Pharmacodynamics and pharmacokinetics
Biprol is a selective beta1-blocker that does not have internal sympathomimetic activity and membrane-stabilizing properties.
When taking this drug, the activity of renin in plasma decreases, the need for oxygen supply to the myocardium, and heart rate in various states decreases. This indicates that the drug has hypotensive, antiarrhythmic and antianginal effects. Low doses of Biprol can block β1-adrenergic receptors of the heart, reduce catecholamine- calcium current , reduce myocardial contractility, inhibit conductivity and excitability, and so on. When the drug is prescribed in high doses, its beta2-adrenergic blocking effect is noted.
The hypotensive effect of this medicine allows you to reduce minute volume of blood, sympathetic stimulation of peripheral vessels, reduce the activity of the renin-angiotensin-aldosterone system, helps restore sensitivity while lowering blood pressure and affecting the central nervous system. During the treatment of arterial hypertension, initial effectiveness appears after 2-5 days, and a stable effect lasts 1-2 months.
The antianginal effect of the drug helps reduce the need for oxygen supply to the myocardium, due to a decrease in heart rate and contractility, prolongation of diastole and improvement of myocardial perfusion.
The manifestation of the antiarrhythmic effect is associated with the elimination of arrhythmogenic factors, a decrease in the rate of spontaneous excitation, and so on.
Taking Biprol in medium therapeutic doses has a less pronounced effect on organs that contain β2-adrenergic receptors, for example: pancreas , skeletal muscles, smooth muscles of peripheral arteries, uterus and bronchi, as well as on carbohydrate metabolism, and does not retain sodium in the body.
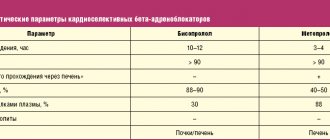
Internal administration of the drug is accompanied by good absorption from the gastrointestinal tract, amounting to 80-90%. However, food does not affect this process. The maximum concentration of the active substance in the blood plasma is detected after 1-3 hours. The connection with blood plasma proteins reaches almost 30%. It has been noted that a small amount of the substance penetrates into breast milk, through the placental barrier and the BBB. metabolic process primarily occurs in the liver. Excretion is carried out through the kidneys, a small part through bile.
Biprol
Monitoring of patients taking the drug should include monitoring heart rate and blood pressure (daily at the beginning of treatment, then once every 3-4 months), ECG, and blood glucose levels in patients with diabetes (once every 4-5 months). In elderly patients, it is recommended to monitor renal function (once every 4-5 months). After starting treatment for CHF at a dose of 1.25 mg, the patient should be examined within 4 hours (heart rate, blood pressure, ECG).
The patient should be taught how to calculate heart rate and instructed about the need for medical consultation if the heart rate is less than 50/min.
Before starting treatment with the drug, it is recommended to conduct a study of external respiratory function in patients with a burdened bronchopulmonary history.
In approximately 20% of patients with angina, beta blockers are ineffective. The main causes are severe coronary atherosclerosis with a low ischemic threshold (heart rate less than 100/min) and increased LV EDV, which impairs subendocardial blood flow. In smokers, the effectiveness of beta-blockers is lower.
Patients who use contact lenses should take into account that during treatment with the drug there may be a decrease in the production of tear fluid.
When used in patients with pheochromocytoma, there is a risk of developing paradoxical arterial hypertension (if effective alpha-blockade is not previously achieved).
In case of thyrotoxicosis, the drug may mask certain clinical signs of thyrotoxicosis (for example, tachycardia). Abrupt withdrawal in patients with thyrotoxicosis is contraindicated because it can increase symptoms.
In diabetes mellitus, it can mask tachycardia caused by hypoglycemia. Unlike non-selective beta-blockers, it practically does not enhance insulin-induced hypoglycemia and does not delay the restoration of blood glucose to normal levels.
When taking clonidine concomitantly, it can be discontinued only a few days after discontinuation of the drug.
It is possible that the severity of the hypersensitivity reaction may increase and the absence of effect from usual doses of epinephrine against the background of a burdened allergic history.
