One of the most accessible and effective types of examination in medicine is a general blood test. It is the most common and is prescribed in almost all cases of visiting a general practitioner. Changes in the composition of the blood make it possible to suspect the development of many diseases at the initial stage, as well as to establish the causes of certain symptoms. During a clinical analysis, the parameters of all blood cells are assessed. Today there are more than 20 important indicators, among which is PDW. This is one of the platelet blood indices. The meaning of the abbreviation is the width of the distribution of platelets by their volume. This indicator reflects the heterogeneity of the population of blood platelets in size and reflects the degree of anazocytosis - changes in cell size. That is, the platelets in the blood differ in size from each other, and the PDW analysis shows what percentage of the total number are micro- and macroplatelets.
Treatment
Hospitalization of the baby is necessary only in the most extreme cases. If the cause is not oncology, treatment is carried out using conservative methods:
- nutrition correction;
- taking medications;
- compliance with the daily routine.
The medicinal part of treatment may include drugs with the following spectrum of action:
- for blood thinning;
- to reduce platelet production;
- non-steroidal anti-inflammatory drugs;
- vitamin and mineral complexes.
Be sure to exclude from your diet foods that produce this blood component. You should add foods that are rich in vitamin B6 and magnesium to your menu. It is necessary to monitor the drinking regime - the child should be given clean water, herbal decoctions, juices and compotes.
Decoding
Many people ask what PDW is in a blood test and who interprets the test. The doctor must decipher the PDW blood test. PDW may be normal, elevated, or decreased. A normal index occurs when the number of old and young cells is the same. This index occurs in healthy people. If the indicator is elevated, then their number has sharply increased, and a large number of young and old cells are contained. This happens with bone marrow pathologies or other diseases.
An increased value of the indicator is determined in cancer, iron deficiency, and inflammatory processes. This result occurs with infectious diseases or when the patient uses hormonal drugs. A decreased PDW indicates that there are more old particles, which may indicate bone marrow disease, viral diseases, or certain medications.
When doctors decipher the result, sometimes the study shows that a person has too large platelets, which indicates the presence of disturbances in the functioning of the immune system or Bernard-Soulier disease.
Norm
The normal PDW in adults is 15-17%. The breadth of platelet population distribution in children under 18 years of age is 10-15%. If there is a deviation from the norm, the doctor considers the possibility of dysfunction of organs or systems. This indicates some kind of disease.
Increased level
An increase in the indicator indicates heterogeneity in platelet volume. This can cause the development of pathologies in the body. In patients, blood vessels gradually become clogged, blood circulation is disrupted, and metabolism slows down. Heart disease gradually develops.
An increase in PDW occurs:
- For anemia. The process causes oxygen starvation, which contributes to a change in cell volume.
- For bleeding after surgery.
- With the development of neoplasms and inflammatory processes.
- If, in addition to an increase in PDW, an increased number of leukocytes is noted, then the doctor diagnoses inflammation.
Analysis transcript
Interpretation of the results is the responsibility of the attending physician. Deviation of PDW from the norm indicates a violation of the size of the population of anucleate cells. An increase in this indicator may be associated with the presence of microerythrocytes, erythrocyte fragments, and platelet aggregates. Changes in PDW can be observed in myeloproliferative diseases. This group includes the following pathologies:
- myelofibrosis,
- essential thrombocythemia,
- chronic myeloid leukemia,
- true polycythemia.
The PDW platelet distribution index helps identify the following pathologies:
- inflammatory diseases,
- anemia,
- parasitic infections (helminthic infestations),
- malignant diseases,
- condition of the walls of blood vessels.
The value of the platelet index is not considered separately, but only in conjunction with other indicators.
Distribution width is higher than normal
The indicator is highly lable, so the slightest pathology of the body changes the percentage of PDW.
The main reasons for increased platelet indices are:
- Any type of inflammation. This cause can be suspected if, in addition to increased heterogeneity, there is a high ESR and leukocytosis (signs of inflammation).
- Anemia. An increase in the indicator should be associated with a decrease in hemoglobin and the number of red blood cells.
- Malignant formations. It is assumed that the index increases when the metastasis process is activated. Platelets help with this through thromboembolism. They spread cancer cells.
- Blood loss (operative, traumatic, menstrual). The bone marrow actively produces cells and many young forms appear.
- Thrombocytopathies, thrombocytopenia associated with impaired immunity.
- Other causes include heavy exercise, sports, overeating, pregnancy and medications. Therefore, if the doctor sees a deviation from the PDW norm, but other indicators are normal, then there is no need to sound the alarm. It can be changed for a trivial reason. Over time, the numbers return to normal.
Additional examinations
Supportive measures allow us to establish the correct diagnosis:
- Oral interview with a hematologist.
- Anamnesis collection.
- Bone marrow puncture. It is prescribed to clarify the nature of the pathology.
- Assessment of the size of the spleen, ultrasound of the digestive tract. At the same time, the liver is examined.
- Biochemistry of blood.
- MRI or CT as needed. With contrast enhancement with gadolinium and iodine, respectively.
The question of what caused the index to rise or fall is complex. The doctors decide. Treatment is carried out as needed. It is mainly etiotropic, that is, aimed at correcting the underlying cause. Primary disease.
How is the analysis carried out?
The PDW value is determined during a general blood test along with many other indicators. Blood is taken from the (ring) finger on an empty stomach in the morning. Whole blood with an anticoagulant is used for the study.
The result may be unreliable if the patient ate food before the analysis, is being treated with medications during this period of time, or underwent an X-ray examination or physical procedures the day before. In addition, the indicator may be higher or lower than normal during pregnancy, before menstruation, or after heavy mental or physical stress. In such cases, a repeat study is prescribed. To avoid distortion of the results, you should properly prepare for the analysis.
Nowadays, modern hematological analyzers are used for blood testing, which obtain up to 24 indicators. Determining platelet volume alone is not sufficient for effective diagnosis. Normal hemostasis depends not only on the quantitative content of nuclear-free plates, but also on their functional indicators
Therefore, it is so important to study their quality characteristics, which is only possible on new equipment. Hardware methods for studying blood elements have many advantages over manual ones:
- a large number of cells are examined - from 10,000;
- provide accurate results - without errors;
- all stages of the study are standardized.
