Introduction
Aortic arch obstruction or interruption often requires emergency surgical intervention in the neonatal period [1]. Although the results of reconstructive operations on the aortic arch have been significantly improved, long-term results still cannot be called completely satisfactory. There is enough data indicating that in 16-28% of patients, even in the absence of anatomical obstruction, arterial hypertension and systemic vascular dysfunction persist in the long term [5, 11]. As a rule, such patients have structural, functional and macroanatomical disorders [3, 8, 9]. The complex of these disorders leads to early atherosclerosis of the aorta and coronary arteries, aneurysms of the aorta and peripheral arteries, and 18% of patients operated on (including at an early age) die before the age of 34 years [14].
Hypoplasia of the descending thoracic and abdominal aorta: surgical treatment
Back to program
Arakelyan V. S., Papitashvili V. G., Gidaspov N. A., Abdulgasanov R. A.
Federal State Budgetary Scientific Institution NTsSSKh im. A.N. Bakuleva;
Hypoplasia of the descending thoracic and abdominal aorta is a rare disease with a wide variety of morphological features. The term hypoplasia is used for prolonged narrowing of the aorta in any part of it. The most common clinical manifestation of aortic hypoplasia is severe uncontrolled hypertension in children and adolescents. Often existing stenoses of the renal and mesenteric arteries require complex reconstructive interventions.
Methods:
For 13 years, the Scientific Center for Sports Agriculture named after. A.N. Bakulev RAMS, with a diagnosis of hypoplasia of the descending aorta, 23 patients were operated on (15 female patients and 8 male patients; age range, from 3 to 41 years), 15 patients had stenosis of the renal and mesenteric arteries. Preoperative imaging of the aorta, celiac trunk, superior mesenteric artery, and renal arteries was performed in all patients using CT-AG. In 16 cases, aorto-aortic bypass was performed (from the thoracic to the abdominal aorta, or from the proximal segments of the descending thoracic aorta to the distal), in 4 patients, resection of the aorta with prosthetics was performed, and in 4 cases, plastic surgery of the affected area with a patch. Reconstruction of the renal arteries was performed in 15 cases, reconstruction of the celiac trunk and superior mesenteric artery was performed in 6 patients. In 3 cases, 2-stage surgical treatment was required (the second stage included reconstruction of the right renal artery).
Results:
Immediate results after surgery: mortality - 0%, postoperative complications (abdominal ischemia, renal failure requiring dialysis) - 0%. Early reoperations were 8.7% (postoperative bleeding in 2 patients). Most patients were discharged with complete regression of the symptom complex. The average follow-up period was 13 years and included 82.6% of patients. Survival rate over 10 years was 100%, freedom from repeated reconstruction was 100%.
Conclusions:
Aortic hypoplasia refers to non-atherosclerotic and non-inflammatory narrowing of the aorta and is a rare pathology. Surgical treatment of thoracic and abdominal aortic hypoplasia shows a low risk of complications and mortality. Reconstruction of the renal and mesenteric arteries is a necessary measure to prevent ischemic complications and treat arterial hypertension.
Material and methods
The study included 62 patients
(44 boys and 18 girls) aged 55±14 days (from 1 to 98 days), with an average body weight of 3.5±1.2 kg (from 2.3 to 4.5 kg), operated on at the Center for Pediatric Cardiac Surgery NNIIPK them. acad. E.N. Meshalkin in the period from 2004 to 2014. All patients underwent surgical correction of congenital anomaly of the aortic arch under conditions of artificial circulation.
Reconstruction of the arch was performed using two methods: using a xenopericardial patch (group 1, 32 patients) and using end-to-side anastomosis (group 2, 30 people). Variants of aortic arch pathology and associated anomalies are presented in Table. 1.
The degree of aortic hypoplasia was assessed using the Z-score. In the long-term period, all patients were examined at least twice by a cardiologist. Also, in the postoperative period, repeated MSCT was performed to assess the size and proportionality of growth of various segments of the aortic arch, identify recoarctation syndrome and study the shape of the postoperative aortic arch.
Surgical procedure.
All patients were operated on under general combined anesthesia. Blood pressure monitoring was performed in the right radial and femoral arteries. Cerebral saturation was assessed using the INVOS 5100 device (Somanetics, USA) throughout the entire procedure. To perform artificial blood circulation, Dideco Lilliput I systems (Sorin, Italy) were used.
