Treatment under the compulsory medical insurance policy is possible!
Submit your application
Follow the news, subscribe to our social networks
Details
Carotid endarterectomy is surgery to remove plaque in the carotid artery and is used to reduce the risk of stroke. Treatment of atherosclerotic plaque on the walls of the vessels of the carotid arteries is impossible with the help of medications, since it is a dense rocky formation and is not able to dissolve.
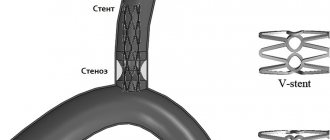
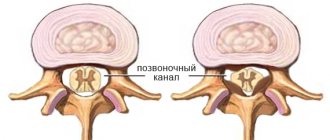
With atherosclerosis, plaques in the carotid arteries grow at the bifurcation (carotid bifurcation), where the common carotid is divided into the internal and external carotid. The plaque can gradually narrow the lumen of the vessel, a condition called stenosis.
Plaque rupture can lead to the formation of a blood clot in the vessel. Part of the resulting blood clot can break off and move through the lumen into the brain, where it blocks blood circulation and leads to the death of brain tissue - ischemic stroke.
Sometimes carotid bifurcation stenosis causes temporary symptoms of cerebrovascular accidents, which are called transient ischemic attack. TIAs are a sign of a high risk of developing a full-blown ischemic stroke and require the active attention of a vascular surgeon.
Even if the atherosclerotic plaque does not cause symptoms, a patient with stenosis is at high risk of developing an ischemic stroke. Based on the results of the studies, it was decided that a narrowing of the carotid bifurcation by 70% or more is a condition threatening the development of a stroke and requires endarterectomy or stenting.
Anesthesia during surgery
In the preoperative room, the patient is fitted with a urinary catheter, an intravenous catheter, and a monitor is connected to monitor the ECG during the operation.
In our clinic, for carotid endarterectomy, local anesthesia with a weak solution of lidocaine is most often used, but with the mandatory supervision of an anesthesiologist. Local anesthesia has enormous advantages over anesthesia in terms of preventing cerebral complications. Local anesthesia provides good pain relief throughout the operation.
A conscious patient is the best neurological monitor. To ensure the safety of carotid endarterectomy, it is necessary to understand how the brain responds to temporary compression of the carotid artery. For this we use local anesthesia. After identifying the carotid bifurcation, we temporarily clamp it, but maintain contact with the patient and give him a number of tasks. If the patient understands and performs the tasks well, then we perform the operation without using a temporary shunt. If we notice that the patient begins to “float away,” we use a special tube to perform the operation under a temporary shunt. Blood flows through this tube during clamping.
Description of the procedure
Carotid endarterectomy is a surgical intervention that involves clearing the inner layer of a vessel from atherosclerotic plaque. It is performed in cases where drug treatment is powerless or the risk of developing stroke is too high. Medicines are not able to have the desired effect when the atherosclerotic plaque occupies more than half the diameter of the carotid artery. Or if cholesterol closes the lumen of the vessel from several sides at the same time. In addition, the risk of stroke increases significantly in the presence of uncontrolled hypertension. In this case, the atherosclerotic plaque can break away from the endothelium at any time, regardless of its size. The result may be a blockage not of the carotid artery itself, but of its branches that supply the brain. As a result, an ischemic stroke develops.
How is the operation performed?
After anesthesia, a 5-10 cm long incision is made along the inner edge of the sternocleidomastoid muscle. The internal, common and external carotid arteries are isolated from the surrounding tissues and rise onto the supports.
During the operation, we perform a test with temporary clamping of the lumen for 3 minutes. The patient is asked to count to 100, shake hands, and move a leg. If there are no signs of circulatory failure in the brain, then we open the vessel and perform an endarterectomy. Otherwise, a special temporary shunt is installed in the lumen.
