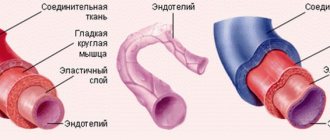
Human arteries and veins perform different jobs in the body. In this regard, significant differences can be observed in the morphology and conditions of blood flow, although the general structure, with rare exceptions, is the same for all vessels. Their walls have three layers: inner, middle, outer.
The inner shell, called intima, necessarily has 2 layers:
- the endothelium lining the inner surface is a layer of squamous epithelial cells;
- subendothelium - located under the endothelium, consists of connective tissue with a loose structure.
The middle shell consists of myocytes, elastic and collagen fibers.
The outer shell, called “adventitia,” is a fibrous connective tissue with a loose structure, supplied with vascular vessels, nerves, and lymphatic vessels.
Arteries
These are blood vessels that carry blood from the heart to all organs and tissues. There are arterioles and arteries (small, medium, large). Their walls have three layers: intima, media and adventitia. Arteries are classified according to several criteria.
Based on the structure of the middle layer, three types of arteries are distinguished:
- Elastic. Their middle layer of the wall consists of elastic fibers that can withstand the high blood pressure that develops during its release. This type includes the pulmonary trunk and aorta.
- Mixed (muscular-elastic). The middle layer consists of varying numbers of myocytes and elastic fibers. These include the carotid, subclavian, and iliac.
- Muscular. Their middle layer is represented by individual myocytes arranged in a circular pattern.
According to their location relative to the organs, arteries are divided into three types:
- Trunk – supply parts of the body with blood.
- Organ - carry blood to the organs.
- Intraorgan - have branches inside organs.
Vessels: what you need to know?
22.10.2019
There are three main types of blood vessels in the human body: arteries , veins , and lymphatic vessels . They all look like a rubber pipe with many branches and different passages. pink arteries the veins are bluish and soft. Blood vessels are yellowish.
Story
Ancient anatomists connected arteries and veins with various organs. In the Middle Ages, scientists misunderstood the system of arteries ; they thought that they were not all connected to each other. This theory was refuted by the Italian physician Jacopo Berengario da Carpi at the end of the 15th century. He noticed that an artery is connected to every artery . In the 16th century, anatomists tried to answer the question of how blood gets from veins to arteries . This was clarified in the second half of the 17th century by William Harvey, who discovered blood circulation.
Under a magnifying glass
The wall of the vessel consists of three layers. Its inner part consists of a lining of flat cells (the so-called endothelium; the entire inner layer has other parts and is called intima). The middle layer consists of round and spirally oriented smooth muscle cells. The outer layer of the vessel is a compound that forms a flexible membrane (adventitia). The adventitia connects blood vessels and nerves to nourish and control vascular . Arteries have a thicker layer of muscle than veins . The capillary wall consists of a single layer of cells - the endothelium. In the veins, the endothelium forms a small pocket, a flap, in certain places, preventing blood flow. Blood vessels have a similar structure to veins .
Comparative anatomy of blood vessels
As is known, humans have a closed blood circulation. For example, mollusks, snails, arthropods and jellyfish have open blood circulation. Their “blood” or hemolymph, if present, is located directly between the organs of the body. Insects are less developed, they have only a simple tubular heart .
Anatomy
Blood vessels extend from the heart to all organs and cells. The aorta originates in the left ventricle, descends into the abdomen and flows into the pelvis, where it divides into two arteries that carry blood to the lower extremities. arteries (emanating from the aorta) also function blood to the head, upper limbs, all internal organs and skin. The arteries branch into smaller ones and eventually become capillaries. Arterial capillaries pass into venous capillaries, which converge further into veins . The superior vena cava carries blood to the heart from the lower extremities, abdomen and torso, and it also carries blood from the head and upper extremities. Blood vessels form blindly between cells flowing into stronger trunks and entering veins .
Functions
Blood vessels are used to transport blood in the body. A person has a so-called closed circulation. This means that blood flows only in blood vessels and does not accidentally “wash” certain organs. Arteries carry blood from the heart . Most of this blood is oxygenated, except for the blood that passes through the pulmonary artery from the right ventricle to the lungs . Veins carry blood to the heart . Except for the blood in the pulmonary veins , which is oxidized and flows into the left ventricle.
In the human body there are two circles of blood connected by the heart . The "small" or pulmonary circulation is where oxygenated blood is drawn through the pulmonary artery from the right ventricle into the lungs , where the pulmonary veins lead to the left ventricle. And the “large” circulation, where oxygenated blood from the left ventricle moves to the right atrium, and from there to other arteries and organs. There the blood loses oxygen and the veins return it to the heart . Blood vessels collect saliva in the intercellular spaces and transport it to the veins .
Published in Cardiology Premium Clinic
Vienna
They are non-muscular and muscular.
The walls of muscleless veins consist of endothelium and connective tissue of a loose structure. Such vessels are found in bone tissue, placenta, brain, retina, and spleen.