Using modern blood analyzers, histograms are obtained - a graphical representation of the results in the form of thrombocytometric curves
The importance of this study is due to the fact that the size of platelets determines their functionality, the change in their volume before gluing the plates in the process of clot formation, as well as the tendency to adhesion and the content of bioactive substances in anucleated cells
If there are predominantly young platelets in the blood, the histogram is shifted to the right, old platelets are located on the left of the graph. Thus, platelet volume decreases as platelet aging occurs.
Value of the study
The main indicators that the doctor pays attention to when deciphering a general blood test are hemoglobin and red blood cells, ESR, leukocytes and leukocyte formula. The rest are more likely to be auxiliary.
Most often, a general blood test is prescribed to understand whether there is inflammation and signs of infection in the body, and if so, of what origin - viral, bacterial or other.
Also, a general blood test can help determine anemia - anemia. And if there are signs of it in the blood, additional tests are prescribed to establish the causes.
A general blood test is also prescribed if there is a suspicion of an oncological process, when there are a number of warning symptoms and clues are needed. In this case, the blood can indirectly tell you in which direction to move next.
What to do if the platelet distribution index is elevated
Platelets are the most microscopic blood cells that can stick together to form a blood clot. It is needed in cases where the integrity of a capillary, vein or artery is damaged. Thanks to platelets, damaged vessel walls are sealed from the inside, which prevents the development of full-scale bleeding.
One of the indicators of laboratory tests for platelet count is the PDW index. Thanks to this analysis, the width of platelet distribution is determined - an important indicator by which one can judge the presence of many diseases and pathologies. What standards have been established, and what standards are recognized, as well as the reasons and consequences of increasing the maximum permissible values, we will analyze further.
In a healthy person, the normal width of platelet distribution by volume is 15-17 percent. Deviations of 2-3 percent are acceptable, which are attributed to the following manifestations:
- the blood test was taken incorrectly (on a full stomach, in the presence of drug impurities);
- physical and moral condition of the patient;
- the presence of chronic inflammatory diseases.
For children, the norms are slightly different: under the age of 18, rates from 10 to 16 percent are acceptable, writing off 1% in each direction. Poor immunity and increased vulnerability of the body, as well as the presence of congenital pathologies, make this indicator less reliable when deciphering a blood test.
Based on the fact that the reliability of platelet distribution width indicators is influenced by the general condition of the body, in the presence of chronic diseases, noma indicators may vary.
It is necessary to prepare for the test in advance
Indications for analysis
There are four cases when a complete blood count and identification of the PDW indicator is mandatory:
Feel free to ask your questions to a staff hematologist directly on the website in the comments. We will definitely answer.Ask a question>>
- When hospitalized, it is included in the mandatory list of tests required for the initial medical history.
- To monitor treatment, a blood test to determine the width of platelet distribution allows you to see the effect of treatment, or, on the contrary, to find out about its absence and the need to prescribe new drugs.
- An annual medical examination is a mandatory procedure not only for workers in all professions and industries, but also for children of all ages.
- In the presence of diseases of the circulatory system and suspected blood cancer, as well as for diagnosing inflammatory diseases.
A blood test is mandatory in most cases. It can be used to tell about a person’s health status, indicating possible problems.
In qualified clinics that have their own laboratories with ultra-precise equipment, the patient is given a transcript in hand, which is a table consisting of several columns. It reflects the available indicators, their norm and presence in human blood.
Usually the last column indicates whether there are deviations from the norm and what could cause this.
Deviation from the norm indicates the presence of pathologies or diseases, the treatment of which should be started as quickly as possible. A pathological condition is considered to be not only a result above the norm, but also a value below the recommended values. The therapist who receives the results of the analysis is obliged to inform the patient about possible problems with his health, as well as compare the patient’s symptoms and complaints with the data received. After this, a decision is made to undergo a comprehensive examination, the results of which will ultimately make it possible to make the correct diagnosis and select the most successful and effective treatment.
preparation for analysis was not carried out
- physical overload;
- unstable emotional background, especially in depressive states;
- eating immediately before blood sampling;
- During pregnancy and breastfeeding;
- blood sampling during menstruation in women;
- presence of chronic diseases;
- taking medications.
Therefore, in order to obtain the most accurate data, you should be in a good mood, not experience physical overload, and also limit your food intake. Women during menstruation or in the premenstrual period are better off refraining from testing. Taking blood without fasting and the presence of menstruation are the two most significant and significant factors on which the accuracy of the analysis depends.
It is important to note that failure to follow the blood sampling rules can also lead to unreliable data on other blood parameters. From here you can get not only deviations from the norm, but also an incorrect diagnosis
The essence of the analysis and what it shows
To understand what we are talking about, you need to turn to human anatomy and physiology.
Platelets are special shaped blood cells. They ensure its normal coagulation.
The development of cytological structures occurs in special tissues of the bone marrow. This process is called hematopoiesis, and if we talk about platelets in isolation, then thrombocytopoiesis.
Platelets perform their functions for quite a long time. Within 5-12 days. Then they die, and new ones come to replace them.
But this is not a quick phenomenon. Over the course of a short period of time, a shaped cell goes through all stages of life from youth to old age.
After maturation and immediately after leaving the bone marrow, the structure is large. The blood plate is capable of performing its tasks as efficiently as possible.
It takes less time and not as many platelets to close the wound surface. Moreover, adhesion and aggregation occur faster. That is, attachment to the wall of the vessel and accumulation, layering.
Old cells are no longer as active. More of them are needed, and the natural processes themselves proceed slowly and not as well as before. Hence the problems.
Accordingly, if there are more obsolete cytological units, then coagulability will suffer. Its intensity will not be so great that it will be reflected in the coagulogram.
The platelet distribution index or PDW precisely indicates the heterogeneity of cells: that is, the percentage of red plates distributed.
Normally they should be in dynamic equilibrium. Numbers from 1 to 20% are used as values. When young forms of cytological structures predominate, the formula shifts to the right. That is, in a big way. In the opposite case, when there are a lot of old cells, the opposite is true. The number will be lower.
