In the Russian Federation, 7% of adults suffer from chronic heart failure (CHF). Every year, even in conditions of treatment in a specialized hospital, up to 12% of patients with clinically significant CHF die. The only thing that can help a patient in the terminal stage of this disease is a heart transplant.
Not everyone who needs surgery lives to see it, but since Dr Christian Barnard's team performed the world's first human-to-human heart transplant 46 years ago, there has at least been hope for recovery.
Background
The successes of transplantology are associated with the development of two independent areas of medicine: the improvement of surgical techniques and anesthesia methods, on the one hand, and the achievements of immunology and pharmacology, on the other. The first ensured the successful completion of operations, and the second ensured the successful course of the postoperative period.
First steps
Back in the 16th century, the Italian surgeon Gasparo Tagliacozzi, after a series of unsuccessful experiments with skin transplantation from person to person, presented to the public the successful result of autotransplantation (transplantation of the recipient’s own organ, in this case skin). In 1596, he described his observations of the "strength and power of individuality" in De Curtorum Chirurgia per Insitionem (Replacement Surgery by Transplantation).
However, the idea of organ transplantation aroused widespread interest only 300 years later, when surgeons began practical experiments en masse. Once again faced with the problem of rejection, they enriched medicine with three important conclusions: cross-species organ transplants (xenotransplantations) are always unsuccessful; transplants between members of the same species (allogenetic transplants) in most cases, too, and repeated organ transplants between the same donors and recipients accelerated rejection; if there was a blood relationship between the donor and the recipient, the likelihood of a favorable outcome of the operation increased significantly, and transplantation of one’s own organs (autotransplantation) was almost always successful.
The first successful transplantation described in the literature dates back to the 2nd century AD: the Indian surgeon Shushrata performed a skin graft during rhinoplasty.
And in the 3rd century, according to the chronicles of the Roman Catholic Church, Saints Damian and Cosmas transplanted the limb of a recently deceased Ethiopian to the Roman deacon Justinian, who had lost his leg from gangrene.
dog's heart
In 1905, in a series of experiments on organ transplantation, the turn came to the heart. The first transplantation of the heart of a donor dog onto the vessels of the neck of a recipient dog was carried out by surgeon, biologist and pathophysiologist Alexis Carrel and physiologist Charles Guthrie, Americans of French origin. The donor heart worked for 2 hours.
In 1933, the American physiologist Frank Mann and his colleagues repeated Carrel’s experiment and showed the possibility of a heterotopically (that is, placed in an atypical place) transplanted dog heart functioning for up to 8 days (the dog’s own heart remained in place and continued to work).
Soviet surgeons also kept up with the times. The most significant contribution to the experimental foundations of heart transplantation in the USSR was made by Vladimir Petrovich Demikhov. From 1946 to 1955, in several hundred experiments, he developed 24 (!) variants of the surgical technique of heterotopic heart transplantation into the chest. In some experiments, the donor heart effectively provided blood circulation to the recipient dog for more than 15 hours.
Fighting ischemia
The most obvious problem that stood in the way of surgeons was ischemia: in conditions of insufficient blood flow, both recipient tissue and donor hearts were damaged. Transplantation cannot be performed in a short time, so surgeons and anesthesiologists began to look for ways to extend the operation time. This is how methods of controlled hypothermia were developed and artificial blood circulation (CPB) machines were designed.
Controlled hypothermia can reduce blood loss and also prolong surgery time without increasing the risk of tissue ischemia.
In 1953, American surgeons Wilford Neptune and Brian Cookson and their colleagues performed the first transplantation of the cardiopulmonary complex of a dog under conditions of deep hypothermia (during the operation, the temperature in the room was maintained at about minus 4 ° C).
In 1957, Americans William Webb and Heather Howard repeated this experiment, connecting the recipient dog to an infrared apparatus. They later reported transplantation under the same conditions of an isolated heart. They performed nine anastomoses between the aorta, pulmonary artery, pulmonary and vena cava. True, this transplant functioned for only 7 hours.
