Indications for placing a catheter in a vein
Often, in emergency conditions, access to the patient’s vascular bed cannot be achieved by other methods due to many reasons (shock, collapse, low blood pressure, collapsed veins, etc.). In this case, to save the life of a seriously ill patient, it is necessary to administer medications so that they immediately enter the bloodstream. And here central venous catheterization comes to the rescue. Thus, the main indication for placing a catheter in the central vein is the provision of emergency and emergency care in an intensive care unit or ward where intensive care is provided to patients with serious illnesses and disorders of vital functions.
Sometimes catheterization of the femoral vein can be performed, for example, if doctors perform cardiopulmonary resuscitation (artificial ventilation + chest compressions), and another doctor provides venous access, and does not interfere with his colleagues with manipulations on the chest. Also, catheterization of the femoral vein can be attempted in an ambulance when peripheral veins cannot be found, and the administration of drugs is required in an emergency.
central vein catheterization
In addition, the following indications exist for placing a central venous catheter:
- Carrying out open heart surgery using a heart-lung machine (ACB).
- Providing access to the bloodstream in critically ill patients in intensive care and intensive care.
- Installation of a pacemaker.
- Insertion of the probe into the cardiac chambers.
- Measurement of central venous pressure (CVP).
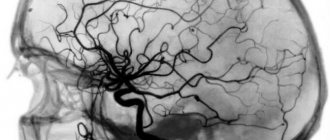
- Conducting X-ray contrast studies of the cardiovascular system.
Installation of a peripheral catheter is indicated in the following cases:
- Early initiation of infusion therapy during emergency medical care. When hospitalized in a hospital, a patient with a catheter already installed continues the treatment that has been started, thereby saving time for placing an IV.
- Installation of a catheter in patients who are scheduled for heavy and/or round-the-clock infusions of medications and medical solutions (saline solution, glucose, Ringer's solution).
- Intravenous infusions for patients in a surgical hospital, when surgery may be required at any time.
- Use of intravenous anesthesia for minor surgical interventions.
- Installation of a catheter for women in labor at the beginning of labor so that there are no problems with venous access during childbirth.
- The need for repeated sampling of venous blood for research.
- Blood transfusions, especially multiple ones.
- The patient cannot feed himself orally, and then parenteral nutrition can be administered using a venous catheter.
- Intravenous rehydration for dehydration and electrolyte changes in the patient.
What is a venous catheter
The instrument is a thin hollow tube (cannula) equipped with a trocar (a hard pin with a sharp end) to facilitate insertion into the vessel. After administration, only the cannula is left, through which the medicinal solution enters the bloodstream, and the trocar is removed.
Before diagnosis, the doctor conducts an examination of the patient, which includes:
- Ultrasound of veins.
- Chest X-ray.
- MRI.
- Contrast phlebography.
How long does installation take? The procedure lasts on average about 40 minutes. Anesthesia at the insertion site may be required when inserting a tunneled catheter.
It takes about one hour to rehabilitate the patient after installing the instrument; the sutures are removed after seven days.
Advantages and disadvantages of the technique
The undoubted advantage of catheterization is the provision of quick access to the patient’s bloodstream. In addition, when placing a catheter, the need for daily puncture of a vein for the purpose of conducting intravenous drips is eliminated. That is, the patient only needs to install a catheter once instead of having to “prick” the vein again every morning.
Also, the advantages include sufficient activity and mobility of the patient with the catheter, since the patient can move after the infusion, and there are no restrictions on hand movements with the catheter installed.
Disadvantages include the impossibility of long-term presence of the catheter in a peripheral vein (no more than three days), as well as the risk of complications (albeit extremely low).
- Catheterization of the subclavian vein
Peripheral catheter
A peripheral venous catheter is installed for the following indications:
- Inability to take liquids orally.
- Transfusion of blood and its components.
- Parenteral nutrition (administration of nutrients).
- The need for frequent administration of drugs into a vein.
- Anesthesia during surgery.