The conditional generalized norm is approximately 15-17%. That is, young forms of platelets should predominate in the bloodstream. This is an indispensable condition for normal coagulation and functioning of the body. Of course, there are differences depending on the gender and age of the patients.
The analysis shows several main violations:
- Thrombocytopathies. A classic pathological process in which the functional activity of red blood platelets decreases. Formally, their number remains normal. This is where the index in question comes to the rescue.
Because the reason is often on the surface and lies in a change in the platelet ratio. The more old cells there are, the worse the body’s functioning is. In critical cases, obsolete structures remain.
- Thrombocytopenia. Different condition. With it, not only the PDW index changes, but also other indicators. The hallmark of the pathological process is a decrease in the number of platelets. It all depends on the primary diagnosis.
- Bone marrow disorders. It’s quite difficult to say exactly which ones. As a rule, with disorders of this kind, the previous named pathologies develop. At the same time, immature hematopoietic cells appear in the bloodstream. Megakaryocytes. They are unable to perform any functions. In this case, it makes sense to conduct a diagnosis. A bone marrow puncture is prescribed.
A blood test for PDW is far from the only necessary test. To tell exactly what is wrong with the patient, auxiliary measures are needed.
When thrombocrit is low
A decrease in PCT occurs when the production of platelets or platelet precursors, which are megakaryocytes, is blocked. With a decreased PCT, there is a tendency to bleed.
This indicator is reduced during pregnancy. The drop in thrombocrit in women can be 2 times lower than normal, but during pregnancy this reduces the risk of thrombosis, and means that blood circulation and fetal nutrition will not be affected.
PCT decreases in conditions caused by:
- anemia - folate deficiency, aplastic, megaloblastic;
- autoimmune diseases – systemic lupus erythematosus, collagenosis;
- chronic diseases of the liver, kidneys;
- poisoning by poisons, drugs - diuretics, cytostatics, antibiotics, corticosteroids;
- chemotherapy;
- oncological diseases - hemoblastosis, leukemia.
When the thrombocrit is lowered and is less than 0.11%, then in adults this indicates a disorder of hematopoiesis in the bone marrow or an acceleration of the breakdown of platelets in the spleen.
A low PCT thrombocrit in a child’s blood test may be explained by:
- in infants - prematurity, low birth weight, hypoxia;
- in a child of an older age group – parasitic infection.
Complete blood count: WBC and leukocyte count
Most often, in a general blood test, WBC is determined with a leukocyte formula. There are five types of leukocytes that are examined in a blood test - neutrophils, eosinophils, basophils, lymphocytes, monocytes. The leukocyte formula is the percentage of these types of leukocytes.
Neutrophils
The most numerous type of leukocytes, which plays a major role in providing immunity to the body. Normally, the content of neutrophils in the blood is 60–75% of all leukocytes in adults, and 30–65% in children aged 6 to 12 years. An increase in the level of neutrophils (neutrophilia) is observed in infectious diseases (pneumonia, bronchitis, intestinal infection, sinusitis, sore throat), arthritis, thyroiditis, peritonitis, pancreatitis, osteomyelitis, gangrene, phlegmon, abscess, cancer, uremia, diabetes, heart attacks.
A reduced level of neutrophils (neutropenia) may indicate certain infections (rubella, viral hepatitis, chickenpox, influenza, typhoid fever), acute leukemia, aplastic anemia, thyrotoxicosis.
Eosinophils
They take part in protecting the body from parasites and allergic reactions. The norm in the WBC blood test for eosinophils is 1–5% of the number of all types of leukocytes. The reasons for the increased content of this type of leukocytes in the blood are allergic reactions, parasitic infections (enterobiasis, ascariasis, giardiasis, echinococcosis, opisthorchiasis), malignant neoplasms, diseases of the hematopoietic system, scleroderma, periarteritis nodosa, rheumatoid arthritis.
A decrease in eosinophils is observed during sepsis, purulent processes, intoxication with heavy metals, and at the beginning of the development of inflammatory processes.
Lymphocytes
A special type of leukocyte, which is responsible for the formation of the body’s specific immunity. Interestingly, this type of leukocyte predominates in the blood of children under 4–6 years of age. And only after this age does a gradual predominance of neutrophils over lymphocytes occur. The normal content of lymphocytes in the blood of adults is 20–35%.
An increase in the level of lymphocytes in the blood may indicate the development of viral infections (influenza, parainfluenza, adenovirus), tuberculosis, thyrotoxicosis, bronchial asthma, childhood infections (scarlet fever, whooping cough, rubella, measles). A significant increase in lymphocytes occurs with lymphocytic leukemia, a tumor lesion of the bone marrow.
A decrease in the volume of leukocytes can be a symptom of bacterial diseases (pneumonia, sepsis), myocardial infarction, lymphoma, systemic lupus erythematosus, HIV infection.
Monocytes
Immature blood cells that turn into macrophages when they enter body tissues. Macrophages absorb pathogens, foreign microorganisms, and dead body cells. The interpretation of the WBC blood test indicates the normal level of monocyte content - 4–10%. Monocytosis, or an increase in the content of monocytes, can occur with lymphogranulomatosis, lymphoma, some types of leukemia, subacute endocarditis, tuberculosis, sepsis, brucellosis, malaria, syphilis, mononucleosis, toxoplasmosis.
A reduced concentration of monocytes occurs with dysfunction or damage to the bone marrow, radiation sickness.
Basophils (mast cells)
A type of white blood cell that is responsible for the release of histamine (a hormone that provokes an allergic reaction in the body). Normally, the basophil content is 0–1%.
An increase in basophils in the blood may indicate allergic diseases, megakaryoblastic leukemia, chronic myeloid leukemia, systemic mastocytosis, some infections (influenza, chickenpox, tuberculosis), Hodgkin's disease.
A decrease in basophil levels is often a symptom of acute infection, hyperthyroidism, anaphylactic shock, and bronchial asthma.
When PDW Becomes Important
The decoding of the analysis proceeds in parallel with the decoding of other platelet indices (primarily MPV).
