Manipulations and operations
Varicocele (varicocele; lat. varix, varicis - swelling in the veins, ancient Greek kēlē - tumor) is called varicose veins of the spermatic cord, which is a consequence of the obstructed outflow of venous blood through the system of the internal testicular and other veins draining the testicle. Varicocele is one of the most common diseases among the male population and is diagnosed in 10-15% of all men. The presence of a varicocele in a man most often does not affect his general well-being; many men do not even suspect that they have varicose veins in the scrotum. An active examination of the patient to establish a diagnosis of varicocele is carried out during an examination for infertility, since varicocele is one of the common causes leading to the absence of children in a marriage. If you take all men with infertility, then varicocele is detected in 40% of them. Moreover, with secondary male infertility (in the presence of their own children or a history of pregnancies, but with difficulties in conceiving at the present time), varicocele occurs in 80% of men.
Causes of varicocele
Inside any vein there are valves that prevent blood from flowing back down and allow blood flow to be directed only towards the heart. This happens because the muscles, when contracting, direct the blood flow towards the heart, and when relaxing, the valves begin to work, which block the lumen of the vein, like a door leaf, preventing the reverse flow of blood. The cause of varicocele development is the congenital absence of valves in the veins of the testicles, or their weakness. As a result of this defect, venous blood returns back to the scrotum and accumulates in its veins, causing them to expand. Thus, the greater the pressure in the veins of the scrotum, the more pronounced the varicocele.
Symptoms of varicocele
The course of varicocele is usually asymptomatic, does not cause any concern to the man and does not threaten his life. You can easily live your whole life with a varicocele and not even know about its presence. Sometimes a painful form of varicocele occurs, when a man is bothered by pain in the testicular area from the side of the varicocele. Almost always, varicocele is left-sided. Very rarely, varicocele is detected on both sides. Due to the anatomical features of the structure of the human body (the spermatic vein on the left side ends on the left renal vein at a right angle (90°), blood from the spermatic vein on the right bypasses the renal vein and enters directly into the inferior cava, which reduces venous pressure), a varicocele develops on the right extremely rare. If you have a right-sided varicocele, you must be examined for a formation in the right kidney that impedes venous outflow. With pronounced varicocele (varicocele IV degree), dilated veins in the scrotum area are visible to the naked eye.
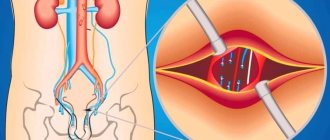
Gonadal vein embolization
We are talking about thrombosis of a damaged vein. A special catheter is inserted through a puncture of the vein in the thigh; it is gradually brought to the renal and then to the spermatic vein. Using contrast, the doctor determines which vessels need to be turned off. Using a catheter, a substance is injected that embolizes and “turns off” pathologically dilated veins.
Embolization requires virtually no downtime because the entire operation is performed through a small puncture. This is an effective and modern treatment method.
The choice of treatment method for varicocele depends on the patient’s wishes, his state of health, and the availability of medicine.
To receive treatment for varicocele at the highest level, contact the Urology Clinic named after R. M. Fronshtein of the First Moscow State Medical University named after I.M. Sechenov (State Urology Center). September 9, 2020
Akopyan Gagik Nersesovich - urologist, oncologist, doctor of medical sciences, doctor of the highest category, professor of the department of urology of the Federal State Autonomous Educational Institution of Higher Education First Moscow State Medical University named after. THEM. Sechenov
Clinic of Urology named after R. M. Fronshtein of the First Moscow State Medical University named after I.M. Sechenov invites you to an appointment with experienced urologists. To get an appointment with a qualified specialist, just fill out a short online application. Be sure to fill out all the fields, including a brief description of the symptoms (the “Information” column), specify whether you are interested in a secondary or primary appointment.
Pay attention to the “Attach file” button - it allows you to immediately send medical documents to the doctor in electronic form. This may include images, tests and other information that will be important to determine the diagnosis.
Still have questions? Call us by phone or! On a weekday, you can come for a consultation with a doctor within a few hours after filling out the online application. Do not delay visiting a specialist if you are concerned about your genitourinary health!
Degrees of severity of varicocele
Varicocele I degree: enlargement of the veins of the pampiniform plexus, detected only during the Valsalva maneuver or instrumentally (ultrasound, Doppler sonography); Varicocele II degree: dilated veins of the pampiniform plexus are visible to the naked eye only when standing, they are not palpable in the lying position, there is a palpable enlargement of the venous plexus, the size of the testicle and its condition remain unchanged; Varicocele III degree: visually visible enlargement of the veins of the pampiniform plexus in a standing and lying position; Varicocele IV degree: dilated veins of the testicle and spermatic cord are visible to the naked eye in a standing and lying position; the testicle on palpation has a changed consistency and is reduced in size; In most cases, varicocele develops during puberty, quickly reaches a certain degree and does not progress further. It is extremely rare that one degree of varicocele passes into another (for example, with increased physical activity).
