Retinal hemorrhage is a visual disorder that occurs due to damage to the eye vessels. As a result of the development of pathology, bleeding occurs into the retina tissue.
Often the causes of hemorrhage are mechanical damage to the organ of vision (contusions that can occur due to a blow to the head, face, etc.); some serious diseases can also provoke the pathological process.
Root causes of hemorrhage:
- Arterial hypertension.
- Leukemia, anemia and other blood diseases.
- Intraocular tumors.
- Diabetes.
- Inflammatory pathologies of the choroid.
- Myopia in later stages of development.
- Systemic connective tissue diseases: vasculitis, scleroderma.
- Atherosclerosis and other diseases.
Strong screaming or coughing can also cause damage to the eye vessels. Retinal hemorrhage is sometimes diagnosed in women during labor during childbirth.
Cardio training and excessively intense sports can also cause bleeding in the retina.
Signs of retinal hemorrhages
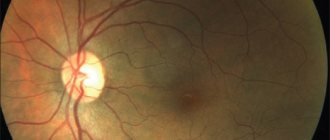
Hemorrhages can occur in any layers of the retina. The localization of pathology, as a rule, can be determined by a number of external signs. Thus, the outpouring of blood into the layer of nerve fibers looks like streaks, and into the area of the optic nerve head and macula - radial stripes. Blood in the middle layers of the retina appears as small, clearly defined circles of bright purple or red color. Preretinal hemorrhage, localized between the posterior hyaloid membrane of the vitreous body and the layer of nerve fibers, has the appearance of a large puddle (up to 4-5 diameters of the optic disc) with a horizontal level of separation of plasma and other blood elements. Subretinal hemorrhage, localized between the layers of the retinal neuroepithelium and pigment epithelium, is characterized by a darker color than retinal hemorrhage and the absence of clear contours. Choroidal hemorrhage appears as a dark red and even bluish tint. The most dangerous pathology is retrochoroidal hemorrhage, which is essentially arterial bleeding, otherwise expulsive hemorrhage.
Retinal hemorrhages usually occur in one eye, and the patient feels it by a sharp decrease in visual acuity.
Bleeding in the eye
Atherosclerosis
Diabetes
Fungus
26017 March 22
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Hemorrhage in the eye: causes of occurrence, what diseases it occurs with, diagnosis and treatment methods.
Definition
Hemorrhage in the eye is the accumulation of blood under the conjunctiva, in and between the membranes of the eye, in the chambers of the eye or in the vitreous body. Hemorrhage is caused by a violation of the integrity of the blood vessels of the eye.
The eyes continuously perceive, transform and send a huge amount of information to the visual analyzer.
The eyes are sensitive to changes in the body and, although quite protected, are easily damaged by external influences.
The eyeball is located in the cavity of the orbit - a bone frame; the orbit protects the eyeball from above, below, behind and on the sides. The eye in the orbit is located in fatty tissue - a kind of pillow. In front, the eyeball is protected by eyelids and eyelashes.
Eyeball
consists of three shells:
- external, represented by a convex transparent cornea, turning into the sclera - the frame of the eyeball;
- middle - in front is the colored iris, then the ciliary body, and in the back is the choroid itself, represented by a network of small arteries and veins. At the center of the iris is the pupil, which allows light to enter the eye. The ciliary body produces intraocular fluid, which is needed to maintain the shape of the eye and help with metabolism. The lens is attached to the ciliary body with the help of muscles and ligaments. By contracting and relaxing the muscles, the curvature of the lens changes, thus the eye “switches” the distance and focuses the image;
- the inner retina, which contains rods and cones that perceive light and convert it into an electrical impulse, which is then sent to the brain.
Vitreous body
fills the space between the lens and the retina and is a gel-like substance.
The eye has two spaces filled with intraocular fluid: the anterior chamber of the eye (between the cornea and the iris) and the posterior chamber of the eye (between the iris and the vitreous body, which contains the lens).