This platelet indicator is increased in the case of certain pathological conditions:
- Inflammatory processes;
- Liver pathologies;
- Cardiovascular diseases;
- After removal of the spleen;
- Malignant neoplasms and, in particular, their metastasis to the bone marrow;
- Massive blood loss;
- Poisoning with salts of heavy metals (lead);
- Certain anemic syndromes;
- Corticosteroid therapy;
- Alzheimer's diseases.
In addition, the index is also increased in some cases that can hardly be called pathological conditions, but which could cause a high degree of platelet anisocytosis:
- Excessive physical activity;
- Surgery.
The platelet index PDW, on the contrary, is reduced when:
- Some blood diseases;
- Radiation sickness;
- Myelodysplastic syndrome;
- Megaloblastic anemia;
- DIC syndrome;
- Diseases of viral origin;
- Septic conditions;
- Severe liver damage.
In addition, PDW is reduced in situations where there is a need to use certain groups of pharmaceuticals, for example, cytostatics.
examples of PDW graphs – normal, with thrombocytopenia, hyperthrombocytosis with the presence of macroplatelets in the blood
Taking into account that platelets are sensitive cells, when going for analysis, you need to remember some rules: do not overeat, do not overload mentally, do not overexert yourself physically, do not smoke or drink medications that can change your blood picture. However, given that such a test is not carried out independently, but goes in tandem with other platelet indices, there is no point in describing the entire preparatory part in detail
The reader can find answers to these questions in other publications concerning the general blood test in general and the platelet component in particular.
Display all posts with the tag:
Analyzes
Go to section:
Blood diseases, tests, lymphatic system
Recommendations to SosudInfo readers are given by professional doctors with higher education and specialized work experience.
One of the leading authors of the site will answer your question.
Features of the analysis
It is necessary to prepare for the test in advance
Which doctor should I contact?
Increase in coefficient
If the PDW decoding indicates an increase in values, this is a direct sign of significant heterogeneity of the described cells in volume. And, accordingly, this state of the blood fluid can lead to dangerous consequences. The gradual clogging of capillaries, and then larger vessels, causes difficulties with blood circulation, which leads to even greater thrombus formation. This results in a so-called vicious circle.
PLT in blood test - what is it?
The result of this condition can be many pathologies, ranging from metabolic disorders in the bloodstream to heart disease (myocardial infarction) or blood clots in the brain (stroke).
Indicators may be elevated in the following situations:
- Bleeding due to surgery or injury leads to an increase in platelet concentration, which is due to their increased production. This is required to quickly restore the normal blood formula.
- Anemia, which causes oxygen starvation, as a result of which nuclear-free blood cells undergo various types of deformation.
- Pathologies of an oncological nature, leading to systematic damage to all formed elements of the blood, including platelets. This, in turn, causes a change in their volume, and, consequently, the width of distribution in the blood mass itself.
- Inflammatory processes leading to an increase in the number of these cells, and as a result, an increase in PDW. A parallel increase in leukocytes can only mean one thing – the development of inflammation is obvious!
At the same time, you should know that if PDW is elevated, then not in all absolutely cases this will mean the presence of any serious abnormalities in the body. The reasons for this can be the most trivial, for example, failure to comply with the basic rules of preparing for a blood test or directly collecting it from the laboratory medical staff.
Therefore, before undergoing the analysis, it is necessary to consult with a doctor about all possible subtleties in order to minimize the risks of receiving unreliable results and repeated analysis. Firstly, you need to know that blood is donated only on an empty stomach, that is, at least 10–12 hours must pass between the last meal and the collection of biomaterial.
Secondly, it is necessary to exclude excessive physical activity and, if possible, psycho-emotional activity the day before the study. Thirdly, you should refrain from taking any medications, even if they are multivitamin complexes, having previously discussed stopping them for several days. Strict adherence to all of the above measures will allow the doctor to see a complete picture of the patient’s blood condition.
How to prepare for the procedure
Very often, patients ignore the specialist’s recommendations for preparing for blood sampling, but the result of the laboratory test depends on this. In case of uncharacteristic changes in PDW, one should not discount the fact that it was incorrect preparation for the analysis that led to this result.
How to properly prepare for the procedure?
- 24 hours before the procedure, avoid absolutely all physical activity. This is due to the fact that during sports the body requires more oxygen consumption, which leads to an increase in platelets in the blood.
- Before taking blood, you should sit quietly for 20 minutes and calm down.
- It is necessary to take the test on an empty stomach. And also, at least 24 hours in advance, give up everything spicy, salty and peppery. This is due to the fact that such products enhance liver function, which leads to false test results.
- It is forbidden to drink coffee on the day of the test itself.
- Alcoholic beverages should not be consumed at least three days before the scheduled event.
- The test results are affected by the use of synthetic hormones, so you should take a break from taking medications. If this is not possible, then you must notify your doctor.
If there are deviations in the results of the laboratory test, the specialist is obliged to reschedule the procedure. This will help to accurately determine the reason for the change in indicators. If during a complete examination of the patient no abnormalities in health are noted, then monitoring of PDW is necessary; it is possible that its decrease is a temporary phenomenon of unknown origin. In any case, a diagnosis can only be made after receiving repeated results from blood tests and other procedures.
Definition and concept of platelet volume
To make a correct and comprehensive diagnosis, it is not enough to see the platelet count alone. It is necessary to know their average volume. The value indicating the average platelet volume in the blood is called MPV in tests. It is calculated using special equipment and measured in femtoliters (Fl). The device first calculates the platelets themselves in the blood taken, and then calculates their volume (roughly speaking, the space occupied by platelets).
We recommend studying the article “What role do platelets play in human blood?” on a similar topic within this material
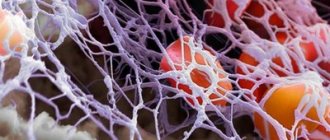
Formation of a blood clot from red blood cells and platelets (micrograph layout)
Average platelet volume is reduced
A decrease in average platelet volume occurs when many old, low-volume, “spent” cells circulate and accumulate in the blood. It is logical that a decrease in platelet volume, i.e. qualitative indicator occurs when the quantitative indicator increases.