By the mid-60s, Norman Shumway and Richard Lower and colleagues from the Stanford University Clinic developed a heart transplantation technique that is still used today: using “local hypothermia” - local cooling to 18-21 ° C. From this point on, there was only one obstacle left for the successful operation - immunological rejection.
Reasons for rejection
In 1952, immunologists Jean Dausset (France) and Baruch Benacerraf (USA), together with geneticist George Snell (USA), discovered that the most important antigens involved in transplant rejection are major histocompatibility complex (HLA) antigens. For this discovery they were awarded the Nobel Prize in 1980.
There are about 150 variants of HLA antigens, and each person has six variants of such antigens on their cell membranes. Consequently, more than a trillion of their combinations are possible - the probability of two people existing with the same HLA antigen complexes is close to zero, of course, unless they are identical twins. Ideally, the donor and recipient have a mismatch of only one antigen out of six. Operations are also performed if the two do not match, but this increases the risk of developing immunological rejection.
In practice, determination of tissue compatibility - histotyping - is carried out using blood lymphocytes.
On the host side, the main effectors of transplantation rejection are cytotoxic CD8 T cells and CD4 T cells. The latter attract inflammatory cells (including macrophages) to the area of transplant rejection. Recognition of transplantation antigens occurs either directly on the transplant cells or in the nearest lymphoid tissue.
Antibodies in the recipient’s body (for example, those that appeared due to a previous whole blood transfusion) can also play a significant role in transplant rejection. By interacting with antigens of the endothelium of blood vessels penetrating the graft, they initiate the complement system and a cascade of reactions leading to blockage of blood vessels.
Immunosuppression
The first substances that were used to suppress the immune response were corticosteroids.
In 1948, the American doctor Philip Hench, using cortisone in the treatment of rheumatoid arthritis, showed that the drug has a pronounced anti-inflammatory effect. In 1952, American surgeon Roger Baker and his colleagues demonstrated that cortisone could also be used for immunosuppression after transplantation.
In 1962, Americans Willard Goodwin and Matt Mims first used azathioprine, an immunosuppressive drug with the greatest activity against T-lymphocytes, to prevent acute rejection of a transplanted kidney. Azathioprine in combination with corticosteroids was also planned for heart transplant patients.
Man's turn
The first human heart was transplanted in 1964. James Hardy and his colleagues transplanted the heart of a large chimpanzee, weighing more than 43 kg, into a 68-year-old patient with severe coronary artery disease in the terminal stage of progressive heart failure. Initially, the graft worked satisfactorily, but an hour after the CP device was turned off, acute heart failure developed due to volume overload of the graft, and the patient died.
The first allogenetic human heart transplant was performed three years later in Cape Town by South African surgeon Christian Barnard, who trained under Norman Shumway. Dr. Barnard's team transplanted the heart of a 25-year-old girl who died in a car accident into a 55-year-old diabetic who had suffered three heart attacks and suffered from congestive heart failure. The transplantation was successful, but on the 18th day after the operation the patient died of bilateral pneumonia. A month later, a second donor heart transplant was performed in the same clinic, after which the recipient lived for a year and a half, dying from chronic rejection.
In the USSR, the first successful heart transplant was performed in 1987 by the famous transplantologist, academician of the USSR Academy of Medical Sciences Valery Ivanovich Shumakov (1931–2008).
The success of the first clinical experiment captivated the medical community, and surgeons around the world turned to solving the problem of heart transplantation. However, most patients died soon after the operation, and the interest of researchers began to fade: if in 1968 there were 100 heart transplants, then in 1970 there were only 18. The main cause of death remained rejection of transplanted organs.
Only four of those operated on between 1967 and 1973 lived with a new heart for more than a year; from 1974 to 1983, the one-year survival rate increased to 60%, but the five-year survival rate was only 21%.