If planned surgical treatment is necessary, the drug should be discontinued 48 hours before the start of general anesthesia. If the patient took the drug before surgery, he should select a drug for general anesthesia with minimal negative inotropic effect.
Reciprocal activation of the n.vagus can be eliminated by intravenous administration of atropine (1-2 mg).
Drugs that reduce catecholamine reserves (for example, reserpine) can enhance the effect of beta-blockers, so patients taking such combinations of drugs should be under constant medical supervision to detect arterial hypotension or bradycardia.
Patients with bronchospastic diseases can be prescribed cardioselective adrenergic blockers in case of intolerance and/or ineffectiveness of other antihypertensive drugs, but the dosage of the drug should be strictly monitored. An overdose is dangerous due to the development of bronchospasm.
If elderly patients develop increasing bradycardia (less than 50/min), arterial hypotension (systolic blood pressure below 100 mm Hg), AV block, bronchospasm, ventricular arrhythmias, severe liver and kidney dysfunction, it is necessary to reduce the dose or stop treatment . It is recommended to discontinue therapy if depression caused by taking beta-blockers develops.
Treatment with the drug should not be abruptly interrupted due to the risk of developing severe arrhythmias and myocardial infarction. Cancellation is carried out gradually, reducing the dose over 2 weeks or more (reduce the dose by 25% in 3-4 days).
The use of the drug during pregnancy and lactation is possible if the benefit to the mother outweighs the risk of side effects in the fetus and child.
Should be discontinued before testing the content of catecholamines, normetanephrine and vanillylmandelic acid in the blood and urine; antinuclear antibody titers.
During treatment with the drug, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Contraindications for use
The drug is not prescribed for:
- shock, for example, cardiogenic;
- collapse;
- edema ;
- acute and chronic heart failure;
- AV blockade II and III degrees;
- severe bradycardia;
- under 18 years of age;
- sinoatrial block;
- sick sinus syndrome;
- Prinzmetal's angina;
- arterial hypotension;
- bronchial asthma and chronic pulmonary obstruction;
- lactation, pregnancy and so on.
Biprol 2.5 mg (tablets)
Termination of therapy and “withdrawal syndrome”
You should not abruptly interrupt treatment with bisoprolol or change the recommended dose without first consulting your doctor, as this may lead to a temporary deterioration in heart function. Treatment should not be interrupted suddenly, especially in patients with coronary artery disease (increased severity of angina attacks, the development of myocardial infarction and the occurrence of ventricular arrhythmias in patients with coronary artery disease with sudden cessation of beta-blockers have been noted). If discontinuation of treatment is necessary, the dose of bisoprolol should be reduced gradually. In case of significant worsening of angina or development of acute coronary syndrome, bisoprolol should be temporarily resumed.
Diseases for which the drug should be used with caution
Bisoprolol should be used with caution in the following cases:
- severe forms of COPD and non-severe forms of bronchial asthma;
- diabetes mellitus with significant fluctuations in blood glucose concentrations: bisoprolol may mask symptoms of hypoglycemia (a marked decrease in blood glucose concentrations), such as tachycardia, palpitations or increased sweating;
- strict diet;
- carrying out desensitizing therapy;
- atrioventricular block of the first degree;
- vasospastic angina (Prinzmetal's angina); cases of coronary spasm have been observed. Despite its high beta1 selectivity, angina attacks cannot be completely excluded when taking bisoprolol in patients with Prinzmetal's angina. You should take the drug with extreme caution;
- mild to moderate peripheral arterial circulatory disorders (increased symptoms may occur at the beginning of therapy);
- psoriasis (including history).
Diseases of the cardiovascular system
Beta blockers should not be used in decompensated chronic heart failure until the patient's condition has stabilized. At the initial stages of using bisoprolol, patients need constant monitoring.
Beta blockers may cause bradycardia. If the resting heart rate decreases to less than 50-55 beats/min, the dose should be reduced or discontinued taking bisoprolol.