The average platelet volume is reduced in the following cases:
- diseases of the blood coagulation system (coagulopathy);
- inability to adequately and timely synthesize new blood cells due to oncohematological diseases, congenital bone marrow aplasia, radiation therapy or the use of antitumor drugs that inhibit hematopoietic function;
- inability to fully utilize “waste” cells (diseases of the liver and spleen, lymphogranulomatosis).
We also recommend studying this topic:
Average platelet volume is increased
An increase in the average volume occurs when young (up to blasts) elements of the platelet series are present in the blood. Immature platelets are released into the bloodstream due to increased bone marrow activity.
Hematology analyzer
The mean platelet volume is increased when:
- post-hemorrhagic conditions (anemia, blood loss - acute and chronic);
- congenital diseases (thrombocytopenic purpura of Henoch-Schönlein, thalassemia);
- diabetes mellitus;
- infectious diseases.
What are platelets?
Platelets (PLT) are cells designed for the stable functioning of the body's blood vessels. The site of PLT formation is the bone marrow. The method for determining blood platelets is a general blood test.
Blood plates perform a number of functions:
- Hemostatic - for skin lesions, PLTs are combined into large and small groups to stop bleeding.
- Nourishing - in case of wounds or damaged skin, they nourish the inner surface of blood vessels.
- Protective - can independently absorb small bacteria (phagocytosis).
- Transport - capable of delivering various substances to the body, for example, serotonin.
- Strengthening - help maintain the density of the walls of blood vessels to reduce their premature destruction.
The optimal PLT level is 150-400*109/l. These indicators depend on the patient’s age, as well as gender and general condition of the body. In addition, platelet values change by 10-15% throughout the day.
In medicine, it is worth distinguishing 5 forms of blood platelets, namely:
In addition, PLTs go through 3 stages to stop bleeding, namely:
- Adhesion is the adhesion of blood platelets to the walls of a damaged vessel.
- Activation - enlargement of cells in order to increase the area of interaction.
- Aggregation is the sticking together of PLT with the help of fibrinogen (via receptors).
Carrying out analysis
The indicator is determined by drawing blood. In order for the indicators to correspond to reality, the following must be taken into account:
- It is not recommended to take the test during the premenstrual period.
- The day before donating blood, you should avoid heavy physical activity and, if possible, avoid taking medications.
- Tests must be taken on an empty stomach; in the morning you can only drink a glass of water.
The determination of indicators is carried out using the Fonio method. The material for the study is blood obtained from a finger, mixed with a sterile solution of magnesium sulfate.
From the resulting material, a smear is made on glass, which is placed in special equipment. The automatic counter counts the number of different forms of platelets per 1000 red blood cells. Using a special formula, the percentage of the width of the distribution of blood platelets is calculated.
Reasons for falsely high results
Among them:
- Wrong analysis.
- Violations of sample processing techniques.
Sometimes the patient himself may be to blame. Many factors influence the final result.
Deviation occurs in the following cases:
- Intense physical activity. Approximately a day before taking the test, you should not practice excessive mechanical activity.
- Smoking. It is abandoned a few days before the study.
- Eating. Food should be avoided 3-4 hours before blood sampling. This way the results will be more accurate.
- It is not advisable to take the test during menstruation, pregnancy and breastfeeding. Because the results will definitely be false. Possibly within the margin of error.
- You should also not drink alcohol, overheat or become hypothermic. In about 1-2 days. Deviations within small values are possible. If other analysis indicators are normal, such errors are not paid attention to.
When the platelet distribution index is increased, this means that the number of young cells is greater than the number of old, waste structures. As a rule, blood diseases are to blame.
It often turns out that there is no pathological process and the deviation is due to the actions of the patient. Smoking, leading an unhealthy lifestyle.
Reasons for the decline
A decrease in the number of platelets in a blood test indicates a high risk of bleeding due to low blood clotting. This must be taken into account in surgical operations.
A reduced PDW in a blood test occurs with myelodysplastic syndrome. This disease affects the bone marrow, where platelets are formed. Hepatitis provokes a decrease in PDW. In this case, the analysis will show increased bilirubin. Possible cancer.
An increased distribution of platelets in a child may be due to an inflammatory process. Also, the number of leukocytes in this case will be high.
Why deviation is dangerous and what to do
If the test result shows that the PDW does not meet the norm, the therapist will order you to take it again in different laboratories. If this is confirmed, then a comprehensive examination is prescribed. If the patient has additional symptoms, it is easier to make a diagnosis.
A reliable result is not only due to the patient’s good preparation, but also to the laboratory in which the blood is drawn. Poor quality reagents incorrectly determine blood composition. It is advisable to take tests in laboratories that have quality certificates and modern equipment.
Only a specialist should explain the result: there are many nuances in deciphering the PDW indicator. In some cases, the indicator is looked at in relation to other points of laboratory research.
Other cases of abnormal PDW blood levels
Reasons why PDW levels in the blood may change
Elevated PDW levels do not always mean some terrible disease such as cancer, severe anemia, or internal bleeding. Sometimes the reasons are ridiculously trivial, especially if PDW is the only indicator that has a serious deviation from the norm in the overall analysis. And this is a violation of the rules for taking tests.
Before you blame the laboratory workers and the nurse who took the test, carefully remember what you did or did not do before donating blood. Although no special preparation is required, there are a number of restrictions that the doctor must warn you about in advance. It is not recommended to neglect them:
Physical exercise. After active physical activity, the heart rate increases, and the number of various blood cells increases rapidly. Therefore, the analysis may be unreliable
It doesn’t matter how long a person has been playing sports, he should be at rest for about 30-40 minutes before taking the test. It is advisable to limit the load the day before the analysis.