Immunologists and pharmacologists get down to business
In 1983, clinical studies of a new immunosuppressant, cyclosporine, a non-ribosomal polypeptide obtained from soil fungi of the species Beauveria nivea, were successful. It was isolated in 1970 as part of a program to screen new antibiotics. In 1972, the Belgian immunologist Jean-François Borel discovered the ability of cyclosporine to inhibit the culture of lymphocytes in the absence of a general cytostatic effect. In the late 70s, British surgeon Roy Calne conducted the first tests of the effectiveness of cyclosporine after heart and kidney transplantation on experimental animals. Its introduction into widespread practice opened a new era in heart transplantation, as it made it possible to significantly prolong the life of patients after transplantation. In 1994, another new immunosuppressant, tacrolimus (FK-506), a macrolide produced by the actinomycete Streptomyces tsukubaensis, was approved for postoperative therapy. In 1987, Japanese immunologists Shinichi Sawada and Jen Suzuki discovered in in vitro experiments that tacrolimus was 100 times more potent than cyclosporine in suppressing the proliferation of T lymphocytes. In studies in rats, dogs, and primates conducted from 1988 to 1993, tacrolimus provided prevention of transplant rejection at doses 10 to 100 times lower than cyclosporine and with fewer side effects. However, modifications of cyclosporine developed at the same time had similar advantages.
Recent advances in immunosuppression are associated with poly- and monoclonal antibodies (we talked about this in detail in KS No. 5 (118) 2013, article “Pharmaceutical Advances: Monoclonal Antibodies”), which help prevent steroid-resistant rejection, which cannot be stopped even by pulse therapy with methylprednisolone. tissues, which occurs with a frequency of 10–18%.
Currently, a three-component regimen of immunosuppressive therapy is used: cyclosporine A or tacrolimus in combination with methylprednisolone and mycophenolate mofetil (a cytostatic agent that is most effective against lymphocytes). Antilymphocyte antibody drugs (ALG, ATG, OKT-3) are used as induction therapy, as well as for severe signs of rejection or steroid-resistant rejection.
What complications can follow after transplantation?
The most well-known complications are well studied by clinicians and are therefore recognized at an early stage. These include:
- addition of infection;
- rejection reaction to transplanted heart tissues;
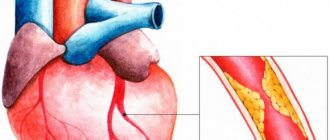
- narrowing of the coronary arteries, signs of ischemia;
- congestion in the lungs and lower lobe pneumonia;
- blood clot formation;
- arrhythmias;
- postoperative bleeding;
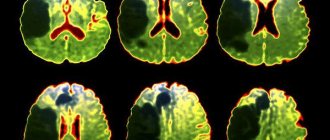
- dysfunction of the brain;
- Due to temporary ischemia, damage to various organs (kidneys, liver) is possible.
To suppress the rejection of donor tissue, the patient is prescribed strong drugs that affect the immune cells of the blood. This simultaneously creates favorable conditions for contracting any infection and cancerous degeneration.
Modern statistics
To date, more than 15,000 heart transplants have been performed worldwide. The 10-year survival rate for patients is about 50%. The highest mortality rate is in the first year after surgery (in different clinics - from 15 to 25%). The main causes of death are infectious diseases and Kaposi's sarcoma, which develop during immunosuppressive therapy.
Happy cases have also been described in which patients with a transplanted heart lived for more than 25 years. The world record holder was Tony Huseman, a patient at the Stanford University Clinic. He was operated on in 1978, the indication was dilated cardiomyopathy. After the transplant, he lived for 30 years and died at 51 from skin cancer.
From 2.7 to 4.5 thousand heart transplants are performed annually in the world. Of these, only about 100 operations are in Russia. The leader in the number of transplants is the United States: up to two thousand heart transplants are performed there annually.
Today in Russia there are 10 centers performing heart transplantation (all data are presented in accordance with information published in the journal “Bulletin of Transplantology” for 2009–2013).
Indications for heart transplant surgery
Diagnosis:
— cardiomyopathies of various origins;
- benign heart tumors;
- inoperable congenital heart defects (for example, left ventricular hypoplasia).