Like other beta blockers, bisoprolol may cause a prolongation of the PQ interval on the ECG. Bisoprolol should be used with caution in patients with first degree atrioventricular block.
Non-selective beta-blockers may increase the frequency and duration of anginal attacks in patients with vasospastic angina (Prinzmetal's angina) due to alpha-receptor-mediated coronary artery vasoconstriction. Cardioselective beta-blockers (including bisoprolol) should be used with caution in vasospastic angina.
To date, there is insufficient data regarding the use of bisoprolol in patients with CHF in combination with type 1 diabetes mellitus, severe renal and/or liver dysfunction, restrictive cardiomyopathy, congenital heart defects or heart valve disease with severe hemodynamic disturbances.
Also, sufficient data have not yet been obtained regarding patients with CHF with myocardial infarction within the last 3 months.
Respiratory system
Despite the fact that selective beta-blockers have a lesser effect on the function of the respiratory system than non-selective beta-blockers, patients with chronic obstructive pulmonary disease (COPD) and mild forms of bronchial asthma should be prescribed bisoprolol with extreme caution and only if if the possible benefits of its use outweigh the potential risks. For bronchial asthma or COPD, simultaneous use of bronchodilators is indicated.
In patients with bronchial asthma, there may be an increase in airway resistance, which requires a higher dose of beta2-agonists.
In patients with COPD, therapy with bisoprolol prescribed in combination therapy for the treatment of heart failure should be initiated at the lowest possible dose, and patients should be carefully monitored for the development of new symptoms (eg, shortness of breath, exercise intolerance, cough).
Major surgery and general anesthesia
If surgical interventions are necessary, the anesthesiologist should be warned that the patient is taking beta-blockers (risk of drug interactions with the development of severe bradyarrhythmias, reduction of reflex tachycardia and arterial hypotension). It is recommended not to stop taking bisoprolol in the perioperative period unless clearly necessary (since beta-adrenergic receptor blockade reduces the risk of arrhythmias and myocardial ischemia during induction of anesthesia and tracheal intubation). If it is necessary to interrupt treatment with bisoprolol before surgery, the drug should be discontinued at least 48 hours before surgery.
Pheochromocytoma
In patients with pheochromocytoma, bisoprolol can only be prescribed while using alpha-blockers.
Thyrotoxicosis
With hyperthyroidism, beta-blockers (including bisoprolol) can mask tachycardia and reduce the severity of symptoms of thyrotoxicosis.
Abrupt withdrawal of the drug can cause exacerbation of symptoms of the disease and the development of thyrotoxic crisis.
Hypersensitivity reactions
Beta blockers, including bisoprolol, may increase sensitivity to allergens and the severity of anaphylactic/hypersensitivity reactions due to decreased adrenergic compensatory regulation by beta blockers. The use of usual therapeutic doses of epinephrine (adrenaline) while taking beta-blockers does not always lead to achieving the desired clinical effect.
Caution should be exercised when prescribing bisoprolol to patients with a history of severe hypersensitivity reactions or undergoing desensitization.
Psoriasis
When deciding on the use of bisoprolol in patients with psoriasis, the expected benefits of the drug should be carefully weighed against the possible risk of exacerbation of psoriasis.
Contact lenses
Patients who use contact lenses should take into account that the use of beta-blockers may reduce the production of tear fluid.
Special conditions
When treating with Biprol, it is necessary to regularly monitor the patient's condition by measuring heart rate and blood pressure, performing an ECG, and determining blood glucose levels - for patients with diabetes . Elderly patients should monitor their kidney function. In addition, when starting treatment, it is necessary to examine the functions of external respiration if patients have disorders of the respiratory system.
It has been established that in smoking patients the effect of beta-blockers is reduced.
When using contact lenses, you need to remember that during the treatment period there may be a reduction in the production of tear fluid.
Treatment of patients with other complicated forms of chronic diseases should be carried out with caution, since the manifestation of some undesirable symptoms is often disguised as others. For example, in diabetes mellitus of tachycardia caused by hypoglycemia is not excluded .