Welcome, write. You should not eat food earlier than 8 hours before the test. The blood may clot, examination will become impossible, and all formed elements will dissolve. The day before the test, it is not recommended to eat fatty and spicy foods so that the liver function does not worsen and cholesterol is not even higher than usual. Menstruation. During menstruation, a woman's pure platelet count decreases. To avoid getting a false test, it is recommended to avoid donating blood during this period of the cycle. Pregnancy. During pregnancy, hormonal changes occur in the body, which cannot but affect the blood test. Blood clotting increases, cholesterol levels also increase. The hormone test will also be different. The doctor takes this into account when looking at the results. Taking medications Many medications affect test results. Therefore, on the day of donating blood, do not take any medications; it is recommended to even stop taking vitamins. Consult your doctor; some medications may not be taken a day or two before the test.
- Myelodysplastic syndrome. The abbreviation MDS refers to a range of diseases affecting the bone marrow. As you know, it is in it that blood cells are formed. Therefore, MDS cannot but affect the blood test. This is the only way to detect the disease. The reasons are usually unknown. MDS can occur after chemotherapy or chemical poisoning.
- Leukemia. This disease is also called blood cancer. Cancer cells attack the bone marrow and the normal formation of blood cells becomes impossible. As a result, the patient experiences a decrease in the number of almost all blood cells, and the immune system suffers.
- Metastases to the bone marrow. Any cancer at a certain stage metastasizes. They can affect the brain and spinal cord, as well as other organs. In this case, except for PDW, almost all blood parameters will be reduced.
- Thrombocytopenia. This is an insufficient number of platelets in the blood. This condition itself can be caused by a variety of reasons: bleeding, cancer, etc. It manifests itself in increased bleeding of the gums, hemorrhages, and anemia.
- Radiation sickness. Radiation sickness is a condition of the body that occurs as a result of radioactive radiation of a certain range. The most striking symptoms are low blood pressure, hand tremors, decreased muscle tone, and diarrhea.
- Chronic hepatitis. Despite the scary name, chronic hepatitis is usually mild and does not cause serious liver damage. Blood test results may be abnormal. This is primarily manifested in increased bilirubin.
A timely blood test will be one of the finishing touches in the overall picture necessary to make a correct diagnosis.
Reasons for RDW deviation
If the width of the distribution of red blood cells in the body is increased, this means that the sizes of the red blood cells are very different from each other. Moreover, the larger the red blood cell, the shorter its lifespan, which reduces the number of red blood cells in the body.
With significant destruction of red blood cells, an increased iron content is observed in the blood. At the same time, an increase in bilirubin occurs (the so-called very toxic substance that is formed from dead red blood cells). It is sent to the liver for neutralization, which causes it to become overloaded and poorly cope with processing toxins. This negatively affects the functioning of the entire body.
An increased RDW value in many cases indicates iron deficiency anemia. With this disease, the RDW value may increase even before the red blood cell and hemoglobin values change. That is why the volume of red blood cells makes it possible to determine the presence of the disease at the initial stage and take timely measures to eliminate it. At the same time, during treatment, the RDW index steadily increases, which is associated with the appearance of young red blood cells. If therapy is effective, red blood cell volume is the last indicator that returns to normal, and therefore indicates recovery.
In addition, the width of the distribution of red blood cells can increase in the following situations:
- Hemolytic anemia of an immune nature.
- Megaloblastic anemia (B9 and B12 deficiency).
- Hemoglobinopathy is the presence of pathological hemoglobins in red blood cells and is inherited.
- Liver problems.
- Blood transfusion.
The width of the distribution of red blood cells is never considered by a doctor separately from other indicators. The doctor must look at other erythrocyte indices (MCV, MCH, MCHC). This is necessary in order to more accurately diagnose a person’s condition.
For example, if the value of the distribution width of erythrocytes is within the normal range, while the mean erythrocyte volume (MCV) is reduced, this may indicate a hereditary disease that is associated with a violation of the synthesis of one of the globin chains (thalassemia). The MCV value is lower than normal and the RDW content can be normal during hemorrhage, when the walls of the vessels are so permeable that blood leaks through them, leading to hemorrhages. In addition, normal erythrocyte volume and low average erythrocyte volume are observed after removal of the spleen in oncology.
It may also be that the width of the distribution of red blood cells is increased, while the average volume of red blood cells is decreased. Then you can suspect iron deficiency anemia or beta thalassemia (a disorder of the synthesis of the beta globulin chain). If both values are high, the body may be deficient in vitamin B or develop hemolytic anemia.
Reasons for the increase
The PDW value may be increased for the following reasons:
- anemia of various origins;
- the presence of inflammatory diseases;
- significant blood loss;
- physical stress;
- splenectomy;
- recovery period after surgery;
- undergoing a course of treatment with corticosteroids;
- oncological diseases.
If the width of the platelet volume distribution is higher than normal, a person may experience:
- general weakness and malaise throughout the day;
- decreased ability to work.
Etiology
The reasons that a child may have elevated platelets are as follows:
- congenital blood diseases;
- systemic and/or autoimmune diseases;
- oncological diseases, including blood cancer;
- Iron-deficiency anemia;
- enlargement of the spleen or removal of this organ;
- viral infections;
- severe, long-term infectious diseases that have led to a severe weakening of the immune system;
- disruption of the circulation of blood components during emotional or physical stress.
Elevated platelets in a baby can be caused by errors in nutrition - an incorrectly selected mixture, insufficient amounts of vitamins in the diet, early introduction of complementary foods. Only a doctor can determine why platelets in the blood are elevated.
Decrease in values
If the CBC indicates a decrease in the described parameter, then at the same time this is a sign of a low platelet count. A low platelet index is not always considered as a harbinger or symptom of various pathologies.
It is necessary to take into account that in women during menstruation, PDW is sometimes reduced. In addition, a decrease in the indicator can occur due to an unhealthy lifestyle, poor-quality or unbalanced nutrition, as well as the individual physical characteristics of the body
Low index values are observed in situations such as:
- diseases of the hematopoietic organs;
- oncological diseases;
- radioactive exposure;
- functional liver disorders;
- viral and bacterial infections;
- taking cytostatic drugs;
- DIC and myelodysplastic syndrome;
- anemia due to deficiency of vitamin B12 or folic acid.
Myelodysplastic syndrome is one of the reasons for a decrease in PDW - these are diseases that damage the bone marrow, which leads to less production of all formed blood components, including platelets. A decrease in the indicator is also observed with the formation of metastatic foci in the bone marrow.
