Introduction
One of the most common forms of heart rhythm disturbances is paroxysmal supraventricular tachycardia (SVT).
In the general population, its occurrence reaches 20%, and among patients with hypertension (HTN) and coronary heart disease (CHD) it is much more. Due to the severity of clinical manifestations, paroxysmal SVT occupies a leading place among all cardiac arrhythmias in terms of the frequency of requests for emergency medical care. Frequent and prolonged paroxysms of SVT induce arrhythmogenic myocardial dilatation and systolic chronic heart failure (CHF) [1], contribute to the formation of more complex cardiac arrhythmias [2], and correlate with the risk of developing atrial fibrillation, ischemic stroke and cardiovascular death [3]. For drug therapy of paroxysmal SVT, β-blockers (BABs) are most often used [4]. The rationale for their use is the blockade of the sympathoadrenal system, which is often in a state of pathological hyperactivation [5]. However, in a significant proportion of patients, the use of beta blockers may be limited by their side effects: increased tone of the bronchi and peripheral arteries, decreased physical and mental performance, and erectile dysfunction.
Therapy with certain beta blockers can sometimes be accompanied by a worsening of an existing arrhythmia. Negative chrono-, dromo- and inotropic effects limit the use of beta blockers for bradycardia, atrioventricular block, arterial hypotension, and severe left ventricular (LV) systolic dysfunction [6]. These circumstances justify the choice of drugs that selectively eliminate arrhythmia and do not worsen the functional state of the body.
Assuming a possible multidirectional effect of beta blockers, monitoring the effectiveness of drug therapy should be carried out using sensitive diagnostic methods that determine not only antiarrhythmic and organoprotective effects, but also the functional state of the body as a whole, its ability to regulate and adapt. For an objective quantitative assessment of the regulatory-adaptive status (RAS), a cardiorespiratory synchrony test (CRS) is used, which reflects the interaction of the two most important functions of autonomic support - cardiac and respiratory. The test is based on the close functional connection between the central mechanisms of rhythmogenesis of the heart and respiration, the possibility of voluntary control of the breathing rhythm, and the participation of multi-level afferent and efferent structures of the central nervous system [7].
There is no information in the literature on monitoring the effect of beta blockers on the ASD of patients with paroxysmal SVT. It is possible that their intragroup heterogeneity, mediating different clinical and hemodynamic effects, also has different effects on ASD. Therefore, the selection of optimal beta blockers that effectively suppress SVT paroxysms and have a positive effect on both target organs and the RAS seems relevant.
Purpose of the study
— compare the effectiveness of bisoprolol and sotalol in patients with paroxysmal SVT secondary to hypertension and/or coronary artery disease, taking into account their effect on the RAS.
During pregnancy
Bisoprolol is not recommended for the treatment of pregnant and lactating women. However, in situations where the benefits to the mother potentially outweigh the likely risks to the developing fetus, the drug may still be prescribed.
In exceptional cases, when the medicine is used during pregnancy , it should be discontinued no later than 72 hours before the expected date of birth. Otherwise, there is a high probability of developing hypoglycemia , arterial hypotension , bradycardia , and respiratory depression .
When withdrawal is not possible, constant monitoring of the baby's condition is necessary during the first 72 hours after birth.
If it is necessary to prescribe Bisoprolol to a nursing woman, it is necessary to resolve the issue of stopping lactation .
Material and methods
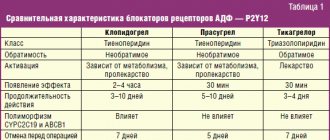
The study involved 60 patients with paroxysmal SVT secondary to stage II–III hypertension and/or coronary artery disease. After randomization (by random sampling), the first group of patients (n=30) was prescribed bisoprolol, the second group (n=30) was prescribed sotalol. The initial dose of bisoprolol was 2.5 mg/day in 1 dose, sotalol - 80 mg/day in 2 doses. Taking into account hemodynamic parameters and individual tolerance, drug doses were titrated at intervals of 2–4 weeks. up to 10 and 320 mg/day, respectively (Table 1).