Clinical and functional characteristics of patients:
— chronic heart failure of NYHA class III-IV, resistant to drug therapy;
— ejection fraction of LVS < 30%;
— end-diastolic size of the left ventricle > 7 cm;
— LVA end-diastolic pressure > 20 mm Hg. Art.
— cardiac index (CI) < 2.5 l / (min × m2);
- refractoriness of ventricular tachyarrhythmias;
— expected survival of a potential recipient without heart transplantation < 6–12 months;
- age up to 55 years.
Absolute contraindications:
- persistent pulmonary hypertension (transpulmonary pressure gradient > 15 mm Hg, total pulmonary resistance (TPR) > 5 Wood units, systolic pressure in the pulmonary artery more than 60 mm Hg);
- acute infectious diseases and/or exacerbation of chronic ones;
- irreversible multiple organ failure;
- history of malignant neoplasms;
- thrombophlebitis;
- systemic diseases;
— obesity (> 30% of proper body weight);
- mental illness, alcoholism, drug addiction;
— lack of discipline in taking medications, non-compliance with hospital regulations.
Relative contraindications
- active diffuse myocarditis;
- insulin-dependent diabetes mellitus;
- peptic ulcer of the stomach and duodenum in the acute stage;
- history of cerebrovascular accident;
— infection with hepatitis C and hepatitis B viruses;
- atherosclerosis of the vessels of the lower extremities;
- limited family support.
First steps from natural to artificial
Mechanical pump
On April 4, 1969, a dying forty-seven-year-old patient was admitted to the Houston Heart Center with a diagnosis of heart failure. The operating surgeon undertakes a risky operation: he installs a mechanical pump for the patient, which temporarily performs the function of a failed organ. The installed pump pumps blood for him for three days. Thanks to this pump, the patient survives until he receives a donor organ. So the date is April 4, 1969. became the beginning of something like artificial heart implantation.
Challenges for the future
Only about 10–15% of patients awaiting heart transplantation survive to undergo it. One of the options for prolonging life until the time of surgery is the installation of an artificial heart. The average survival rate of patients with such a prosthesis is about a year. If during this time a suitable donor is not found, the patient may die, usually due to thrombotic complications. Unfortunately, the hemodynamic characteristics of artificial hearts are still far from perfect. The latest achievement in this area belongs to the German: the developers replaced the mechanical bearings of the device with a miniature turbine suspended in a controlled magnetic field. This made it possible to significantly reduce thrombus formation in the prosthetic heart.
Member of the Council of the European Society of Transplantology, Director of the Research Institute of Transplantology and Artificial Organs, Academician of the Russian Academy of Medical Sciences Sergei Gauthier in the “Bulletin of Transplantology and Artificial Organs” (No. 3, 2012) notes that the main reason why the required number of transplantations is not performed in our country is negative population's attitude towards posthumous organ donation. It should be noted that in Russia, unlike the United States and Western European countries, there is a presumption of consent: the law allows the removal of tissues and organs from a corpse if the deceased or his relatives have not expressed their disagreement.
An interesting technique that allows prolonging the life of patients with dilated cardiomyopathy awaiting a heart transplant was developed in 2002 by specialists from the Scientific Center of Surgery of the Russian Academy of Medical Sciences, headed by Doctor of Medical Sciences Alexei Koroteev. His team has successfully tested the following technique in practice: after a course of intensive cardiac therapy, the patient undergoes a spiral tomography to create an accurate three-dimensional computer model of the heart. Then a mesh is sewn from a special polyester material, Dacron, based on an individual dummy. During subsequent surgery, the mesh is placed over the living heart, preventing further dilatation.
The search for effective therapy for postoperative complications is still relevant. Most of them (infections, Kaposi's sarcoma, kidney and liver damage, as well as the rapid development of atherosclerosis of the coronary vessels of the graft) develop due to the constant use of immunosuppressants.
Perhaps someday these problems will be avoided, for example, by “growing” a patient’s own heart in vitro from stem cells. In April 2006, scientists at the California Institute of Regenerative Medicine, led by Dr. Anthony Atala, reported successfully growing and transplanting bladder domes into patients. But no team of researchers has been able to grow structured tissue of the heart muscle, at least not yet.