Chronic hepatitis often causes a decrease in this coefficient, which means that the doctor, suspecting such a liver disease, must prescribe the patient to undergo a biochemical blood test. This will determine the concentration of bilirubin, and in case of hepatitis it will be high.
Attention! A sharp and at the same time strong decrease in the number of platelets, as well as their distribution in the blood volume, is considered no less dangerous to human life and health than an increase in the indicator. Such a change leads to the loss of the integrity of organs not only circulatory, but also other functional systems
Moreover, if, as a result of deciphering the analysis, it turns out that the parameter being studied is slightly increased, this circumstance should not be neglected. It is imperative to normalize its values and in the future try to control them, as well as take measures to maintain them at the proper level.
To obtain the most accurate analysis results, two indices are used to characterize PDW. These are SD (standard deviation) and CV (coefficient of variation). PDW-SD and PDW-CV provide the opportunity to maximize platelet heterogeneity to help guide diagnostic decisions. These two criteria must be taken into account when deciphering the results of the CBC, especially if any deviations in the number or distribution of platelets are detected.
Norm for women
The parameters of the relative width of platelet distribution do not depend in any way on the gender of the patient. But due to the characteristics of the female body, sometimes a slight deviation is allowed
from the norm, in which the woman does not develop a dangerous disease or pathology. Even under the condition of exclusivity, the PDW analysis indicators should not deviate from the norm by 1-2%, otherwise the cause should already be sought in a disorder in the functioning of the internal organs.
Typically, the indicators deviate from the accepted values of 15-17, sometimes 10-15% is taken as the norm when engaging in heavy sports activities
, when employed in physically demanding work, in a state of pregnancy and breastfeeding.
A hearty dinner on the eve of the test, as well as even minimal food consumption a few hours before the test, can also prevent you from getting an accurate analysis. Deviations from the accepted parameters are also allowed in the period before the onset of menstruation.
If there were no such interferences with the PDW analysis, and the result turned out to be bad, the patient is prescribed a repeat blood donation and more often a venous blood test is used for this.
. If deviations are confirmed, a more in-depth, often in-patient, examination is carried out.
Significance in diagnosis
First of all, by determining thrombocrit indicators, the following aspects are established:
- Determination of the risk of bleeding, increased thrombosis (thrombocytosis condition).
- Assessment of the benefit/risk ratio when prescribing certain medications.
The most well-known reasons for determining this indicator in the blood are:
- The patient has a high temperature of unknown origin.
- Evaluation of treatment with immunosuppressive drugs.
- Severe viral, bacterial, fungal infection of the body.
- The patient is on artificial ventilation.
- Complications after organ transplantation.
Important. It must be taken into account that any change in the number of platelet germ cells - an increase (thrombocytosis), a decrease (thrombocytopenia), a change in shape, aggregation - immediately affects the thrombocrit numbers
To assess platelet distribution in peripheral blood, it is necessary to know its normal values.
Recommendations for taking the test
There is no need to prepare extensively to take the pdw test. It is recommended to donate blood on an empty stomach in the morning so that there is no reason for false results. If a person is taking medications, the specialist must be informed about this before taking blood. This blood test will be ready very quickly.
Usually blood is taken from a finger, but if additional information is required for research, then venous blood is needed, which contains a larger number of indicators that are needed for a more accurate analysis. If any of the components deviates from the norm, then the analysis from venous blood will be more informative and there is no need to repeat the test.
Blood sampling from children on pdw is carried out from a finger, as this is more comfortable for the child and more convenient for the nurse.
The material is sent to the laboratory for testing and preparation of results. It takes two days to complete all these actions.
In addition, different laboratories have different equipment and different reagents, so two laboratories may produce completely different results in terms of accuracy.
What does the PDW index mean in a blood test: interpretation and norm
Blood contains various enzymes and substances
Currently, up to 24 different indicators are known in medicine that are important for the functioning of the human body. Of these, the most vital are leukocytes, hemoglobin concentration, red blood cells, hematocrit, platelets and the average concentration in the blood of each of them.
About hematocrit norms in children:
PDW indicator refers to blood platelet indices. The transcript of the analysis characterizes the relative width of the distribution of platelets by volume. In other words, it is also called an indicator of platelet heterogeneity. Accordingly, there is a certain norm that must be present in the blood. Otherwise, the patient will experience disruption of the circulatory system, possible chronic or acute diseases and other abnormalities.
For example, the normal width of platelet distribution by volume is in the range of 15% - 17%. If this percentage is increased, then they speak of a violation of the size of the platelet population. Platelet indices also include MPV - the average platelet volume, the norm of which ranges from 7 to 10 fl. PCT - thrombocrit, the component norm is 0.108 - 0.282 as a percentage of the entire proportion of blood that is occupied directly by platelets.
Details about thrombocrit:
Laboratory research
No special preparation is required to determine the test results. General analysis in this regard is very convenient, as it allows you to identify the presence of a particular problem in a patient at any time of the day. Only in this case there are some restrictions regarding food intake or medications. Therefore, it is still recommended to take a general analysis in the morning on an empty stomach, when there are no additional irritants for false results.
Blood is most often taken from a finger capillary, but there are cases of venous blood taken. This can only be explained by the fact that venous blood contains a larger and clearer amount of exactly those indicators that are expected from the analysis. For example, if one or another component is elevated, then in venous blood this figure will be more clear. This way you won’t have to take the test again. But for children, it is easier to transfer blood sampling from a finger, as it is faster and more convenient for the nurse herself.
The collected material is immediately sent for laboratory testing. Therefore, results should be ready in as little as two days, depending on the laboratory. It is also worth noting that you should not always rely on the results of one laboratory. This can be explained by the fact that each research point uses certain equipment and different reagents. Therefore, sometimes false results come. For greater reliability, it is better to take tests in two or three laboratories at once, so that the doctor can see the overall picture of the examination and prescribe further treatment.