Muscular veins, in turn, are divided into three types depending on how the myocytes are developed:
- poorly developed (neck, face, upper body);
- medium (brachial and small veins);
- strongly (lower body and legs).
Veins, in addition to the umbilical and pulmonary veins, carry blood, which gives up oxygen and nutrients and takes away carbon dioxide and breakdown products as a result of metabolic processes. It moves from the organs to the heart. Most often, she has to overcome the force of gravity and her speed is lower, which is due to the peculiarities of hemodynamics (lower pressure in the vessels, the absence of a sharp drop, a small amount of oxygen in the blood).
Structure and its features:
- Larger in diameter compared to arteries.
- The subendothelial layer and elastic component are poorly developed.
- The walls are thin and fall off easily.
- The smooth muscle elements of the middle layer are rather poorly developed.
- Pronounced outer layer.
- The presence of a valve apparatus, which is formed by the inner layer of the vein wall. The base of the valves consists of smooth myocytes, inside the valves there is fibrous connective tissue, and on the outside they are covered by a layer of endothelium.
- All wall membranes are endowed with vascular vessels.
The balance between venous and arterial blood is ensured by several factors:
- a large number of veins;
- their larger caliber;
- density of the vein network;
- formation of venous plexuses.
What is an aortic aneurysm?
The article was prepared by cardiologist Ksenia Nshanovna Borel
The aorta is the largest unpaired arterial vessel in the human body.
In the anatomical structure of the aorta, several sections are distinguished: the ascending aorta and the descending aorta, which, in turn, is divided into the thoracic and abdominal aorta. What are the functions of the aorta?
Figuratively speaking, the aorta is a pipeline that carries out the function of transporting blood.
The aorta allows 200 million (!!!) liters of blood to pass through a person’s entire life! In addition, the aorta regulates blood pressure and heart rate.
A feature of the aorta is its specific structure: the aortic wall contains a large number of elastic and collagen fibers, which determines good extensibility and elasticity. The main arterial trunks depart from the aorta, supplying blood to all organs! It is for this reason that any disease of the aorta can be fatal.
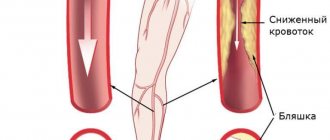
Normally, the diameter of the aorta does not exceed 40 mm and is characterized by a gradual narrowing in the direction from top to bottom. With age, over the course of every 10 years, the aortic root increases by 0.9 mm in men and by 0.7 mm in women, which, in turn, leads to thinning of the aortic wall and increases the risk of its rupture and the formation of an aneurysm.
Why is this happening? This is due to a decrease in the content of elastic and collagen fibers in the aortic wall, which is a manifestation of the “aging” of blood vessels. In other words, older people are at risk of serious damage to the aorta, which can be fatal.
But not all older patients experience aortic damage! This means that there are some additional provoking reasons. Which ones?
The most common of them are factors that change the condition of the vascular wall:
- high blood pressure,
- high levels of blood glucose and cholesterol,
- exposure to tobacco smoke,
- excessive alcohol consumption,
- trauma (as a manifestation of external influence).
Other causes of aortic damage are congenital (hereditary, genetically determined) diseases, which are characterized by thinning of the aortic wall:
- Turner Syndrome,
- Marfan syndrome,
- Ehlers-Danlos syndrome,
- Loeys-Dietz syndrome,
- syndrome of pathological tortuosity of arteries,
- syndrome of a combination of aortic aneurysm and osteoarthritis.
The damage can also be caused by injury (fall from a height, frontal/side collision during an accident).
In addition, patients with a bicuspid aortic valve are at risk for a high incidence of aortic aneurysm.
Attention! Aortic diseases are asymptomatic! It's a ticking time bomb!
If pain appears, this means only one thing - the patient has a very high risk of death, because if it hurts, it means it’s “tearing.” Sorry for this non-medical slang.
The pain varies in intensity. Localized in the chest or abdomen, depending on the location of the aneurysm. The pain may radiate to the spine.
Often the patient loses consciousness because massive blood loss occurs! Provoking factors: a sharp increase in blood pressure, injuries to the chest or abdomen, a sharp increase in intra-abdominal or intrathoracic pressure (coughing, straining, heavy lifting and others).
In this regard, every patient at risk should undergo a screening examination to actively identify problems with the aorta.
If you or your relatives belong to the risk category, then read this text to the end to know how you can prevent sudden death!
Let's talk about aortic aneurysm.
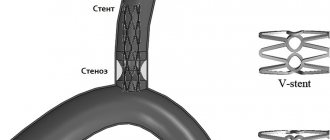
An aneurysm (from the Latin aneurysma - “expansion”) is a saccular or spindle-shaped local deformation of the wall of a vessel or heart.
The most common location of aortic aneurysms is its ascending section. This is a section of the aorta from the left ventricle of the heart and is 5-6 cm long.
The risk of aortic rupture increases when the diameter of the ascending aorta increases to more than 60 mm, and the descending aorta increases to more than 70 mm. Abdominal aortic aneurysms are most often localized in the projection of the origin of the renal arteries and are diagnosed when its diameter increases to more than 30 mm: here they need to be specifically looked for, this section is quite clearly visible when performing an ultrasound.