As part of combination therapy, all patients received lisinopril, and, if indicated, atorvastatin 15.6±5.1 mg/day, n=14, and 14.2±4.6 mg/day, n=15, and acetylsalicylic acid 92 .3±18.8 mg/day, n=15, and 94.8±15.8 mg/day, n=18, or rivaroxaban 20 mg/day, n=3 and n=2, respectively. Treatment adherence was assessed during monthly physician visits.
Inclusion criteria for the study: patient age 30–70 years, presence of paroxysmal SVT against the background of stage II–III hypertension and/or coronary artery disease with preserved LV systolic function (LV ejection fraction (EF) ≥50%), non-use of test drugs within the previous 10 years days, familiarization with the study protocol and written consent to participate in it.
Exclusion criteria: dependence on alcohol and drugs, acute vascular events (cerebral and coronary) during the last year, stage III arterial hypertension, angina pectoris functional class 3-4 (FC), heart rhythm and conduction disorders, CHF FC 3-4 according to the New York Heart Association classification, LV systolic dysfunction, history of cardiac and neurosurgical interventions, respiratory, renal and liver failure, exacerbation of autoimmune diseases, malignant neoplasms, endocrine disorders in the stage of decompensation.
The study was approved by the ethics committee of the State Budgetary Educational Institution of Higher Education "Kuban State Medical University" of the Ministry of Health of the Russian Federation (protocol No. 34 of February 27, 2015).
At the beginning of the study and after 6 months. drug therapy was carried out:
quantitative assessment of ASD using the SDS test with determination of the ASD index (the RAS index is the ratio of the synchronization range (DS) to the duration of development of SDS at the minimum border of SDS×100) [8]. ASD index score: 100 or more – high, 99–50 – good, 49–25 – satisfactory, 24–10 – low, 9 or less – unsatisfactory [9];
ECG in V- and M-modes;
treadmill test using the SHILLER CARDIOVIT CS 200 device (Switzerland) to determine exercise tolerance and identify hidden coronary insufficiency;
six-minute walk test (SMW);
daily monitoring (CM) of blood pressure (BP) in order to determine the daily blood pressure profile, as well as adequate monitoring of the effectiveness of pharmacological therapy;
SM ECG to identify paroxysms of SVT and monitor the effectiveness of therapy;
assessment of quality of life (QOL) using the questionnaire “Quality of life of a patient with arrhythmia” [10].
Statistical processing was carried out using variation statistics methods using the STATISTICA package (version 6.0). Differences were considered statistically significant at p<0.05. Data from only those patients who fully complied with the study protocol were analyzed.
Bisoprolol tablets, instructions for use (Method and dosage)
The dosage of the drug is selected individually. The tablets are taken in the morning, before meals, without chewing. The course of treatment begins by prescribing 0.005 grams to the patient, which is taken once. For patients whose blood pressure is slightly elevated, the starting dose is 0.0025 grams per day.
In cases where this is necessary, the dose is doubled. The dosage regimen remains the same.
The highest daily dose is 0.02 grams; for patients with renal dysfunction , which is characterized by a decrease in creatinine clearance (CC) below 20 ml per minute, the highest dose should be half that (0.01 grams per day).
Exceeding the prescribed average daily dose is allowed in extreme cases. The drug is usually used for a long time.
Elderly patients do not need dose adjustment.
The instructions for use of Bisoprolol-Ratiopharm are identical to the instructions for use of Bisoprolol-Lugal and the instructions for use of Bisoprolol-Teva . Bisoprolol-Prana and other bisoprolol preparations are taken according to the same regimen
Research results
According to the results of the SDS test, the use of therapy with bisoprolol led to an increase in the duration of development of SDS at the minimum limit of the synchronization range (by 20.9%); a decrease in the synchronization range (by 18.8%) and the RAS index (by 46.3%). These changes indicate a decrease in ASD. As a result of taking sotalol, patients experienced a decrease in the synchronization range (by 9.4%) and the RAS index (by 12.7%); there was no significant change in the duration of development of SDS at the minimum border of the synchronization range. Thus, these changes show a less pronounced decrease in RAS when taking sotalol compared to that in the bisoprolol group (Table 2).