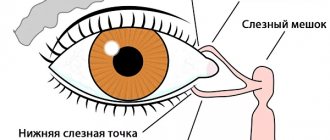
The cameras communicate with each other through the pupil. Conjunctiva
- This is the mucous membrane, it lines the inside of the eyelids and extends to the visible part of the eye. The conjunctiva is nourished by a network of very small vessels located directly underneath it. Externally, it is constantly washed with tears produced by the lacrimal glands.
Types of hemorrhages in the eye
Hemorrhages in the eye are divided depending on the place where the blood accumulates:
- With hyposphagma, blood accumulates between the conjunctiva and sclera due to damage to the conjunctival vessels. It looks like a bright red spot on the white of the eye. This is the least dangerous type of hemorrhage and does not lead to visual impairment, but you should be wary if it occurs regularly;
- With hyphema, blood flows into the anterior chamber of the eye. Hyphema has 4 degrees: 1st degree is characterized by filling the chamber by no more than 1/3, 2nd – by no more than 1/2, 3rd – by more than 1/2, but not completely, 4th – complete filling of the anterior chamber of the eye with blood. If blood reaches the pupil, the vision becomes blurred, vision decreases, and fear of bright light appears. With this type of hemorrhage, pain occurs;
- with hemophthalmia, blood fills the vitreous body. There are complete and incomplete hemophthalmos. Vision drops sharply, the degree of impairment of which depends on the volume of blood shed. A very dangerous type of hemorrhage that can lead to filling of the vitreous with connective tissue, permanent vision loss and possible retinal detachment;
- In retinal hemorrhages, blood accumulates just in front of the retina (preretinal hemorrhages), inside the retina (intraretinal hemorrhages), or just after the rod and cone layer (subretinal hemorrhages).
This is the most serious type of hemorrhage, most often leading to decreased or even loss of vision.
Possible causes of hemorrhage in the eye
The most likely causes of hemorrhage in the eye include:
- mechanical impacts, eye injuries, head injuries - the degree of damage depends on the force of the impact;
- intraocular operations;
- rupture of newly formed vessels;
- diseases and conditions that affect the composition and properties of blood, disrupting the blood clotting process (taking blood-thinning drugs, hematological diseases);
- diseases affecting the vascular wall (hypertension, atherosclerosis, diabetes mellitus);
- eye diseases: glaucoma (with increased intraocular pressure), high degree of myopia, retinal detachment, thrombosis (blockage) of the central retinal vein;
- various infections (viral, bacterial, fungal, etc.) leading to inflammation of the eye structures. Conjunctivitis (inflammation of the conjunctiva), iritis (irises), iridocyclitis (iris and ciliary body), chorioretinitis (choroid and retina), retinitis (retina only);
- increased intracranial pressure due to excess volume in the cranial cavity due to intracranial hematomas, brain tumors, cerebral edema;
- an increase in intra-abdominal and, as a consequence, venous pressure during severe physical exertion, debilitating vomiting, and during childbirth.
For non-penetrating blunt eye injuries
The cause of vascular rupture is a sharp increase in intraocular pressure, the same mechanism is triggered in glaucoma.
Newly formed vessels have a rather fragile wall; they can appear without good reason or to replace damaged ones, for example, in diabetes mellitus
. In addition, an increase in blood sugar levels leads to damage to the smallest vessels - capillaries.
For infectious diseases
the inflammatory process leads to increased vascular permeability, which can cause damage.
Blood diseases that most often lead to hemorrhages include hemorrhagic diathesis
.
This is a group of diseases in which the processes of stopping bleeding are disrupted.
For example, in hemophilia, there is a hereditary decrease in blood clotting factors, which prevents a blood clot from forming. In thrombocytopenia, there are not enough platelets to initially block the lesion. Oncological diseases of the blood. The most striking example is acute leukemia
. Tumor cells displace bone marrow cells, then enter the bloodstream and replace all healthy cells, including those responsible for stopping bleeding.