After arteriotomy, endarterectomy is performed - removal of the atherosclerotic plaque. The removal method may vary. With a longitudinal section, the atherosclerotic plaque peels off from the outer wall of the vessel. With the eversion technique, the internal carotid artery is divided transversely, after which it is everted, and the hard plaque moves away from the wall and comes off. After removal of the atherosclerotic plaque, the vessels are sutured. After a longitudinal dissection, to expand the lumen of the vessel, it is necessary to sew a special patch into the incision, but with the eversion endarterectomy technique, a patch is not required.
After starting the reconstructed artery, ultrasound monitoring of blood flow is mandatory. After this, the wound on the neck is closed with stitches after eliminating all possible bleeding. The skin is closed with an absorbable suture that will not need to be removed. Additionally, to control bleeding, a drainage tube with a bulb is installed, which is removed the next day.
Carotid endarterectomy – what is it?
Carotid endarterectomy (CAE) is a surgical method that involves removing atherosclerotic plaque from the lumen of the carotid artery to restore blood flow in it.
This operation is used to prevent stroke or TIA (transient ischemic attack).
Endarterectomy is an effective, reliable and safe method of surgical treatment, which has proven to be in demand for the treatment of patients with atherosclerosis of the brain and neck vessels.
The advantage of carotid endarterectomy is the use of local anesthesia and a reduction in the rehabilitation period.
Why is carotid endarterectomy performed?
It has been proven that the greatest cause of stroke is atherosclerosis of the carotid artery bifurcation (the common carotid artery is divided into the external carotid artery and the internal carotid artery); drug treatment alone is powerless.
Therefore, the development of unpleasant symptoms (head pain, dizziness, loss of consciousness, cognitive dysfunction) forces the patient to seek medical help.
And the most important thing is that carotid endarterectomy is the main way to prevent the development of fulminant stroke, which can cost the patient’s life.
Indications for use
The following indications exist for carotid endarterectomy:
- Artery stenosis greater than 60%.
- A history of two or more transient ischemic attacks.
- Bilateral retraction of the carotid arteries into the atherosclerotic process.
- Presence of unstable plaque or thrombus.
- To prevent recurrent stroke.
Contraindications
Carotid endarterectomy is a minimally invasive operation, but there are contraindications to its implementation:
- The person is over 70 years old;
- Ischemic or hypertensive disease of the third stage.
- Rapidly progressing stroke.
- Oncological disease.
- Acute and severe neurological pathology.
- Infectious disease in the acute stage.
- Severe liver or kidney failure.
- Alzheimer's disease.
Alzheimer's disease
What examinations are performed before surgery?
Before performing a carotid endarterectomy, the attending doctor conducts a thorough examination of the patient’s health:
- General blood test (to confirm the absence of anemia, acute inflammatory process);
- General urine analysis (in the absence of an inflammatory process in the kidneys);
- Biochemical blood test (study of lipid spectrum);
Coagulogram (assessment of the rheological function of the patient’s blood, the main thing is blood clotting):
- Electrocardiogram (assessment of the state of the heart muscle, rhythm and conductivity of the heart);
- Ultrasound scanning of the carotid arteries using a contrast agent (carried out to assess the location of the plaque, its lability, the degree of lumen occlusion, blood flow assessment);
- Computer angiography of the vessels of the head and neck (assesses the state of blood flow and pathological disorders in the carotid, vertebral artery, jugular vein);
- Computed tomography of the brain (an x-ray method of examining the brain with a series of complete images of all anatomical structures of the brain).
Complications during the procedure
Carotid endarterectomy is a gentle and safe operation, but as with any operation, all complications are taken into account. It is known that the occurrence of complications is associated with the following factors: smoking, high blood sugar.
Therefore, preoperative preparation includes the exclusion of all factors causing harm, treatment of chronic diseases or therapy to stabilize the patient’s health.
The following risks are possible when performing carotid endarterectomy:
- Development of stroke (risk less than 2%).
- Hypertensive or hypotensive crisis.
- Risk of blood loss.
- Risk of infectious complications.
- Damage to the nerves of the neck and face is possible (extremely rare).
Scheme of the operation
Types of surgery
Carotid endarterectomy is an operation whose technique has been improved by practicing surgeons over a long period of time.