According to the results of echocardiography, during the use of therapy with bisoprolol, the peak velocity of the transmitral diastolic flow E (VE) increased (by 7.8%), the ratio of VE and the peak velocity of the transmitral diastolic flow A (VA) (VE/VA) (by 18.2 %), peak velocity of LV base elevation in early diastole (Ve′) (by 21.1%), deceleration time of transmitral diastolic flow E (DTE) (by 25%); the end-diastolic size (EDD) of the LV decreased (by 7.6%), the anteroposterior size of the left atrium (LA) (by 5.6%), the ratio of VE and Ve′ (VE/Ve′) (by 17.6% ), VA (by 12.6%); LVEF, interventricular septal thickness (IVS) and posterior wall thickness (PV) were not subject to significant changes. The listed changes indicate an improvement in the structural and functional parameters of the myocardium. As a result of therapy with sotalol, VE (by 8.4%), VE/VA (by 20%), Ve′ (by 18.5%), DTE (by 31.7%) increased; LV EDV decreased (by 4.6%), LA anteroposterior size (by 2.4%), VA (by 9.7%), VE/Ve′ (by 20.5%); LVEF, LV PV thickness, and IVS thickness did not change significantly. These changes demonstrate regression of cardiac remodeling processes, which is comparable to that under the action of bisoprolol (Table 3). In both groups, LV isovolumetric relaxation time (IVRT) increased comparablely.
According to the results of the treadmill test, during therapy with bisoprolol, the maximum load increased (by 11.9%), and the double product decreased (by 17.1%). During sotalol therapy, the maximum load increased (by 14.6%) and the double product decreased (by 16.3%). Thus, both pharmacological treatment regimens increased exercise capacity to the same extent.
According to the results of TSHM, patients taking bisoprolol as part of combination drug therapy showed an increase in the distance traveled (by 14.5%). In 30% of patients there was a decrease in FC of CHF from II to I, in 8% of cases CHF was not registered. Therapy with sotalol led to an increase in the distance traveled (by 16.3%); in 30% of patients the FC of CHF decreased from II to I, in 10% of cases CHF was not registered. Thus, both regimens of pharmacological therapy comparablely reduced the FC of CHF (Table 4).
According to the BP data, target blood pressure values were achieved in 87% of patients taking bisoprolol and in 83% of those taking sotalol.
According to the results of the SM ECG, the use of bisoprolol as part of combined pharmacological therapy made it possible to achieve a decrease in the average heart rate (HR) (by 18.2%), SVT paroxysms (by 69.1%) and the number of supraventricular extrasystoles (by 62.8%). During therapy with sotalol, the average heart rate (by 21.5%), the number of paroxysms of SVT (by 76.4%) and supraventricular extrasystoles (by 79.3%) decreased. The results obtained demonstrate targeted and comparable antiarrhythmic efficacy of combined pharmacological therapy in both groups.
According to the QOL questionnaire for patients with arrhythmia, the sum of negative scores as a result of therapy using bisoprolol decreased by 33%, and during therapy with sotalol - by 47.5%. Obviously, therapy using sotalol improved the quality of life of patients more significantly than using bisoprolol (Table 5).
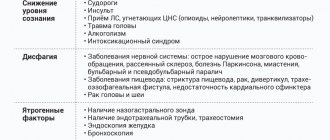
When using bisoprolol as part of combination pharmacotherapy, side effects occurred in 13% of cases: erectile dysfunction (n=1), dry cough (n=1), drowsiness (n=1), dyspepsia (n=1). During therapy with sotalol, side effects were observed in 17% of cases: dry cough (n=2), drowsiness (n=2), dyspepsia (n=1). These manifestations were mild and transient in nature, which did not require exclusion of patients from the study or discontinuation of therapy.
The discussion of the results
Currently, the position of beta blockers as first-line drugs for a number of cardiac diseases is being reasonably reconsidered [11]. Modern representatives of this group of drugs must meet a number of requirements: have high cardioselectivity, optimal anti-ischemic, antihypertensive and antiarrhythmic properties, and satisfactory tolerability. However, their impact on the RAS, which objectively quantitatively reflects the functional state of the body, can be ambiguous. A number of clinical studies have proven the sensitivity of the method for assessing RAS, including in patients suffering from cardiovascular diseases. The data obtained as a result of the study turned out to be comparable with the results of generally accepted laboratory and instrumental examination methods [12, 13].