PVK cannot be used if it is necessary to administer solutions that irritate the inner surface of blood vessels, a high infusion rate is required, and also when transfusing large volumes of blood
How to choose veins
A peripheral venous catheter can only be inserted into peripheral vessels and cannot be installed into central ones. It is usually placed on the back of the hand and on the inside of the forearm. Rules for choosing a vessel:
- Well visible veins.
- Vessels that are not on the dominant side, for example, for right-handed people should be chosen on the left side).
- On the other side of the surgical site.
- If there is a straight section of the vessel corresponding to the length of the cannula.
- Vessels with large diameter.
PVC should not be placed in the following vessels:
- In the veins of the legs (high risk of thrombus formation due to low blood flow speed).
- On the bends of the arms, near the joints.
- In a vein located close to an artery.
- In the median ulna.
- In poorly visible saphenous veins.
- In weakened sclerotic.
- In deep-lying ones.
- On infected skin areas.
How to put
Placement of a peripheral venous catheter can be performed by a trained nurse. There are two ways to grab it in your hand: longitudinal grip and transverse grip. The first option is more often used, which allows you to more securely fix the needle in relation to the catheter tube and prevent it from going into the cannula. The second option is usually preferred by nurses who are accustomed to performing vein punctures with a needle.
Algorithm for placing a peripheral venous catheter:
- The puncture site is treated with alcohol or an alcohol-chlorhexidine mixture.
- A tourniquet is applied, after the vein is filled with blood, the skin is taut and the cannula is installed at a slight angle.
- Venipuncture is performed (if blood appears in the imaging chamber, it means the needle is in the vein).
- Once blood appears in the imaging chamber, the needle stops advancing and must now be removed.
- If, after removing the needle, the vein is lost, reinserting the needle into the catheter is unacceptable; you need to pull out the catheter completely, connect it to the needle and reinsert it.
- After the needle is removed and the catheter is in the vein, you need to put a plug on the free end of the catheter, fix it on the skin with a special bandage or adhesive tape and flush the catheter through the additional port if it is ported, and the attached system if it is not ported. Rinsing is necessary after each infusion of liquid.
Caring for a peripheral venous catheter follows approximately the same rules as for a central one. It is important to maintain asepsis, wear gloves, avoid touching the catheter, change plugs more often and wash the instrument after each infusion. It is necessary to monitor the bandage, change it every three days and do not use scissors when changing the adhesive plaster bandage. The puncture site should be carefully observed.
Although catheterization of peripheral veins is considered less dangerous than central veins, if the rules of installation and care are not followed, unpleasant consequences are possible
Complications
Nowadays, consequences after a catheter occur less and less, thanks to improved models of instruments and safe and low-traumatic methods of their installation.
Complications that may occur include the following:
- bruises, swelling, bleeding at the insertion site;
- infection in the area where the catheter is installed;
- inflammation of the vein walls (phlebitis);
- formation of a blood clot in a vessel.
How is the procedure performed?
No special preparation is required for catheterization of both central and peripheral veins. The only condition when starting to work with a catheter is full compliance with the rules of asepsis and antisepsis, including cleaning the hands of the personnel installing the catheter and thoroughly cleaning the skin in the area where the vein puncture will be performed. Working with a catheter, of course, is necessary with the help of sterile instruments - a catheterization kit.
Catheterization of the subclavian vein
When catheterizing the subclavian vein (with “subclavian”, in the slang of anesthesiologists), the following algorithm is performed:
- catheterization of the subclavian vein
Place the patient on his back with his head turned in the direction opposite to the catheterization and with his arm lying along the body on the side of the catheterization,
- Carry out local anesthesia of the skin according to the infiltration type (lidocaine, novocaine) from below the collarbone at the border between its inner and middle thirds,
- Using a long needle, into the lumen of which a conductor (introducer) is inserted, make an injection between the first rib and the collarbone and thus ensure entry into the subclavian vein - this is the basis for the Seldinger method of catheterization of central veins (insertion of a catheter using a conductor),
- Check for the presence of venous blood in the syringe,
- Remove the needle from the vein,
- Insert a catheter into the vein using a guidewire and secure the outer part of the catheter with several sutures to the skin.