Indications and contraindications for surgery
The only indication for this operation is varicocele - any degree of dilation of the veins along the spermatic cord of the testicles. But the need for intervention is determined by the attending physician based on the general clinical picture of the patient.
Surgeons argue about the time when surgery is necessary. Some experts recommend surgery at the earliest stages of the disease, because the longer it develops, the higher the risk of infertility. Others point out that infertility, in principle, accompanies the disease in most patients, regardless of its stage. In addition, surgery does not always improve sperm parameters. This means that there is no urgency in surgical intervention. But do not forget that each case is unique and only the attending physician can give an accurate recommendation.
The list of contraindications is small, but quite serious. Ivanissevich's operation is impossible if:
- the patient has severe pathology of one or more internal organs;
- there are acute infectious diseases;
- skin diseases, in particular in the area of surgery;
- have a urinary tract infection;
- there are blood pathologies.
Pathologies of internal organs are a contraindication until the patient’s condition becomes stable or a complete recovery occurs. As for skin lesions, the verdict is clear: before surgery, both the disease itself and its consequences must be eliminated.
Treatment of varicocele
There is no conservative treatment for varicocele. The only treatment for varicocele is surgery.
A varicocelectomy is performed (removal of varicocele, ligation of veins for varicose veins of the scrotum). There are many different types of surgical removal of varicocele, the most common of them: varicocelectomy according to Ivanisevich’s method, microsurgical varicocelectomy according to Marmar, microsurgical varicocelectomy according to Goldstein (for recurrent varicocele).
INDICATIONS FOR SURGICAL TREATMENT OF VARICOCELE:
- Spermatogenesis disorders (deterioration of sperm quality)
- Pain syndrome
- Sperm DNA fragmentation
- Reduction in testicular volume by more than 15% compared to a healthy one (without varicocele)
Pros and cons of the Ivanissevich method
The Ivanissevich operation is almost never used in modern urological surgery, since the technique is very outdated and has a large number of disadvantages :
- high incision on the stomach;
- it is necessary to cut the aponeurosis and abdominal muscles;
- long healing period;
- high percentage of varicocele recurrences;
- There may be testicular atrophy if the testicular artery is accidentally ligated.
The only advantage that can be highlighted is the low cost of the operation . But believe me, it's not worth it. In our practice, we use only modern methods of surgical intervention for varicocele - Marmara operation and microsurgical operation.
Operation Ivanissevich
The Ivanissevich operation is currently the traditional method of surgical treatment of varicocele. This type of treatment for varicocele was proposed by Ivanissevich himself in 1924. Ivanissevich's operation consists of ligating the testicular vein at the level of the intersection with the iliac vessels. The Ivanissevich operation can be performed in an inpatient or outpatient setting, both under local anesthesia and intravenous anesthesia. Ivanissevich's operation begins with treatment of the surgical field and a 4-5 cm incision in the anterior abdominal wall in the left iliac region at the level of the anterior superior iliac spine parallel to the course of the inguinal canal (retroperitoneal section). In fact, the incision is similar to that for an appendectomy, but from the opposite side, since most often the varicocele is found on the left, and the appendix on the right. Next, access is made to the retroperitoneal space and in the retroperitoneal tissue, the testicular vein and, if possible, all its additional branches are isolated, ligated and crossed. The surgical wound is sutured tightly, and a sterile bandage is applied on top. The Ivanissevich operation is performed on both adult patients and children. But since it is quite traumatic, it is necessary to consider other surgical treatment options. In addition, after Ivanisevich’s operation, the probability of varicocele recurrence reaches 40% of cases. This is due to the peculiarities of the surgical technique and the anatomical structure of the patient: the possibility of intraoperative visualization of the testicular vein only over a short distance and the possibility of a branch of the testicular vein originating above or below the surgical site.
Laparoscopic method
Laparoscopy is a modern endoscopic technique that has some advantages over the Ivaniseevich operation. With the help of a laparoscope, the surgeon becomes able to access not only the affected vein, but also small vessels that are not visible during standard surgery.
Three small incisions are made in the abdominal cavity, into which a tube with a camera at the end is inserted. The doctor monitors the process through a monitor.
Advantages
this method:
- low morbidity and short period of stay in the clinic (no more than 2-3 days);
- the ability to immediately ligate both veins of the testicle with bilateral varicocele;
- treatment of asymptomatic varicocele;
- relapses are practically excluded (no more than 2%);
- good tolerance;
- good cosmetic effect.
The laparoscopic method has proven itself well in the re-treatment of varicocele, if the Ivanissevich operation was performed previously and resulted in a relapse.