Atherosclerosis
manifested by the deposition of cholesterol plaques in blood vessels.
A constant or periodic increase in blood pressure
damages the inner layer of blood vessels - the endothelium, while the middle, muscular layer thickens, and the vessel loses its elasticity. These changes sooner or later lead to a violation of the integrity of any vessel.
Retinal disinsertion
from the choroid with hemorrhage occurs with eye injuries, inflammatory diseases of the retina, and disturbances in its nutrition. The risk of detachment increases in people with a high degree of myopia.
Symptoms of retinal detachment include a sharp decrease in vision, narrowing of the visual field or loss of a portion of the image, the presence of spots in front of the eyes, flashes of light.
Which doctors should you contact if there is a hemorrhage in the eye?
The treatment of hemorrhages in the eye is carried out by an ophthalmologist; to correct concomitant conditions, a consultation with a general practitioner may be required.
Diagnosis and examinations for hemorrhage in the eye
The doctor conducts a survey and examination of the patient and his eyes, determines visual acuity, measures blood pressure, intraocular pressure, studies the structures of the anterior chamber of the eye, and examines the fundus, if possible.
A number of additional examination methods may be required:
- ultrasound examination of the eye;
- electroretinography to assess the functional activity of the retina;
- general blood analysis;
Treatment
Treatment of retinal hemorrhages is carried out only in an ophthalmological hospital, where patients are required to be hospitalized.
As a conservative therapy, in the treatment of retinal hemorrhages, corticosteroids (subconjunctival injections), angioprotectors, antioxidants, non-steroidal anti-inflammatory drugs, diuretics, vasodilators and antihistamines are prescribed. Osmotherapy and laser coagulation are carried out (for large volumes).
The duration of treatment is usually 14 days, after which the hemorrhage will resolve and vision will improve.
Forecast
In most patients, retinal hemorrhages resolve well. Sometimes, in their place, delicate connective tissue moorings develop or mottling of the macular zone remains, as a result of which visual acuity sharply decreases. Therefore, to preserve vision, it is important to promptly contact a specialized eye clinic with doctors who know and can treat such diagnoses. We will be happy to help you - call to ask your questions and make an appointment.
You can find out the cost of basic diagnostic procedures and surgical procedures performed in our clinic in the PRICES section.
Prevention
Retinal hemorrhages may recur. To prevent such complications, mandatory medical examination and limitation of physical activity are recommended for 2-3 months after discharge from the hospital. For diabetic patients, therapy of the underlying disease, correction of the diet, as well as working and rest conditions are necessary.
In the medical department, everyone can undergo examination using the most modern diagnostic equipment, and based on the results, receive advice from a highly qualified specialist. The clinic provides consultations to children from 4 years old. We are open seven days a week and work daily from 9 a.m. to 9 p.m. Our specialists will help identify the cause of vision loss and provide competent treatment for identified pathologies.
You can find out the cost of a particular procedure or make an appointment at the Moscow Eye Clinic by calling 8 and 8 (499) 322-36-36 (daily from 9:00 to 21:00) or using the online registration form .
Diagnostics
If retinal bleeding is suspected, our ophthalmologists conduct a comprehensive examination of the patient.
- Visual acuity test, which shows the condition of the central zone of the retina;
- Perimetry (study of lateral vision), which allows assessing the condition of the peripheral areas of the retina;
- Tonometry – measurement of intraocular pressure.
With the help of a special examination - ophthalmoscopy (with a wide pupil) we will determine the location of hemorrhages, their number, and also identify thinned areas that pose a danger in terms of the emergence of new pathological foci (changed vessels).
An ultrasound examination gives an idea of the size of the detached retina (if this occurs against the background of hemorrhage) and the condition of the vitreous body. It is especially important for opacities of the lens, cornea or vitreous body, when it is impossible to see the retina.