When it is necessary to perform an operation using general anesthesia, the drug is discontinued 48 hours before the scheduled procedure. Also, treatment with Biprol is stopped if a depressive state develops.
However, abruptly stopping treatment is contraindicated, as severe arrhythmias or myocardial infarction . Therefore, withdrawal is carried out gradually, with a reduction in dosage over 2 weeks.
During treatment, care should be taken when driving any type of transport or engaging in other dangerous activities that require special attention and quick response.
Biprol 5 mg, 10 mg (tablets)
Termination of therapy and withdrawal syndrome
You should not abruptly interrupt treatment with bisoprolol or change the recommended dose without first consulting your doctor, as this may lead to a temporary deterioration in heart function.
Treatment should not be interrupted suddenly, especially in patients with coronary artery disease (increased severity of angina attacks, the development of myocardial infarction and the occurrence of ventricular arrhythmias in patients with coronary artery disease with sudden cessation of beta-blockers have been noted). If discontinuation of treatment is necessary, the dose of bisoprolol should be reduced gradually. In case of significant worsening of angina or development of acute coronary syndrome, bisoprolol should be temporarily resumed.
Diseases for which the drug should be used with caution
Bisoprolol should be used with caution in the following cases:
- severe forms of COPD and non-severe forms of bronchial asthma;
- diabetes mellitus with significant fluctuations in blood glucose concentrations: bisoprolol may mask symptoms of hypoglycemia (a marked decrease in blood glucose concentrations), such as tachycardia, palpitations or increased sweating;
- strict diet;
- carrying out desensitizing therapy;
- atrioventricular block of the first degree;
- Vasospastic angina (Prinzmetal's angina): cases of coronary spasm have been observed. Despite its high beta1 selectivity, angina attacks cannot be completely excluded when taking bisoprolol in patients with Prinzmetal's angina. You should take the drug with extreme caution;
- mild to moderate peripheral arterial circulatory disorders (increased symptoms may occur at the beginning of therapy);
- psoriasis (including history).
Diseases of the cardiovascular system
Beta blockers should not be used in decompensated chronic heart failure until the patient's condition has stabilized.
At the initial stages of using bisoprolol, patients need constant monitoring.
Beta blockers may cause bradycardia. If the resting heart rate decreases to less than 50-55 beats/min, the dose should be reduced or discontinued taking bisoprolol.
Like other beta blockers, bisoprolol may cause a prolongation of the PQ interval on the ECG. Bisoprolol should be used with caution in patients with first degree atrioventricular block.
Non-selective beta-blockers may increase the frequency and duration of anginal attacks in patients with vasospastic angina (Prinzmetal's angina) due to alpha-receptor-mediated coronary artery vasoconstriction. Cardioselective beta1-blockers (including bisoprolol) should be used with caution in vasospastic angina.
To date, there is insufficient data regarding the use of bisoprolol in patients with CHF in combination with type 1 diabetes mellitus, severe renal and/or liver dysfunction, restrictive cardiomyopathy, congenital heart defects or heart valve disease with severe hemodynamic disturbances. Also, sufficient data have not yet been obtained regarding patients with CHF with myocardial infarction within the last 3 months.
Respiratory system
Despite the fact that selective beta1-blockers have a lesser effect on the function of the respiratory system than non-selective beta-blockers, patients with chronic obstructive pulmonary disease (COPD) and mild forms of bronchial asthma should be prescribed bisoprolol with extreme caution and only if if the possible benefits of its use outweigh the potential risks. For bronchial asthma or COPD, simultaneous use of bronchodilators is indicated. In patients with bronchial asthma, there may be an increase in airway resistance, which requires a higher dose of beta2-agonists.
In patients with COPD, bisoprolol prescribed in combination therapy for the treatment of heart failure should be started at the lowest possible dose, and patients should be carefully monitored for the development of new symptoms (eg, shortness of breath, exercise intolerance, cough).
