?
If the readings are only slightly outside the normal range, there is no need to panic. It is possible that some time after stopping some medications, a repeat analysis will not reveal any abnormalities. Many women are concerned about the question - what to do with taking contraceptives? If cardiovascular diseases are diagnosed, definitely stop taking it, but if the woman is generally healthy, the pills can be taken, but the analysis should be periodically monitored.
You can also try to correct PTI with a diet if you are sure that your diet is clearly lacking foods such as greens (parsley, dill, spinach), vegetables (cabbage, broccoli), beef or pork liver. Green tea improves PTI quite well.
If prothrombin levels are elevated and there is a risk of thrombosis, doctors usually prescribe anticoagulants. At the same time, only warfarin will clearly reduce this indicator. New generation anticoagulants (Pradaxa, Xarelto, Eliquis and others) act on other coagulation factors, but the level of prothrombin may not change.
Aspirin also does not change this indicator, but taking it in small doses makes sense to reduce the risk of blood clots.
In what cases should you not waste time on a diet?
- If the coagulogram values are significantly higher or lower than normal.
- There are symptoms of impaired homeostasis: recurrent bleeding or thrombosis.
- Presence of pregnancy.
- Abnormal coagulogram in a child.
- There are other symptoms (yellow skin, dark urine, swelling, rash, itchy skin, etc.)
In these cases, you need to undergo a full examination and find out the cause of the pathology of the coagulation system.
Author:
Akimova Valentina Konstantinova general practitioner