During the manipulation process, the surgeon even sees small vessels that cannot be ligated during a conventional operation, which is why the effect is so high.
However, this operation has a disadvantage
– the patient is put into medicated sleep, and this is not suitable for all patients. People with cardiovascular disorders and other pathologies are often not recommended to undergo operations of this nature.
Treatment of varicose veins of the testicular veins by laparoscopic method is prohibited in case of acute inflammatory or oncological diseases of the abdominal organs. This treatment is not given to patients who have a history of several similar interventions.
Operation Marmara
It is performed under both local and intravenous anesthesia. After treatment, a skin incision is made in the groin area (subinguinal access), the spermatic cord is subsequently isolated from the surrounding tissues and taken onto a Farabeft retractor, using 3.5x binocular loupes, microdissection of the spermatic cord is performed using microsurgical instruments (the outer and inner fascia of the spermatic cord are opened in the longitudinal direction; the testicular artery/arteries, lymphatic vessels and the vas deferens with its accompanying artery and vein are isolated. All veins are ligated with 4/0 non-absorbable suture material and resected (veins with a diameter of less than 1 mm are coagulated and divided). As a result, the spermatic cord contains contains the testicular artery/arteries, the vas deferens with its artery and vein and lymphatic vessels. Control of hemostasis. The spermatic cord is immersed in the surgical wound on its bed. The wound is sutured, an aseptic bandage is applied to the skin. This operation is less traumatic because it does not occur muscle dissection, recurrence and complication rates are minimal.
The Marmara operation is considered the gold standard in the treatment of varicocele.
Goldstein operation (for recurrent varicocele)
Microsurgical varicocelectomy according to the Goldstein method is performed in a similar way to the Marmara operation, except that first the testicle is dislocated from the scrotum with a finger into the surgical wound, followed by coagulation or ligation of the dilated veins (depending on the size) with non-absorbable suture material 4/0 and resection, all venous the collaterals of the external spermatic vein are also intersected (since in approximately 10% the cause of relapse is ileospermatic reflux). The testicle returns to the scrotum. In the future, the technique is similar to the Marmara operation technique.
Positive and negative aspects of this technique
For a long time, Ivanissevich’s operation remained practically no alternative for the removal of varicocele (not counting identical techniques, for example, Palomo), but in modern practice new, less traumatic methods of treatment have appeared using micro-access, magnifying imaging equipment, a computer and other innovations.
These operations are becoming increasingly popular, and classical abdominal interventions are gradually becoming a thing of the past. However, the simplicity and accessibility of surgery according to Ivanissevich keeps this method in the top of frequently used ones.
For the sake of objectivity, we will indicate the positive and negative aspects of such therapy, starting with the positive ones:
- The lowest price;
- A regular operating room is suitable for the intervention; there is no need for special equipment;
- The technique does not require special specialized training (unlike laparoscopy or sclerotherapy);
- Suitable for removing varicocele of any degree and regardless of the patient’s age.
However, the negative aspects significantly outweigh, which forces progressive clinics to abandon the use of this technique and switch to more effective methods for eliminating varicocele.
Among the main negative characteristics we highlight the following:
- Highly traumatic;
- Significant likelihood of developing postoperative complications or relapse (30-40%);
- Treatment requires hospitalization from 8 to 14 days, depending on the individual characteristics of the patient;
- Sutures are removed on the 8th day;
- Long rehabilitation period. Full recovery is possible no earlier than six months;
- Severe pain syndrome;
- The operation leaves a large scar (similar to an appendicitis scar).
The procedure is quite painful
POSTOPERATIVE PERIOD
— To relieve pain after any operation for varicocele, the patient is prescribed analgesics; — to avoid the development of infectious diseases, antibacterial prophylaxis is carried out; — to be able to tension the spermatic cord, a special support bandage is required; - when suturing a wound with absorbable suture material, there is no need to remove the sutures, otherwise the sutures are removed after approximately nine to ten days; — over the next six months it is necessary to exclude heavy physical activity; — ultrasound control (Doppler examination) of the scrotal vessels after surgery for varicocele must be performed after 6 months; — if the indication for surgery for varicocele is infertility, you can plan conception immediately after the sutures are removed. If pregnancy has not occurred within 3 months after surgery for varicocele, it is necessary to perform a control spermogram and contact a urologist with the result.
Preparation
When preparing for surgery for varicocele, the following studies are mandatory:
- blood and urine tests;
- ultrasound examination of the scrotum;
- spermogram;
- hormonal studies;
- coagulogram;
- infectious disease test;
- fluorography;
- ECG.
If the patient does not have chronic pathologies other than varicose veins, then an examination by a urologist, consultation with an anesthesiologist and a physician’s opinion are sufficient. If any diseases are detected, the patient is referred for additional consultation to an appropriate specialist.