Optical coherence tomography (OCT) allows differentiation of ocular structures measuring a few thousandths of a millimeter (micrometers) in size. It combines the capabilities of a scanner and a microscope. With this diagnostic test, the ophthalmologist can examine in detail the condition of all layers of the retina.
Our center has a unique opportunity to perform OCT angiography (OCTA) – i.e. examine the blood flow through the vessels of the retina and identify the place of blood exit for further laser treatment.
In terms of forecasts for vision restoration, electrophysiological studies (EPS) are used: an ophthalmologist determines the viability of the optic nerve and retinal nerve cells, which determines the appropriateness of treatment (including expensive ones).
Fig.2 Retinal optical coherence tomography (OCT) procedure
Retinal tumor
Retinal tumors are neoplasms of the retina that can be malignant or benign. Most often, tumors develop in childhood: in the first months of life in 20% of cases, in the first years in 55%. In 25% of patients, the process affects both eyes. The most common of retinal tumors are gliomas, which arise from the outer layer of the retina.
In the early stages, thickening of the retina occurs and this can only be determined by examining the fundus and ultrasound of the eye. After some time, the tumor takes up most of the eye. Due to the development of the tumor, the eyeball protrudes and its mobility is limited. Vision disappears.
The occurrence of the disease has a certain hereditary connection according to the incorrect dominant type.
Retinal tumors must be treated as soon as possible and in specialized ophthalmology departments of hospitals. If treatment is delayed, it can lead to irreversible consequences. Of the modern techniques for retinal tumors, the most effective are low-temperature (cryogenic) therapy and photocoagulation. Surgical treatment methods are organ-preserving.
Recovery period
Rehabilitation therapy begins from the first day after any type of intervention. Patients are recommended:
- Keep your eyelids clean using antiseptic solutions - chloramphenicol, furatsilin, chlorhexidine. They soak a cotton pad and wipe the eyelids several times a day. You should not wash your face with tap water until it is completely restored.
- Instill drops into the eyes with antiseptic solutions, regeneration stimulants, vitamins and antioxidants.
- Distribute eye strain. The operated eye should not be overly protected from stress. Doctors recommend removing the bandage from the second day after surgery, and you are allowed to read and watch TV for a short time.
- Use sunglasses when going outside.
- Refuse to visit the sauna, bathhouse, swimming pool and beach. You can take a shower very carefully so that water does not get on your face.
These measures will have to be observed for 4 to 30 weeks, depending on the treatment method used.
AGE-RELATED MACULAR DEGENERATION (AMD)
The most common cause of vision loss in people over 50 years of age. AMD affects the central part of the retina, the so-called macula.
The main risk factors for developing AMD are:
- Age over 50
- Cardiovascular diseases (atherosclerosis, hypertension)
- Genetic predisposition
- Gender (more common in women)
In the initial stages, the disease occurs unnoticed by the patient and can only be detected during an appointment with an ophthalmologist. With the progression of AMD and its transition to the so-called neovascular form, the patient may notice decreased vision, a feeling of curvature of lines, blurred and disappearing areas. If these symptoms occur, urgent consultation with a doctor is necessary.
Currently, the most effective method of treating AMD is intravitreal (i.e. inside the eye) administration of LUCENTIS, EYLEA (AFLIBERCEPT) - drugs that block the growth of new vessels under the retina. LUCENTIS, EYLEA (AFLIBERCEPT) can not only preserve, but also improve the vision of a patient with AMD. Treatment methods for AMD also include laser photocoagulation and photodynamic therapy.
Causes of the disease
The cause of the development of this vascular disease of the retina may be:
- atherosclerosis (every third disease of the choroid occurs for this reason);
- hypertension (every fourth disease);
- rheumatism;
- temporal arteritis;
- neurocirculatory dystonia, arrhythmia.
If treatment for this disease is not started promptly, complete loss of vision is possible.
1 Diagnosis and treatment of vascular diseases of the retina
2 Diagnosis and treatment of vascular diseases of the retina
3 Diagnosis and treatment of vascular diseases of the retina