04 Jun 2021 at 14:36 MRI of the heart in Tushino 2610
Coarctation of the aorta
is a congenital narrowing (up to complete closure) of the aorta, which is accompanied by hemodynamic disturbances with a characteristic clinical picture. Coarctation in most cases is located in the area of the aortic isthmus. This disease is not a congenital heart defect, since the pathology develops outside the organ, affecting the aorta.
Signs of coarctation of the aorta
With this disease, patients become restless, they are often disturbed by severe headaches, coughing, shortness of breath, and also develop insomnia. Tinnitus, as well as dizziness and nosebleeds are other signs of coarctation of the aorta. As the disease develops, the heart rate increases, severe fatigue appears, and in some cases weakness in the legs is felt.
A characteristic symptom of the development of the disease is disproportionate development of the torso. Relative to the chest, the lower limbs develop much more slowly. During the examination, a fairly strong heartbeat can be detected. With coarctation of the aorta, an increase in blood pressure in the upper extremities is observed.
Get a free consultation Consultation does not oblige you to anything
Coarctation of the aorta - diagnosis of the disease
Despite the ease of diagnosis, this disease does not appear so often. Increased pressure and increased pulsations in the upper body can serve as the first signal. When diagnosing the disease, electrocardiography is mandatory, thanks to which it is possible to determine the degree of load of all parts of the heart. X-ray examination allows you to view the pulmonary vascular pattern. Adult patients undergo cardiac catheterization, as well as angiography to determine the degree of pulmonary hypertension. MRI of the heart and blood vessels also allows us to identify features of the course of the disease.
Prevention
Since the causes of coarctation of the aorta are not fully understood, experts suggest that certain genes are responsible for the tendency to develop the disease. To prevent the disease it is necessary:
- undergo examination at a medical genetic center: determine the risk of developing the disease;
- undergo a preventive examination by a cardiologist;
- to refuse from bad habits.
- reduce physical activity.
Causes of aortic stenosis
The cause of the development of aortic stenosis may be the following diseases: 1. Rheumatism, 2. Protracted septic endocarditis, 3. Atherosclerosis, 4. Infectious diseases. 5. Congenital pathology In addition to true organic stenosis of the aortic mouth, relative stenosis is distinguished, when the aortic valves are not changed, and the ascending part of the aorta is sharply expanded due to arterial hypertension or as a result of loss of elasticity of the aortic wall (atherosclerosis). Aortic stenosis creates a significant obstacle to the flow of blood from the left ventricle into the systemic circulation only if the area of the aortic opening is reduced by more than 50%. Maintaining even 10-20% of its normal value is compatible with life. The lengthening of the systole (contraction time) of the left ventricle and the increase in pressure in its cavity, as a compensatory reaction to the narrowing of the aortic mouth, causes the development of pronounced hypertrophy (increase in muscle mass) of the left ventricle. With no other defect does such significant hypertrophy of the left ventricular myocardium develop as with stenosis of the aortic mouth. Since the powerful left ventricle takes part in the compensation of aortic stenosis, the defect occurs for a long time without circulatory disorders. A long period of compensation is a feature of this defect.
Treatment of coarctation of the aorta
Treatment of this disease is carried out only through surgery after consultation with a doctor. The operation is prescribed if a difference in systolic pressure in the legs and arms is detected, which is more than 50 mm Hg. Art. In cases of severe arterial hypertension and decompensatory cardiac activity, infants are required to undergo surgery. Effective methods of surgical treatment of the disease include:
- vascular plastic surgery using vascular prostheses;
- bypass surgery of a narrowing of a certain area of the aorta;
- stenting of aortic coarctation with balloon angioplasty.
After the operation, the patient is prescribed antihypertensive drugs. The attending doctor selects them individually.
Rehabilitation
After the operation, the patient requires rest. In addition, you must adhere to a diet that includes low-fat foods. If you have this heart disease, it is also recommended to limit the amount of salt you consume. Physical activity needs to be reduced. During the rehabilitation process, it is necessary to give up bad habits. Smoking and drinking alcohol must be avoided.
Make an appointment Make an appointment and get a professional examination at our center
Publications in the media
Coarctation of the aorta (CA) is a congenital segmental narrowing of the aorta in the area of its isthmus. Since CA is often combined with other defects, four types of CA are distinguished: type I - isolated CA; Type II - CA in combination with a patent ductus arteriosus (PDA); Type III - CA in combination with VSD; Type IV - CA in combination with other congenital heart defects.