Nuances and features of a general clinical blood test:
results
Research and analysis preparation are carried out in the laboratory
The interpretation of each analysis is carried out directly in the laboratory when examining the material. The patient receives ready-made results, which indicate the rate of the indicator or its increase. If the PDW result is still significantly elevated, this may indicate the presence of cancer. But it is worth considering that the norm of all others is also absent. If only one pdw is elevated, and everything else is within normal limits, then the cause must be sought in other ways.
What can cause a low blood count?
If PDW platelet distribution is reduced, then most likely the cause of this condition is:
- blood oncology;
- illness due to increased exposure to radiation;
- myelodysplastic syndrome;
- DIC (disseminated intravascular coagulation);
- diseases caused by viruses;
- sepsis;
- taking cytostatics;
- iron deficiency;
- liver problems.
Myelodysplastic syndrome is often diagnosed in patients with reduced PDW. This disease affects the bone marrow, where platelets are formed. In addition, with metastases in bone marrow cells, the rate will also be low.
Hepatitis can provoke a decrease in PDW. To confirm the diagnosis, it is necessary to take a liver test and a biochemical blood test.
If one or more diseases are detected, therapy must be started immediately. With effective and successful treatment, the platelet count will also return to normal. Constant monitoring of your health will allow you to see deterioration in time and make predictions, as well as change your treatment regimen.
In addition to pathological processes in the body that could provoke a decrease in PDW, improper preparation for the analysis could lead to this phenomenon. To exclude false test results, it is necessary to retake it.
Indications for the study
There are quite a lot of reasons for diagnosis. In more detail:
- Bone marrow disorders. Myeloproliferative diseases and conditions in which the maturation of formed cells is disrupted. Not only platelets, but also red white blood cells. Also other bone marrow disorders. Up to blood cancer.
Unfortunately, the analysis is too general to show specific changes. Deviations by PDW are merely indications of a violation. But it is by no means an exhaustive diagnostic method. A bone marrow puncture and other tests will be required.
- Previously diagnosed thrombocytopathy. A condition in which the functional activity of blood cells decreases, but their number remains at a normal level. Happens quite often. It practically never happens to be primary. As a rule, the disorder is caused by other pathological processes.
- Cancer diseases. Regardless of type, stage and location. The platelet distribution index (PDW) may well be a nonspecific marker of the oncological process.
The reason for this is bone marrow dysfunction. It can no longer function in “normal” mode. Consequently, cell maturation slows down. Precursors and old forms of platelets circulate in the bloodstream. This is a fairly typical clinical picture of cancer.
- Preparing for hospitalization. The study of the platelet distribution index is included in the mandatory list. Especially if doctors are planning surgical treatment or invasive procedures. The decrease clearly speaks in favor of coagulopathies.
Attention:
Coagulation disorders are a contraindication for surgical treatment.
- Therapy control. The study of the platelet distribution index is also practiced as part of dynamic observation, when specialists assess the patient’s health status after therapy. This is necessary, for example, in the treatment of megaloblastic, iron deficiency anemia and other pathological processes.
- Preventive examinations. Semiannually. Typically, PDW testing is performed as part of a routine blood test. Therefore, the patient does not have to break down and run for additional research.
The list of indications is approximate. The doctor, at his own discretion and discretion, prescribes the study. If there is a reason for it.
How to normalize platelet levels
To restore the level of platelets and increase their level in the blood, first of all you need to stop psychological stress (being nervous, quarreling, experiencing stress), and also perform as little physical activity as possible. But this is not enough to restore normality. Therefore it is necessary:
- Take special medications that restore (increase or decrease) the number of platelets in the blood. Use such medications only after consulting a doctor.
- To eat well. It is necessary to strictly reduce to a minimum value, and it is best to exclude from the diet all pickled foods, spicy foods, alcoholic drinks, seaweed, grapes, and cucumbers. But almonds, dill, parsley, bananas, fish, and liver should be added to your diet.
- If your platelet count is low, you should stop taking medications that reduce the number of platelets in your blood. In most cases, these are antidepressants and antibiotics.
- Consume more vitamins C, B12 and A.
- In addition, you need to start leading a healthy lifestyle, get rid of bad habits, do not drink alcohol, do not smoke, watch your sleep, and do not engage in traumatic sports.
Low values
An insufficient concentration of platelets per 1 liter of blood negatively affects its clotting.
At low thrombocrit values, the risk of causeless bleeding (both external and internal) increases, which will be very difficult to stop. Depending on the age and gender of the patient, hematologists and therapists differently characterize the identified indicator as low.
According to the standards:
- for women it is less than 0.14%;
- for men - similarly;
- for pregnant women or girls taking a blood test at the beginning of the cycle - below 0.06%;
- for people over 75 years old - less than 0.16%;
- for children aged from birth to 12 months – below 0.1%;
- for children older than one year – less than 0.17%.
The platelet count may decrease due to existing pathological processes or due to previously suffered diseases.
Most often, such changes in the composition of the blood are caused by:
- a tendency to develop anemia (low hemoglobin or “anemia”);
- renal failure;
- liver problems;
- deficiency of vitamins, in particular folic acid;
- infectious or viral disease;
- lupus erythematosus disease;
- existing leukemia or hemoblastosis;
- indiscriminate use of antibacterial and diuretic drugs;
- recently completed chemotherapy;
- intoxication of the body;
- radiation damage;
- underweight;
- the presence of intestinal parasites.
It is possible to normalize thrombocrit levels only with the help of an integrated approach. The patient is usually recommended to review his diet and undergo a course of drug therapy.
In your daily menu you should focus on:
- fruits (bananas, apples, pomegranates, melons);
- vegetables;
- seaweed;
- gluten-free porridges (buckwheat, rice, corn);
- nuts (hazelnuts, walnuts);
- peas;
- beans;
- lean meat (in particular beef);
- fresh herbs;
- green tea
Among the drugs used to increase the level of platelets in the blood, the most effective are:
- "Dicinon" (a drug for the treatment of capillary bleeding);
- "Derinat" (remedy for parasites);
- "Vikasol" (medicine for hemorrhagic disease and hypovitaminosis).
After treatment, it is necessary to take a blood test again to ensure that the thrombocrit level has returned to normal.