An insidious feature of an aneurysm is that its wall is very thin and is easily injured, which can cause massive bleeding.
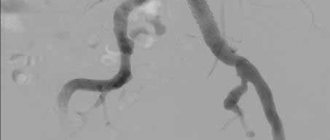
Since the aneurysm does not manifest itself clinically, it must be actively looked for. How?
You need to start by performing a routine ultrasound of the heart, ascending aorta and abdominal aorta. In some situations, it is more informative to perform an ultrasound using a different approach, examining the heart and large vessels not through the chest wall, but through the esophagus!
If signs of an aortic aneurysm are detected, then it is necessary to perform a more specific examination, which is of central importance: computed tomography or magnetic resonance imaging with or without contrast, or aortography.
Pay attention to signs that may indicate you are at high risk of developing an aortic aneurysm:
- hereditary factor - people whose relatives suffered or died from an aortic aneurysm have a much higher risk of a similar disease!!
- men over 65 years old
- smoking women over 65 years of age
Do you recognize yourself? Contact a specialist!
How to treat? It would be more correct to say “How to prevent?”
If the patient does not have congenital anomalies, then this is, first of all, the fight against all risk factors: normalizing blood pressure, normalizing blood glucose and cholesterol, quitting smoking and drinking alcohol. In other words, fight the causes of coronary heart disease!
If the patient has congenital defects in the structure of the aortic wall (see reasons above), then, in addition to the annual examination of the patient himself, an ultrasound examination of first-degree relatives (parents, brothers, sisters) every 5 years is recommended.
What to do if an aneurysm does form? Each specific case is individual: sometimes the situation requires regular monitoring and observation, and some situations require surgical intervention. The methods of surgery are different - stenting or prosthetics.
Let's recap:
- In certain categories of people, aneurysms should be actively identified
- a publicly accessible and inexpensive diagnostic method - ultrasound of the heart, supplemented by examination of the abdominal aorta
- aneurysms are often asymptomatic
- if an aneurysm is detected, then avoid provoking factors that contribute to rupture and regularly see a doctor
- actively combat all risk factors.
Your health is in your hands!
MAKE AN APPOINTMENT WITH A CARDIOLOGIST
Differences
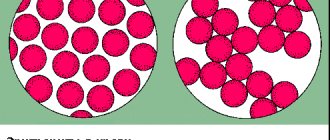
How are arteries different from veins? These blood vessels differ significantly in many ways.
Arteries and veins, first of all, differ in the structure of the wall
According to the structure of the wall
Arteries have thick walls, they have a lot of elastic fibers, smooth muscles are well developed, they do not fall off unless they are filled with blood. Due to the contractility of the tissues that make up their walls, oxygenated blood is quickly delivered to all organs. The cells that make up the layers of the walls ensure the smooth passage of blood through the arteries. Their inner surface is corrugated. The arteries must withstand the high pressure that is created by powerful surges of blood.
The pressure in the veins is low, so the walls are thinner. They fall off when there is no blood in them. Their muscle layer is not able to contract like arteries. The surface inside the vessel is smooth. Blood moves through them slowly.
In veins, the thickest membrane is considered to be the outer one, in arteries it is the middle one. Veins do not have elastic membranes, arteries have an internal and an external one.
By shape
The arteries have a fairly regular cylindrical shape, they are round in cross section.
Due to the pressure of other organs, the veins are flattened, their shape is tortuous, they either narrow or expand, which is due to the location of the valves.
In count
In the human body there are more veins and fewer arteries. Most middle arteries are accompanied by a pair of veins.
According to the presence of valves
Most veins have valves that prevent blood from flowing backwards. They are located in pairs opposite each other throughout the entire length of the vessel. They are not found in the portal cava, brachiocephalic, iliac veins, as well as in the veins of the heart, brain and red bone marrow.
In arteries, valves are located as vessels exit the heart.
By blood volume
Veins circulate approximately twice as much blood as arteries.
By location
The arteries lie deep in the tissues and approach the skin only in a few places, where the pulse is heard: on the temples, neck, wrist, and instep of the feet. Their location is approximately the same for all people.
Veins are mostly located close to the surface of the skin
The location of the veins may vary from person to person.
To ensure blood movement
In the arteries, blood flows under the pressure of the force of the heart, which pushes it out. At first the speed is about 40 m/s, then gradually decreases.
Blood flow in the veins occurs due to several factors:
- pressure forces depending on the push of blood from the heart muscle and arteries;
- the suction force of the heart during relaxation between contractions, that is, the creation of negative pressure in the veins due to the expansion of the atria;
- suction effect on the chest veins of respiratory movements;
- contractions of the muscles of the legs and arms.
In addition, approximately a third of the blood is in the venous depots (in the portal vein, spleen, skin, walls of the stomach and intestines). It is pushed out from there if it is necessary to increase the volume of circulating blood, for example, during massive bleeding or during high physical exertion.