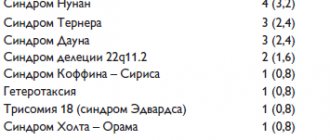
Statistical data • CA makes up 7.5% of all congenital heart diseases in infancy • The ratio of male to female is 2:1–2.5:1 • In 60–70% of cases it is combined with other congenital heart defects: in infants, CA in 70% of cases combined with PDA, in 60–70% — with tubular hypoplasia of the aortic arch and isthmus, in 53% — with VSD, in 14% — with aortic stenosis, in 3–5% — with mitral valve defects, in 6% — with hypoplasia of the left heart • In 26% of children, other severe extracardiac developmental anomalies are detected, 14% of them are not treatable.
Etiology • Skoda's theory - obliteration of the PDA with involvement of the adjacent area of the aorta • Anderson-Becker theory - in the presence of the falciform ligament of the aorta, narrowing of the aortic isthmus during obliteration of the PDA occurs in its area • Rudolf's hemodynamic theory - normal narrowing of the aortic isthmus in the embryonic period, caused by a small the volume of blood passing through it due to the PDA; persists after birth in the presence of septal defects, when a reduced volume of blood continues to flow into the ascending aorta (therefore, CA is never combined with stenosis of the left ventricular outflow tract, in which there is high volumetric blood flow in the ascending aorta in the embryonic period).
Pathogenesis • There are two modes of blood circulation - proximal and distal to the narrowing •• Proximal circulation is characterized by volume overload of the left parts of the heart, their hypertrophy, dilatation and the development of systolic arterial hypertension •• Distal circulation is characterized by systolic arterial hypotension and the development of collateral blood flow through the system of intercostal and internal mammary arteries • Diastolic blood pressure in both modes is the same, when combined with a PDA, diastolic blood pressure is reduced in the proximal region, when combined with aortic valve stenosis, systolic blood pressure can be the same in the proximal and distal regions, when combined with a VSD, systolic blood pressure in the proximal region can be any • From -due to left ventricular hypertrophy and the development of relative coronary insufficiency, 15–20% of infants develop myocardial fibroelastosis • With the preductal type (narrowing of the aorta proximal to the PDA), depending on the degree of stenosis, blood discharge is possible both from the pulmonary artery into the systemic circulation and in the opposite direction (see The ductus arteriosus is open), and pulmonary hypertension is usually low and reversible • With the postductal variant, there is a large discharge of blood from the aorta into the pulmonary artery, the rapid development of pulmonary hypertension and decompensation of circulatory failure in a large circle, especially when combined with VSD • Arterial hypertension with CA is caused not only by a mechanical obstruction, but also by a high level of renin secretion, the cause of which is unclear, because Collateral circulation has been shown to be sufficient to maintain adequate renal perfusion (see also Patent ductus arteriosus, Aortic valve stenosis, Ventricular septal defect).
Clinical picture
There are five periods in the natural course of aortic coarctation.
• I period - critical, age up to 1 year, symptoms of circulatory failure (usually in the pulmonary circulation), also depending on concomitant anomalies; high mortality rate.
• II period - adaptations, age 1–5 years, reduction of symptoms of circulatory failure, which by the end of the period are usually represented only by shortness of breath and increased fatigue.
• III period - compensation, age 5–15 years, various variants of the course, often asymptomatic.
• IV period - relative decompensation, age of puberty, increasing symptoms of circulatory failure.
• V period - decompensation, age 20–40 years, symptoms of arterial hypertension and its complications, severe circulatory failure in both circles.
Complaints • In young children, the symptoms of circulatory failure in the pulmonary circulation predominate (shortness of breath, orthopnea, cardiac asthma, pulmonary edema) • In the postductal variant, coronary artery disease can manifest as cardiogenic shock when the PDA is closed • In older children, the symptoms of arterial hypertension predominate (impaired cerebral blood supply, headaches, nosebleeds) and, much less frequently, decreased blood flow distal to the narrowing of the aorta (intermittent claudication, abdominal pain associated with intestinal ischemia) • Symptoms of associated anomalies - see patent ductus arteriosus, aortic valve stenosis, ventricular septal defect.