Major surgery and general anesthesia
If surgical interventions are necessary, the anesthesiologist should be warned that the patient is taking beta-blockers (risk of drug interactions with the development of severe bradyarrhythmias, reduction of reflex tachycardia and arterial hypotension). It is recommended not to stop taking bisoprolol in the perioperative period unless clearly necessary (since blockade of beta-adrenergic receptors reduces the risk of arrhythmias and myocardial ischemia during induction of anesthesia and tracheal intubation).
If it is necessary to interrupt treatment with bisoprolol before surgery, the drug should be discontinued at least 48 hours before surgery.
Pheochromocytoma
In patients with pheochromocytoma, bisoprolol can only be prescribed while using alpha-blockers.
Thyrotoxicosis
With hyperthyroidism, beta-blockers (including bisoprolol) can mask tachycardia and reduce the severity of symptoms of thyrotoxicosis. Abrupt withdrawal of the drug can cause exacerbation of symptoms of the disease and the development of thyrotoxic crisis.
Hypersensitivity reactions
Beta blockers, including bisoprolol, may increase sensitivity to allergens and the severity of anaphylactic/hypersensitivity reactions due to decreased adrenergic compensatory regulation by beta blockers. The use of usual therapeutic doses of epinephrine (adrenaline) while taking beta-blockers does not always lead to achieving the desired clinical effect. Caution should be exercised when prescribing bisoprolol to patients with a history of severe hypersensitivity reactions or undergoing desensitization.
Psoriasis
When deciding on the use of bisoprolol in patients with psoriasis, the expected benefits of the drug should be carefully weighed against the possible risk of exacerbation of psoriasis.
Contact lenses
Patients who use contact lenses should take into account that the use of beta-blockers may reduce the production of tear fluid.
Side effects
When treated with Biprol, undesirable effects may develop that affect the activity of the nervous, cardiovascular, digestive, respiratory and other systems. In this case, the following manifestations are possible: increased fatigue, weakness, dizziness and headache , sleep disorders, depression, anxiety, confusion, asthenia and tremor .
There is still a possibility of developing: changes in heartbeat, myocardial conduction disturbances, arrhythmias , chronic heart failure, low blood pressure, nausea, vomiting, problems with stool, pain in the gastrointestinal tract, breathing problems, and so on.
Deviations in the functioning of the visual organs, the occurrence of allergic and dermatological reactions, as well as general disorders are not excluded.
Biprol, instructions for use (Method and dosage)
According to the instructions for use of Biprol, you need to take the medicine orally, once a day, preferably in the morning, with liquid.
The tablets are taken as a whole. The dosage is selected by a doctor and depends on the characteristics of the patient, taking into account his heart rate and blood pressure.
For example, for arterial hypertension and coronary heart disease, a single daily dose of 5 mg is prescribed. If necessary, the dose is gradually increased to 10 mg. The therapeutic dosage for patients suffering from arterial hypertension or angina pectoris may be 20 mg, taken once a day.
Biprol, 50 pcs., 5 mg, film-coated tablets
Common to all dosages
Inside,
in the morning, 1 time per day with a small amount of liquid, before, during or after breakfast. The tablets should not be chewed or crushed into powder.
For film-coated tablets, 2.5 mg
Preconditions for starting treatment with Biprol are stable CHF without signs of exacerbation for 6 weeks; treatment with optimal doses of drugs for standard therapy of CHF; no changes in standard therapy for CHF in the previous 2 weeks. Initiation of treatment with Biprol requires a special titration phase and regular medical supervision.
Titration phase
The recommended starting dose of Biprol is 1.25 mg (1/2 tablet of 2.5 mg each) 1 time per day. Depending on individual tolerance, the dose should be gradually increased to 2.5; 3.75; 5; 7.5; and 10 mg 1 time per day. Each subsequent dose increase should be carried out at intervals of at least 2 weeks. If increasing the dose of the drug is poorly tolerated by the patient, a dose reduction may be possible. The maximum recommended (target) dose of Biprol for CHF is 10 mg once a day.
During the titration phase, regular monitoring of heart rate, blood pressure and signs of worsening CHF, which can develop from the first day of drug use, is necessary.