A median sternotomy was used to access the heart and great vessels. For systemic perfusion, three methods of aortic cannulation were used: 1) direct cannulation of the ascending aorta - 11 (17.5%) cases; 2) cannulation of a heparinized polytetrafluoroethylene prosthesis GoreTex 3.0-3.5 mm, which was anastomosed with the proximal part of the brachycephalic trunk - 29 (46.8%) cases; 3) double cannulation: one cannula was inserted into the ascending aorta or heparinized prosthesis, the other through the ductus arteriosus into the descending aorta for perfusion of the lower half of the body - 22 (35.5%) observations. In all cases, separate cannulation of the vena cava was performed. If necessary, a left ventricular drain was placed in the right upper lobe pulmonary vein.
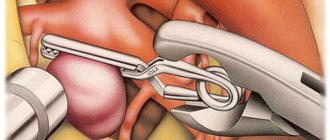
Deep hypothermic circulatory arrest was carried out when the rectal temperature reached 20 °C. All patients underwent antegrade selective brain perfusion through a GoreTex prosthesis anastomosed to the brachycephalic trunk. The first stage involved reconstruction of the aortic arch using one of two methods: expansion of the narrowed section using a xenopericardium patch or formation of an end-to-side anastomosis between the descending and ascending aorta. The technique of this operation was proposed by S. Fraser and R. Mee [4], and also modified by H. Rajasinghe et al. [13]. The second stage, after resuming artificial circulation, was to eliminate intracardiac defects. After disconnection from artificial circulation, modified ultrafiltration was performed.
Statistical analysis.
Statistical processing of the results was carried out using the Statistica 6.0 program.
Continuous variables were expressed as means ± standard deviations. To compare values with their normal distribution, t
-test was used.
p
value ≤0.05 was considered statistically significant.
Coarctation of the aorta in the fetus
And again about congenital heart defects (CHD): most of them are extremely dangerous, as they threaten the very life of the newborn. The incidence of congenital heart defects ranges from 10 to 13 cases per 1000 newborns, and up to 50% of newborns with congenital heart disease in early infancy die from them.
We remind you that statistical figures show a low percentage of detection of congenital heart disease based on the results of a screening ultrasound examination - only 30%, and in specialized institutions, prenatal centers - a little better - only about 50%.
This is due to the great difficulties in diagnosing microscopic defects (remember - at 12 weeks of pregnancy the size of the fetal heart is only a few millimeters, at 18-20 weeks - i.e. the time of the second pregnancy screening, it is about 1-1.4 cm. The research doctor must be truly a virtuoso , a real professional, to detect a tiny defect or other anomalies in the fetal heart beating at a frequency of 140-150 beats per minute.It is clear that the requirements for diagnostic equipment are as high as for the professionalism of the doctor.
One of the virtually undiagnosed fetal heart pathologies during pregnancy is coarctation of the aorta.
The Latin term "coarctatius" means "narrowed, compressed." The frequency of the defect is 6 - 8% of all congenital heart defects.
During pathological examination in these cases, areas of stenosis between the aortic isthmus and the descending aorta, varying in degree of narrowing, are most often found.
The pathogenesis of the disease is not fully understood. A combination of this pathology with aortic stenosis or aortic valve insufficiency, cardiac septal defects, transposition of the aorta and pulmonary trunk, etc. has been noted. Bicuspid aortic valve and mitral valve abnormalities are common.
♥ Extracardiac pathology during coarctation of the aorta can manifest itself as a diaphragmatic hernia, as well as Turner syndrome.
♥ When coarctation of the aorta and tubular hypoplasia of the aorta are combined, the latter in the thoracic region becomes narrow and has a small lumen diameter.
The degree of coarctation is also different: from slight (safe for life) to sharp narrowing, sometimes - complete closure of the lumen - aortic atresia, and then the life of the child is then possible only due to bypass circulatory pathways: open oval window, open ductus arteriosus, ventricular septal defect and etc. Children with less pronounced coarctation survive.
♥ Narrowing of the aorta is much more common than is diagnosed, as in mild cases of coarctation there are few or even no symptoms. The defect is often discovered by chance during an echocardiography examination of a child for another reason.
♥ In clinically significant cases, a rough systolic murmur with trembling is heard over the upper part of the sternum on the right, which is carried out in the carotid arteries, with an accent of the second tone over the aorta.