Objectively • The predominance of physical development of the shoulder girdle with thin legs (athletic physique) in children of the older age group • Pulsation of the intercostal arteries • Cyanosis in the combination of coronary artery disease with congenital heart disease, accompanied by discharge of blood from right to left • Weakening of pulsation in the arteries of the lower extremities • Difference in blood pressure in the upper and lower extremities more than 20 mm Hg • Delay of the pulse wave in the lower extremities compared to the upper extremities • Increased apical impulse • Increased pulsation of the carotid arteries • Systolic murmur over the base of the heart, carried along the left edge of the sternum, in the interscapular region and on the carotid arteries • Systolic click expulsions at the apex and base of the heart • Auscultatory symptoms may be completely absent • Symptoms of associated anomalies - see Patent ductus arteriosus, Aortic valve stenosis, Ventricular septal defect.
Instrumental diagnostics
• ECG •• Signs of hypertrophy and overload of the right (60% of infants), left (20% of infants) or right and left (5% of infants) sections •• Ischemic changes in the final part of the ventricular complex (50% of infants without fibroelastosis and 100% of children with myocardial fibroelastosis), in 15% of cases there are no signs of myocardial hypertrophy •• See also Patent ductus arteriosus, Aortic valve stenosis, Ventricular septal defect.
• Chest X-ray •• Bulging of the pulmonary artery arch •• Cardiomegaly •• In older children, the shadow formed by the aortic arch and its dilated descending part may take the form of the number 3. The same changes give the barium-filled esophagus the appearance of the letter E • • Usuration of the ribs, caused by pressure from dilated intercostal and internal thoracic vessels, is found in patients older than 5 years •• See also Patent ductus arteriosus, Aortic valve stenosis, Ventricular septal defect.
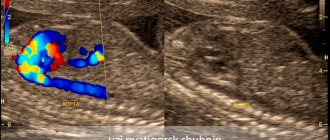
• EchoCG •• Myocardial hypertrophy and dilatation of the heart cavities depend on the degree of narrowing of the aorta and associated anomalies (see Patent ductus arteriosus, Aortic valve stenosis, Ventricular septal defect) •• In a third of cases, the aortic valve is bicuspid •• Visualization of stenosis, determination of its degree ( see Aortic valve stenosis), anatomical variant (local, diffuse, tandem) and relation to PDA •• Measurement of transstenotic pressure gradient •• Transesophageal echocardiography is performed in children of older age groups and adults.
• Probing of the cardiac cavities, ascending, descending parts of the aorta and its arch •• Increase in systolic blood pressure in the prestenotic part and decrease in the post-stenotic part of the aorta •• Measurement of the transstenotic pressure gradient •• When combining the preductal variant of coronary artery with PDA - decrease in paO2 and blood oxygen saturation in post-stenotic part of the aorta •• Adults and children with types II–IV defects undergo tests with aminophylline and oxygen inhalation to determine the prognosis regarding the reversibility of pulmonary hypertension •• See also Patent ductus arteriosus, Aortic valve stenosis, Ventricular septal defect.
• Ascending aortography, left ventriculography •• Visualization of stenosis, diagnosis of its degree and anatomical variant (local, diffuse, tandem) •• With an eccentric location of the lumen at the level of stenosis - post-stenotic dilatation of the aorta •• See also Patent ductus arteriosus, Aortic valve stenosis, Ventricular septal defect.
• Coronary angiography: performed in the presence of episodes of angina and positive results of stress testing, as well as in all women over 45 years of age, men over 40 years of age and all candidates for surgical treatment to exclude concomitant coronary artery disease.
Drug therapy. Prevention of infective endocarditis. When treating cardiogenic shock, standard regimens are used. In case of postductal or unclear variant of CA, even with a closed PDA, an infusion of PgE1 (alprostadil) 0.05–0.1 mg/kg/min is performed. After hemodynamic stabilization, emergency surgical correction is performed. In the treatment of arterial hypertension in adults, preference is given to ACE inhibitors and calcium antagonists. In the postoperative period, a temporary worsening of hypertension may develop, for which beta-blockers and nitroprusside are prescribed.
Surgery
• Indications •• All patients with coronary artery disease under the age of 1 year are subject to surgical treatment. •• If surgical treatment was not performed in infancy, it is recommended to operate on a child under 3 years of age, because at this age, due to the good elasticity of the aorta, plastic correction of the defect is possible without the need for prosthetic replacement of a segment of the aorta •• In adults - a transstenotic pressure gradient of more than 50 mm Hg •• Left ventricular dysfunction, regardless of the presence of clinical symptoms.