After taking the initial dose of 1.25 mg (1/2 tablet of 2.5 mg), the patient should be observed for 4 hours (monitoring heart rate, blood pressure, conduction disturbances, signs of worsening heart failure); if necessary, the drug is discontinued.
Each dose increase should be carried out only if the previous dose is well tolerated and the patient's condition is stable. In case of questionable tolerability and excessive decrease in blood pressure, the dose is increased once every 4 weeks; in this case, the target dose can be achieved by the 24th week. If the target dose cannot be achieved, the patient should receive the maximum tolerated dose.
During titration or maintenance therapy, temporary worsening of heart failure, hypotension, or bradycardia may occur. In these cases, it is recommended to first adjust the doses of concomitant therapy (diuretic and/or ACE inhibitor); if this measure is ineffective, a temporary reduction, slower dose titration, or discontinuation of the Biprol drug may be required. Resumption of therapy and/or dose titration of Biprol should be considered only after the patient's condition has stabilized.
You should not suddenly stop taking Biprol (as well as any beta-blocker), since withdrawal syndrome may develop, which manifests itself as signs of decompensation of CHF. Therefore, discontinuation and reduction of the dose of Biprol should be carried out gradually, under the supervision of a physician, taking into account the individual reactions of the patient (see “Special Instructions”).
If you miss the next dose of the drug, you should not double the next dose.
Duration of treatment.
The drug Biprol is usually prescribed for long-term therapy, the duration of which is determined by the doctor.
Special patient groups
Impaired kidney or liver function.
For mild or moderate renal or hepatic impairment, no dose adjustment is required. In severe renal impairment (creatinine Cl less than 20 ml/min) and in patients with severe liver disease, dose titration is carried out with extreme caution; The maximum daily dose of Biprol is 10 mg.
Elderly patients.
No dose adjustment is required.
Children.
Due to insufficient data, the use of Biprol in children under 18 years of age is not recommended.
Patients with concomitant diseases.
Currently, there is insufficient data regarding the use of bisoprolol in patients with CHF in combination with type 1 diabetes mellitus, severe renal and/or liver dysfunction, restrictive cardiomyopathy, congenital heart defects or heart valve defects with severe hemodynamic disturbances, myocardial infarction within the last 3 years months
For film-coated tablets, 5 and 10 mg
In all cases, the doctor selects the dosage regimen and dose individually for each patient, in particular taking into account the heart rate and condition of the patient.
For arterial hypertension and coronary artery disease, the drug is prescribed 5 mg once a day. If necessary, the dose is increased to 10 mg 1 time per day. In the treatment of arterial hypertension and angina pectoris, the maximum daily dose is 20 mg 1 time per day.
Renal dysfunction.
For patients with impaired renal function (Cl creatinine <20 ml/min) or severe impaired liver function, the maximum daily dose is 10 mg 1 time per day. Increasing the dose in such patients must be carried out with extreme caution.
Elderly patients.
No dose adjustment is required.
Interaction
Simultaneous therapy with Biprol and the use of allergens can cause severe systemic allergic reactions or anaphylaxis.
Combination with iodine-containing radiocontrast drugs increases the risk of anaphylactic reactions.
Phenytoin and general anesthesia drugs increase the severity of the cardiodepressive effect and the likelihood of a decrease in blood pressure.
In addition, Biprol can change the effectiveness of insulin and other oral hypoglycemic drugs, masking the symptoms of hypoglycemia in the form of tachycardia or increased blood pressure.
Combination therapy with cardiac glycosides, methyldopa , reserpine and guanfacine, verapamil, diltiazem, amiodorone can lead to the development or aggravate bradycardia, AV block, cardiac arrest and heart failure.
Nifedipine, diuretics, clonidine, hydralazine, sympatholytics and other antihypertensive drugs can significantly reduce blood pressure.
You should refrain from simultaneous use of bisoprolol and MAO inhibitors , as this significantly enhances the hypotensive effect. Typically, an interval of 14 days is maintained between therapeutic courses of these drugs.