Jugular vein catheterization technique
The standard catheterization technique requires appropriate preparation, the position of the patient during manipulation, and the use of a set of instruments. To carry out the procedure, extensive experience of a specialist and the use of visualization techniques for internal structures are required.
Preparation
The patient first undergoes laboratory tests and a coagulogram. Then the features of the upcoming procedure are explained to him:
- target;
- necessity;
- technology;
- possible complications.
The patient signs voluntary informed consent. After this, he is taken to a sterile operating room. The patient is positioned in a supine position on the operating table. The head is turned in the direction opposite to the puncture area. The cervical spine is slightly extended.
If the patient’s condition allows, then to increase the blood supply to the vessels, he is placed in the Trendelenburg position - with the pelvis elevated, the angle of the body relative to the horizontal surface is 45°. Sometimes the legs are also elevated to expand the internal jugular vein, which has a diameter of 7 mm.
The skin on the neck is treated with an antiseptic solution from the angle of the lower jaw to the collarbone. Used as an antiseptic:
- Why do the veins in the arms hurt in the elbow bend?
- 70% alcohol solution;
- 2% chlorhexidine solution;
- 5% povidone iodide solution;
- iodoform;
- tincture of iodine.
A sterile napkin with a hole in the area of manipulation is placed next to the patient. The specialist prepares the CVC by rinsing it with saline and preparing it for installation.
Ultrasound scanning
The insertion point can be determined using the search puncture technique using a needle for intramuscular injection. A hollow needle is inserted into the vessel and a portion of blood is withdrawn. Based on its color and the intensity of blood flow, the type of vessel is determined - vein or artery. But this method has many limitations and can lead to mechanical damage. The use of external anatomical landmarks determined physically does not provide a 100% guarantee of safety, since their relationship with the target vessel can be variable.
Today, the “gold standard” for diagnosing the location of the jugular vein and adjacent structures is ultrasound. To carry out diagnostics, multi-frequency linear and microconvex sensors are used, the radiation frequency of which ranges from 7 to 10 MHz. They allow detailed visualization of surface structures located at a depth of 6-7 cm. These sensors have special marks on one side.
Of the main veins, the internal jugular vein is most accessible to ultrasound examination. A gel that increases the permeability of radiation is applied to the patient’s side of the neck, and a scan is performed, according to which the position of the vein and access points are marked. The use of color mapping during Doppler scanning facilitates diagnostic measures. The use of ultrasound can reduce the number of unsuccessful punctures and postoperative complications by 50%.
Local infiltration anesthesia
In children, puncture of the main veins is performed under general anesthesia. In adults, when inserting a CVC, infiltration anesthesia of the subclavian region on the right or left is used with local anesthetics, for example, a 0.25% solution of novocaine in a volume of 10 ml.
Installation of a catheter under ECG control
Installation of a catheter under ECG control allows you to optimize its position and reduce the likelihood of complications.
1. The catheter is washed with saline solution. A metal conductor is inserted into the catheter so that it does not extend beyond the catheter (some conductors have a special mark). Or a metal intramuscular needle is inserted through the catheter plug and the catheter is filled with a 7.5% sodium chloride solution. A plug is put on the needle;
2. Attach the chest lead “V” wire of the electrocardiograph or cardioscope to the needle or conductor using an alligator clip. And turn on the “thoracic abduction” mode on the recording device. Or connect the wire of the right hand to the distal electrode and turn on the second (II) lead on the cardioscope or cardiograph;
3. If the end of the catheter is in the right ventricle, we see a high-amplitude (5-10 times larger than usual) QRS complex on the monitor screen. Slowly tightening the catheter, we see a decrease in the amplitude of the QRS complex, but the P wave remains very high, which indicates that the catheter is in the atrium.