• Contraindications: irreversible pulmonary hypertension (with associated anomalies), severe concomitant pathology that threatens the patient's life, end-stage circulatory failure. Relative contraindications in adults are hypoplasia of the left ventricle and the inability to correct concomitant defects.
• Methods of surgical treatment •• Transluminal balloon dilatation is performed in case of local or tandem narrowing and the absence of pronounced fibrosis and calcification in the area of coarctation •• For children with non-extended stenosis, isthmoplasty is performed with a flap from the subclavian artery with simultaneous application of a carotid-subclavian anastomosis or resection of the stenotic area with reconstruction of the aorta end-to-end •• In case of extended narrowing or low elasticity of the aorta in older children and adults, isthmoplasty or resection is performed with replacement of the narrowed area with a synthetic prosthesis •• Elimination of associated defects - see Patent ductus arteriosus, Aortic valve stenosis, Ventricular septal defect.
Specific postoperative complications • Recoarctation • Paradoxical arterial hypertension • Spinal cord ischemia (0.4% of cases of prosthetics) • Ischemia of the left upper limb after isthmoplasty (in 0.1% of cases - ischemic gangrene) • False anastomotic aneurysm and dissecting aortic aneurysm (usually in adults with inadequate blood pressure control) • Abdominal syndrome caused by vasculitis of the branches of the mesenteric arteries (usually in adults with inadequate blood pressure control).
Prognosis • Depends on the age at which the correction was performed, as well as on the presence of other heart defects • In the natural course of the defect, in most cases, death occurs in the 2–4th year of life, 55% of patients die in the first year of life, more often during the neonatal period • Among the most common causes of death in children are heart failure (50%), intracranial hemorrhage (13%), aortic rupture (20%) • The average life expectancy of unoperated patients is about 30 years • The preductal variant of CA is more often accompanied by other congenital heart defects, which causes high natural mortality of infants • 80% of adults die from complications of arterial hypertension • Open operations have no advantages over balloon dilatation of the aorta, both in terms of immediate results and in terms of long-term restenosis • Postoperative hospital mortality in children under 1 year of age in I and II types of CA - 2-3%, with type III - 20-30%, with type IV - up to 58% • 5-year survival rate with types I and II of CA - 93-97%, with type III - 78.5% • The frequency of recoarctation within 5-7 years with isthmoplasty with a subclavian artery flap is 1-2%, with resection - 21-54%, with isthmoplasty with a synthetic patch - 25-51% • Hospital mortality in emergency operations - 30%.
Abbreviations. CA - coarctation of the aorta. PDA - patent ductus arteriosus.
ICD-10 • Q25.1 Coarctation of the aorta.
Treatment of aortic stenosis
— All patients, incl. and with minor aortic stenosis that does not have clinical symptoms are under close medical supervision - Patients with aortic stenosis without severe symptoms are recommended to be examined every 3-6 months - Echocardiography - every 6-12 months - All patients with aortic valve stenosis require prophylaxis endocarditis (antibiotics) before, for example, dental treatment or other invasive procedures (regardless of age, cause or degree of stenosis)
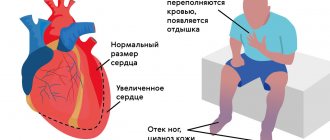
Symptoms of aortic stenosis
Aortic stenosis is more common in men, especially older men, as a result, for example, of calcium deposits on the valve leaflets. In young people, the most likely cause is congenital anomalies. Complaints in patients with aortic stenosis are determined by the cause of the defect, the nature and course of the disease that caused the defect, the severity and stage of development of the defect. At the stage of compensation of the defect, patients do not complain. The defect is most often discovered accidentally. In patients with more severe stenosis of the aortic mouth, during physical activity (less often at rest), there may be dizziness, a feeling of lightheadedness, fainting, increased fatigue, and compressive pain in the heart and behind the sternum. The combination of squeezing pain in the heart with dizziness and fainting is especially characteristic. The appearance of attacks of cardiac asthma and shortness of breath at rest indicates a significant decrease in the contractility of the left ventricle. Pallor of the skin is observed. Stagnation occurs in the pulmonary and then systemic circulation, which causes the appearance of acrocyanosis and edema.