Today, vascular surgeons use the following surgical techniques:
Name of type of carotid endarterectomyDescription
| Classic (straight, open) | It is used when there is an elongated atherosclerotic plaque in the lumen of the carotid artery. The operation lasts several hours using local or general anesthesia. During the operation, a binocular microscope and a magnifying glass are used. Stages of the operation: the surgeon cuts the artery above the site of the lesion, removes the vessel and introduces special equipment that removes the cholesterol plaque out (atherectomy). A special “patch” is installed in the place where the intervention was performed, the artery is sutured, and drainage tubes are installed if necessary. |
| Eversionnaya | It is used in the case of a short plaque (about 2 - 2.5 cm), when it is located in the initial zone of the internal carotid artery. A transverse incision is used, below the site of plaque damage to the artery. The carotid artery is turned inside out to cut off the affected inner layer. If necessary, anastomoses are established and the wound is sutured. |
| Removal of a section of artery with autoplasty | Used in case of extensive damage to the vessel by cholesterol plaques. The affected area is cut out, removed, stitched if possible, or replaced with an autograft. |
| Carotid endarterectomy with simultaneous coronary artery bypass grafting | It is used in the case of generalized forms of atherosclerosis, when the valves and arteries of the heart and carotid arteries are involved in the pathological process. |
What anesthesia is used?
When performing carotid endarterectomy, it is possible to use two methods of anesthesia, each of which has its own advantages:
Used to reduce the transmission of nerve impulses directly in the surgical area. In this case, the vascular surgeon can communicate with the patient to monitor his condition.
Mainly, local anesthesia is used for older people with chronic diseases of the cardiovascular or pulmonary system. Local anesthesia shortens the rehabilitation period.
- General anesthesia. The endotracheal anesthesia method is used to completely block nerve sensitivity, the patient sleeps during the operation. Nitrous oxide with oxygen is used, or intravenous infusion of narcotic drugs is performed.
General anesthesia
Postoperative rehabilitation
In the first hour after carotid endarterectomy, the patient is advised to keep his head straight. After 2 - 3 hours, you are allowed to take light dietary food and drink.
Depending on the method of surgical intervention performed, the patient may remain in the hospital for two to five days, under the supervision of medical workers.
During this period, clean treatment and care of the wound is very important; you must adhere to all antiseptic rules in order to avoid the occurrence of infectious complications.
The stitches are removed on days 5–7.
Before discharge, ultrasound monitoring of the surgical area is performed. The patient is contraindicated for physical activity and driving for one month.
A repeat ultrasound examination is required within 3 to 6 months.
After the operation, doctors prescribe the following medications for the patient’s rehabilitation:
- Anticoagulants . Anticoagulant drugs thin the blood and prevent the development of blood clots (Dicumarin, Warfarin, Phenilin, Sincumar).
- Analgesics . Used to relieve postoperative pain syndrome (Dexalgin, Baralgin).
- Drugs that improve microcirculation in the vessels of the brain (Cavinton, Trental).
- Nootropic drugs . Used to stimulate brain function: improving memory, mental activity, attention and concentration (Phesam, Vinpocetine, Berlition, Cerebrolysin, Actovegin).
- Antihypertensive drugs . Used to correct high blood pressure (Enalapril, Lisinopril).
- Non-steroidal anti-inflammatory drugs to reduce pain , inflammation, swelling.
- Antibacterial drugs . Antibiotics are used to prevent bacterial complications. Broad-spectrum antibiotics are used: cephalosporins, protected penicillins, macrolides.