What is done after a heart transplant?
The patient is transferred to the intensive care unit or intensive care unit. Here a heart monitor is connected to it to monitor the rhythm.
Artificial respiration is maintained until spontaneous respiration is completely restored.
When there is a sufficient volume of breathing movements, the endotracheal tube is removed, but oxygen is constantly supplied through a mask or nasal catheters
- Blood pressure and urine flow are controlled.
- Narcotic analgesics are indicated for pain relief.
- In order to prevent congestive pneumonia, the patient needs forced respiratory movements and antibiotics are prescribed.
- Anticoagulants are indicated to prevent thrombosis.
- Depending on the electrolyte composition of the blood, potassium and magnesium preparations are prescribed.
- Using an alkaline solution, a normal acid-base balance is maintained.
Sources
- Jessen NH., Jensen H., Helsper CW., Falborg AZ., Glerup H., Gronbaek H., Vedsted P. Cancer suspicion, referral to cancer patient pathway and primary care interval: a survey and register study exploring 10 different types of abdominal cancer. // Fam Pract - 2021 - Vol - NNULL - p.; PMID:33904928
- Li T., Ruan DG., Xu XY. . // Sheng Li Xue Bao - 2021 - Vol73 - N2 - p.263-274; PMID:33903888
- Pineda C., Matsumoto K. Types of the New World Stigmoderini (Coleoptera: Buprestidae) deposited in Natural History Museum, London Buprestidae: Buprestinae: Stigmoderini. // Zootaxa - 2021 - Vol4964 - N3 - p.zootaxa.4964.3.2; PMID:33903504
- Singh SM., Liverpool A., Romeiser JL., Thacker J., Gan TJ., Bennett-Guerrero E. Types of surgical patients enrolled in enhanced recovery after surgery (ERAS) programs in the USA. // Perioper Med (Lond) - 2021 - Vol10 - N1 - p.12; PMID:33902705
- Azman NI., Wan-Mustapha WN., Goh YM., Hassim HA., Selamat J., Samsudin NIP. Climatic conditions and farm practices affected the prevalence of Aspergillus section Flavi on different types of dairy goat's feed. // Int J Food Microbiol - 2021 - Vol347 - NNULL - p.109205; PMID:33901942
- van Wigcheren GF., Roelofs D., Figdor CG., Flórez-Grau G. Three distinct tolerogenic CD14+ myeloid cell types to actively manage autoimmune disease: Opportunities and challenges. // J Autoimmun - 2021 - Vol120 - NNULL - p.102645; PMID:33901801
- Raikova R., Krasteva V., Krutki P., Drzymała-Celichowska H., Kryściak K., Celichowski J. Effect of synchronization of firings of different motor unit types on the force variability in a model of the rat medial gastrocnemius muscle. // PLoS Comput Biol - 2021 - Vol17 - N4 - p.e1008282; PMID:33901164
- Zheng WL., Wang JW., Jiang AD., Rehman Khan SA., Yang XQ., Zhang X., Zhang ZY. Study on environmental performance evaluation of different linkage development types of the logistics and manufacturing industries considering the unexpected output. // J Air Waste Manag Assoc - 2021 - Vol - NNULL - p.; PMID:33900887
- Scharnweber K., Chaguaceda F., Eklöv P. Fatty acid accumulation in feeding types of a natural freshwater fish population. // Oecologia - 2021 - Vol - NNULL - p.; PMID:33900451
- Segal NL. Twin Types: Variations and Common Themes/Twin Research Reviews: Birth Weight and Brain Development; Twinning and Vocabulary Knowledge; Fetal Loss in Twin Pregnancy; Twin-Family Olympic Medal Winners/Human Interest: Young Twin Soldiers; Twin-Run Laundry; Male-Female Pair and Politics; Twin-Based Graphic Novel; Twin Sisters' Deliveries. // Twin Res Hum Genet - 2021 - Vol24 - N1 - p.89-94; PMID:33900160