♥ The ECG shows signs of overload on the left side of the heart, depending on the degree of stenosis. Echocardiography demonstrates the location and degree of narrowing of the aorta, as well as the consequences of this condition - left ventricular hypertrophy, dilation of the heart chambers, manifestations of heart failure.
♥ Blood pressure measurement demonstrates an increase in pressure in the arms and a weakening or even absence of pulsation in the legs
Subjective symptoms and complaints in sick children are as follows: a feeling of flushing and heat in the head, arms, upper body, tinnitus, dizziness, excessive pulsation of the heart, sometimes headache, a feeling of weakness, chilliness and coldness in the legs, fatigue when walking . These symptoms depend on hypertension in the carotid and subclavian artery systems and hypotension in the arteries of the lower body. The function of the internal organs of the abdominal cavity and kidneys is often impaired due to a lack of blood supply. The prognosis for life without surgical treatment for clinically pronounced symptoms of the disease is unfavorable.
What is the conclusion from this short article? We recommend conducting a thorough echocardiographic examination (ECHOG) of the fetus at the optimal timing of the 2nd screening. It is this study that allows, in the presence of a fetal heart defect, to detect it with a much greater probability than the statistics above demonstrate. Since congenital heart disease can be the only independent disease of the fetus, it is clear that there is no need to look for special indications for fetal echocardiography.
There is nothing more tragic than a child's illness. And it is not difficult to conduct a timely, detailed examination of the heart of a fetus or newborn. And if everything is fine, let the huge stone of worries and responsibility fall from your shoulders. And if a defect is discovered, then you will have time to agree on the place of delivery, and the volume, type, and urgency of providing the necessary medical care to your child.
In the photo from Dr. R. Shukhnin’s own practice:
Ultrasound, 2nd pregnancy screening. Color flow control and B-study mode. The fetal thoracic aorta is normal. The thoracic aorta is clearly visualized throughout its entire length without visible changes, and this is confirmed by color spectrography of the blood flow in it.
Ultrasound, 2nd pregnancy screening. ED mode. The area of coarctation (arrow) of the aortic arch is clearly visualized. A diagnosis of coarctation of the aorta was made.
Echocardiography of an infant.
Aortic arch. A slight narrowing of the isthmus of the aortic arch (marked by an arrow) is a common, clinically silent finding. Congenital heart disease Fetal ultrasound Fetal echocardiography Echocardiography congenital heart disease congenital heart disease of the fetus Dopplerography Doppler echocardiography coarctation of the aorta tubular hypoplasia of the aorta ultrasound of pregnancy Pyatigorsk ultrasound of the fetal heart Pyatigorsk ultrasound of the heart Pyatigorsk
Why does vice occur?
Any malformation is formed in the fetus if a woman is influenced by negative environmental factors during pregnancy - smoking, alcoholism, drug addiction, ecology and unfavorable background radiation. However, genetic (hereditary) factors play an important role in the development of the child’s heart, as well as existing chronic diseases in the mother or past infectious diseases, especially in the early stages of pregnancy (influenza, herpes infection, chickenpox, rubella, measles, toxoplasmosis and many others) .
But, in any case, when any of these factors influence a woman in the early stages of pregnancy, the normal processes of ontogenesis (individual development) of the heart and aorta, formed during evolution, are disrupted.
So, in particular, the period of pregnancy of approximately 2-6 weeks is especially vulnerable to the fetal heart, since it is at this time that the formation of the aorta occurs.
Treatment
In the event that the right aortic arch is isolated and is not accompanied by any clinical manifestations after the birth of the child, the defect does not require surgical treatment. All you need is a monthly examination by a pediatric cardiologist with regular (every six months - once a year) ultrasound of the heart.
When combined with other heart defects, the type of surgical intervention is selected based on the type of defect. Thus, with tetralogy of Fallot, surgery is indicated in the first year of a child’s life, carried out in stages. At the first stage, palliative (auxiliary) shunts are applied between the aorta and the pulmonary trunk to improve blood flow into the pulmonary circulation. At the second stage, open heart surgery is performed using a cardiopulmonary bypass machine (ACB) to eliminate pulmonary stenosis.
In addition to surgery, cardiotropic drugs that can slow the progression of chronic heart failure (ACE inhibitors, diuretics, etc.) are prescribed for auxiliary purposes.