Azitrox Actovegin Analgin Warfarin Ibuprofen Capoten Trental
Complications in the postoperative period
Despite the general safety of carotid endarterectomy, there is a possible risk of the following complications in the postoperative period:
- Infectious complications . The addition of a bacterial infection is possible during any surgical intervention, including after carotid endarterectomy. Compliance with the rules of personal hygiene, rules of asepsis and antisepsis by medical personnel and taking antibacterial drugs will help avoid the development of infection;
- Hematoma at the surgical site . Taking anticoagulant drugs contributes to the development of bleeding and subcutaneous hematomas. If the formation is large, there may be a risk of compression of the neurovascular bundle, breathing problems and infection. Surgical correction and discontinuation/reduction of the anticoagulant dose are required, which is considered on an individual basis;
- Injury to the vagus or hypoglossal nerve
Possible complications
Eversion carotid endarterectomy in our clinic is a safe intervention. We noted serious complications in the postoperative period only in 0.5% of patients. The following complications sometimes occur after surgery:
- Stroke during or after surgery develops for various reasons. Most often, this may be thrombosis of the reconstructed artery or embolism (transfer of a piece of plaque) to the cerebral vessels. The patient should be closely monitored in the early postoperative period to notice neurological problems as early as possible and take action. The incidence of these complications in our clinic was 0.5%.
- Bleeding from the surgical area is potentially life-threatening, as the hematoma can compress the trachea and cause suffocation. Installing drainage allows you to suspect this complication in time and take action.
- Damage to the hypoglossal or recurrent nerve is a consequence of inaccurate technique during surgery. This complication is manifested by loss of voice or deviation of the tongue and difficulty eating and speaking. We have not encountered this in our practice.
Contraindications for surgery
Despite the benefits of surgical interventions, in some cases they cannot be performed. Like other operations, carotid endarterectomy also has contraindications. Reviews from patients suffering from atherosclerosis make it clear that many different examinations are performed before surgery. Only after the doctor is convinced that there are no contraindications, the patient begins to be prepared for surgery. Carotid endarterectomy is prohibited in the following cases:
- Uncontrolled by medications (decompensated) hypertension.
- Extensive acute cerebrovascular accident.
- Unstable angina or recent myocardial infarction.
- Acute heart failure.
- Recently suffered a stroke.
- Chronic circulatory failure of 2 and 3 degrees.
- Alzheimer's disease.
- Severe oncological diseases.
Prognosis in the postoperative period
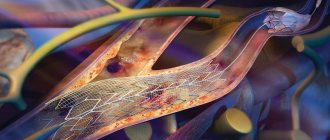
After successful surgery, the risk of stroke is reduced by 5-7 times. The patency of the carotid artery remains satisfactory in most patients for many years. To prevent thrombotic complications, blood thinning drugs (Plavix, aspirin), drugs to lower blood cholesterol levels, and changes in diet and lifestyle are prescribed. However, some patients may develop repeated narrowing in the endarterectomy area - restenosis. For timely diagnosis of restenosis, we examine our patients with ultrasound every year, and if restenosis is detected, we prescribe MSCT of the vessels of the neck and head. Detection of restenosis of the internal carotid artery forces the surgeon to suggest re-intervention. Most often, to correct such pathology, we use endovascular intervention without incisions - balloon angioplasty and stenting. The effect of such treatment lasts for a long time.
Monitoring for carotid stenosis
If you have been diagnosed with plaques in the carotid arteries, you should regularly undergo ultrasound examination of the carotid arteries.
Most patients, even with significant carotid stenosis, are asymptomatic. The first manifestations of carotid artery stenosis may be symptoms associated with a stroke, micro-stroke, TIA (transient ischemic attack) such as: weakness, numbness in one limb, half of the body, slurred speech, drooping corner of the mouth. Carotid artery stenosis can be detected accidentally during a routine ultrasound examination, during an appointment with an ophthalmologist, or after a stroke. Sometimes symptoms of carotid artery disease can include: tinnitus, episodes of loss of consciousness. Neck pain is usually not a symptom of carotid artery disease.
Recommended Research
- A generally accepted non-invasive research method is duplex angioscanning of the carotid arteries. This method can determine the location of narrowing of the arteries, if any, characterize the atherosclerotic plaque, and the degree of narrowing of the arteries;
- An alternative method is radiological (computed tomography ,
magnetic resonance angiography, X-ray contrast angiography), used to determine the presence, extent and degree of stenosis.