Bisporolol is a hydrolipophilic cardioselective beta blocker without internal sympathomimetic and membrane-stabilizing activity. Due to its selective action, bisoprolol reduces the rate of spontaneous depolarization of the sinus node and ectopic pacemakers, as a result of which it suppresses their excitability. In addition, the action of bisoprolol inhibits re-entry
, and also helps to reduce pacemaker automatism. In the MIRSA, BISOMET, BIMS, TIBBS projects, bisoprolol demonstrated a decrease in overall mortality and the incidence of acute coronary events in patients with hypertension and coronary artery disease, a decrease in cardiac remodeling in CHF, and a sufficient hypotensive effect [14].
Sotalol is a hydrophilic non-cardioselective beta blocker that has the properties of class III antiarrhythmic drugs. The antiarrhythmic effect of sotalol is to lengthen the repolarization phase and action potential of cardiomyocytes. Like all representatives of the beta blocker group, sotalol is capable of reducing myocardial oxygen demand. In studies such as ESVEM, AVID, VT-MASS, Brazilian multicenter study of sotalol effectiveness in ventricular arrhythmias, in patients with hypertension and coronary artery disease, prevention of the induction of sustained ventricular tachycardia, suppression of supraventricular arrhythmias, as well as effective control of arterial hypertension while taking sotalol, but there was no significant reduction in the risk of sudden cardiac death [15].
As a result of our study, bisoprolol therapy showed positive dynamics of myocardial remodeling processes, optimization of blood pressure during the day, targeted antiarrhythmic effect, increased tolerance to physical activity, which led to an improvement in quality of life, but was accompanied by a decrease in RAS. Probably, this phenomenon can be caused, on the one hand, by sufficient suppression of arrhythmia, and on the other, by inhibition of the sympathetic division of the autonomic nervous system. Patients randomized to the sotalol group experienced comparable antiarrhythmic, hemodynamic, and organoprotective effects. However, when treated with sotalol, a less pronounced negative effect on the RAS and a more pronounced improvement in QoL were recorded. It is possible that the inhibitory sympathotropic effects of sotalol are partially offset by its additional antiarrhythmic properties and the absence of a direct effect on the central nervous system.
conclusions
Regimens using bisoprolol or sotalol as part of combination pharmacological therapy had an equally positive effect on target organs, comparable increased exercise tolerance, and had antiarrhythmic and hypotensive effects.
Sotalol, in comparison with bisoprolol, reduces RAS less and improves quality of life more significantly.
Taking into account the less pronounced negative effect of sotalol on the RAS in patients suffering from a paroxysmal form of SVT against the background of stage II–III hypertension and/or coronary artery disease, its use may be preferable to bisoprolol.
Interaction
Inadmissible combinations with Bisoprolol:
- Floctafenine;
- Sultopride.
Not recommended combinations:
- with calcium antagonists;
- with antihypertensive drugs , which are characterized by a central mechanism of action;
- with MAO inhibitors (except for MAO-B inhibitors).
The drug is prescribed with caution with:
- antiarrhythmic drugs class I and III;
- calcium antagonists , which belong to the group of dihydropyridine derivatives ;
- anticholinesterase drugs;
- Local β-blockers;
- insulin preparations and oral antidiabetic agents ;
- cardiac glycosides (digitalis preparations);
- anesthetics;
- non-steroidal anti-inflammatory drugs;
- ergotamine derivatives;
- β-sympathomimetics;
- sympathomimetics, which are characterized by the ability to activate α- and β-adrenergic receptors ;
- antihypertensive drugs that increase the risk of hypotension (for example, tricyclic antidepressants , phenothiazines or barbiturates );
- Baclofen;
- Amifostin;
- parasympathomimetics.
Allowed combinations:
- mefloquine;
- corticosteroid drugs.