Biprol
The effectiveness and tolerability of bisoprolol may be affected by other medications taken at the same time. Such an interaction is also possible when two drugs are taken after a short period of time. It is necessary to inform your doctor about other medications you are taking, even if you are taking them without a prescription (over-the-counter medications).
Floctafenine.
In case of shock or arterial hypotension caused by floctafenine, beta-blockers cause a decrease in compensatory cardiovascular reactions (joint use is contraindicated).
Sultopride.
Due to the additive effect, severe bradycardia may develop; high risk of ventricular arrhythmias (combined use is contraindicated).
MAO inhibitors.
Concomitant use is not recommended (with the exception of MAO type B inhibitors), since there is a high probability of a significant increase in the antihypertensive effect. The treatment break between taking MAO inhibitors and bisoprolol should be at least 14 days.
Slow calcium channel blockers: verapamil and, to a lesser extent,
diltiazem
. Due to the synergistic effect, when used together with bisoprolol, AV conduction may slow down and myocardial contractility may decrease (this combination should be avoided).
During treatment with Biprol, intravenous administration of verapamil or diltiazem and other antiarrhythmic drugs is contraindicated (risk of developing asystole, high-degree AV block, severe bradycardia, severe arterial hypotension, increased heart failure).
Centrally acting antihypertensives
(eg clonidine, apraclonidine, alpha-methyldopa, moxonidine, rilmenidine). Concomitant use with bisoprolol is not recommended. Due to the synergism of action and inhibition of sympathetic compensatory mechanisms, the risk of developing severe bradycardia, sinus node arrest, impaired AV conduction, a pronounced decrease in blood pressure, and a decrease in cardiac output increases. Abrupt withdrawal, especially before discontinuation of bisoprolol, increases the risk of developing “rebound” arterial hypertension (see section “Special Instructions”).
Class I antiarrhythmic drugs
(for example, quinidine, disopyramide, lidocaine, phenytoin, flecainide, propafenone), when used together with bisoprolol, reduce AV conduction and increase the negative inotropic effect (strict clinical and electrocardiographic monitoring is required).
Class III antiarrhythmic drugs
(eg amiodarone). Possible increased negative impact on AV conduction.
Blockers of "slow" calcium channels - dihydropyridine derivatives
(eg nifedipine, felodipine, amlodipine). The risk of a pronounced decrease in blood pressure and increased heart failure increases.
Parasympathomimetics.
AV conduction disturbances may increase and the risk of bradycardia may increase.
Beta blockers for topical use
(for example, eye drops for the treatment of glaucoma) may enhance the systemic effect of bisoprolol (lowering blood pressure, lowering heart rate).
Insulin and hypoglycemic agents for oral administration
. When used together, the hypoglycemic effect may be enhanced. Signs of hypoglycemia, in particular tachycardia, may be masked or suppressed. This interaction is more typical for non-selective beta-blockers.
Agents for inhalation general anesthesia, hydrocarbon derivatives
(for example, chloroform, cyclopropane, halothane, methoxyflurane) increase the severity of the cardiodepressive effect and the likelihood of arterial hypotension (see section "Special Instructions").
Cardiac glycosides.
Increased risk of developing bradycardia, prolongation of AV conduction time.
Nonsteroidal anti-inflammatory drugs
(due to sodium ion retention and blockade of prostaglandin synthesis by the kidneys),
glucocorticosteroids and estrogens
(due to sodium ion retention) weaken the antihypertensive effect of bisoprolol.
Beta-agonists
(eg, isoprenaline, dobutamine). The effect of both drugs may be weakened.
Adrenomimetics affecting beta and alpha adrenergic receptors
(eg, norepinephrine, epinephrine). It is possible to enhance the vasoconstrictor effects of these drugs, which occur with the participation of alpha-adrenergic receptors, with an increase in blood pressure. Such interactions are more likely with non-selective beta-blockers.
Diuretics, sympatholytics, hydralazine, other drugs with a potential effect on blood pressure
. When used together, an excessive decrease in blood pressure is possible.
Tricyclic and tetracyclic antidepressants, sedatives, hypnotics and antipsychotic drugs (neuroleptics),
ethanol
. When used together, an excessive decrease in blood pressure and increased depression of the central nervous system is possible.
Mefloquine
. The risk of developing bradycardia increases (additive effect).
Sympathomimetics, xanthines (aminophylline, theophylline)
. Mutual weakening of therapeutic effects is possible.
Baclofen
. The risk of arterial hypotension increases.
Non-hydrogenated ergot alkaloids, ergotamine
increase the risk of developing peripheral circulatory disorders.
Sulfasalazine
increases the concentration of bisoprolol in the blood plasma.
Rifampicin
shortens the half-life of bisoprolol (clinically insignificant).
Allergens used for immunotherapy or
allergen extracts
for skin testing may provoke severe systemic allergic reactions in patients receiving bisoprolol (see section "Precautions").
Iodine-containing radiopaque diagnostic agents
for intravenous administration increase the risk of developing anaphylactic reactions refractory to treatment. Bisoprolol prolongs the effect of non-depolarizing muscle relaxants and the anticoagulant effect of coumarins.
Biprol's analogs
Level 4 ATC code matches:
Biol
Metocard
Metozok
Nebilet
Nebilong
Betaxolol
Bisogamma
Aritel
Cordinorm
Vasocardin
Corvitol
Bidop
Bisoprolol
Nebivolol
Bisoprol
Concor Cor
Lokren
Concor
Niperten
Betaloc ZOK
The main analogues of this drug: Aritel, Bidop, Bisogamma, Bisoprol, Concor, Cordinorm, Coronal, Niperten and Tirez .
Reviews of Biprol
As reviews of Biprol show, when prescribing this medicine, many patients are frightened by the list of possible side effects. Therefore, often, after studying the instructions, people believe that this is not only a medicinal, but also a very dangerous remedy, which makes the pills simply forbidden for them.
However, the majority of patients who have already been treated with Biprol report its good tolerability combined with high efficiency. Moreover, for some patients this drug is better suited than, for example, the original Concor .
Experts express a similar opinion about this drug. Many of them often prescribe Biprol to their patients. As clinical practice shows, side effects during treatment with these tablets develop in isolated cases and usually they manifest themselves only as headaches.
Biprol is one of the most popular and highly effective drugs. If taken correctly, the treatment brings a stable and long-lasting effect. The main thing is that the therapy should be prescribed by a doctor who can evaluate its effectiveness.
Biprol price, where to buy
The price of Biprol 10 mg for 30 pieces in a package in Moscow pharmacies is 125-160 rubles.
You can buy 5 mg tablets for 30 pieces in a pack within the range of 67-85 rubles.
- Online pharmacies in RussiaRussia
- Online pharmacies in KazakhstanKazakhstan
ZdravCity
- Biprol tab.
p.p.o. 5 mg n100 Hemofarm LLC, Russia RUB 288 order - Biprol tablets p.p.o. 10 mg 30 pcs. LLC HEMOFARM
164 RUR order
- Biprol tablets p.p.o. 5 mg 30 pcs. LLC HEMOFARM
105 rub. order
- Biprol tablets p.p.o. 5 mg 50 pcs. Hemofarm LLC, Russia
RUB 143 order
- Biprol tablets p.p.o. 2.5 mg 30 pcs. Hemofarm LLC
105 rub. order
Pharmacy Dialogue
- Biprol tablets 5 mg No. 50 Hemofarm LLC
RUB 142 order
- Biprol (tab.p.pl/vol. 10 mg No. 30) Hemofarm LLC
160 rub. order
- Biprol (tab.p.pl.vol. 10 mg No. 30) Hemofarm LLC
RUB 168 order
- Biprol (tab.p.pl.vol.5mg No. 50) Hemofarm LLC
RUB 143 order
- Biprol (tab.p.pl.vol.5mg No. 30) Hemofarm LLC
109 rub. order
show more