doctor
One of the most difficult periods in a woman’s life is undoubtedly the period of cessation of the menstrual cycle, the production of estrogen and progesterone. Symptoms: temperature changes, night sweats, decreased libido, vaginal dryness, nervousness, sometimes depression, migraines and joint pain.
Stopping estrogen production leads to several disorders:
- Decreased levels of good cholesterol and increased levels of bad cholesterol, and as a result, increases the risk of cardiovascular disease
- Thinning of bone mass (decreased density), development of osteoporosis
- Many women approaching menopause notice unexplained weight gain and an increase in fat tissue, especially in the abdominal area, despite all attempts to lose weight
Moreover, with age, the incidence of obesity in them progresses, especially after menopause, against the background of a decrease in the secretion of ovarian hormones, the total amount of fat increases and is redistributed to the anterior abdominal wall, and the mass of muscle and bone tissue decreases.
An increase in body weight and the formation of abdominal obesity against the background of a deficiency of sex hormones is explained by changes in the energy balance and regulation of fat cells, enhanced by glucocorticoid stimulation in postmenopause, the resting metabolic rate decreases.
Due to the metabolic consequences of a long period of dysregulated energy balance, not only does the mass of adipose tissue increase, but also the amount of muscle tissue decreases. One of the main mechanisms of the influence of sex hormones on adipose tissue is a direct effect on the activity of lipoprotein lipase, the main enzyme regulating the accumulation of triglycerides in adipocytes.
In women of reproductive age, lipoprotein lipase stimulates estrogens in the adipose tissue of the thighs and buttocks, where the activity of this enzyme is higher than in the subcutaneous fat of the abdominal region.
As a result, lipids accumulate to ensure adequate energy reserves during pregnancy and lactation.
After menopause, lipoprotein lipase activity decreases, and adipocytes of the femoral-gluteal region decrease in size, and a relative redistribution of fat occurs.
How to reduce hot flashes and how to deal with excessive sweating?
To reduce the negative consequences of hormonal disorders during menopause, you need to take appropriate medications, adjust your diet, and adjust your work and rest schedule. However, that's not all. There are some simple rules to reduce the unpleasant symptoms of attacks:
- Avoid going to the bathhouse and sauna. Hot air in steam rooms causes excessive sweating.
- Spend less time outside on hot days, and also stay as far as possible from heat sources - fireplaces, stoves, heaters, bonfires.
- Stop smoking, eating hot, fatty and spicy foods, coffee, alcohol and sweets.
- A woman's diet during menopause should include more fresh fruits and vegetables, dairy products, cereals, wheat bran, chicken eggs, and nuts.
These products have a beneficial effect on female hormonal levels, which helps reduce the symptoms of menopause. It is also worth including foods rich in so-called phytohormones in your diet. In their composition they are close to human hormones, but are not as effective. Eat: coconut, soybean and olive oil, lentils, flax seeds, garlic, chickpeas, beans, barley, rye. - Drink at least 1.5 liters of water per day. Due to increased sweating during menopause, the body quickly loses fluid, so it must be replenished in a timely manner.
- Do not wear synthetic clothing. It is better to give preference to cotton, silk and linen items. The exception is fleece clothing: this artificial material dries quickly and provides the necessary moisture removal.
- Avoid outfits with high collars. Choose clothes with a neckline and cutouts near the neck.
- Change synthetic bedding to natural ones. This will help you sweat less while you sleep.
- If you experience intense hot flashes, you can carry a spare set of clothes with you. If you get very sweaty, you will have the opportunity to change clothes.
- Observe personal hygiene rules. To avoid the unpleasant odor of sweat, it is recommended to use a high-quality antiperspirant that prevents the appearance of unpleasant odor.
- Make time for rest, try to be less nervous and engage in static sports - Pilates, yoga, stretching, callanetics. During this difficult period, regular seaside holidays are highly desirable for the female body, but it is important to avoid hot months (July, August) and choose more comfortable and cooler ones - May, June and September.
Treatment of hot flashes during menopause
Menopause symptoms
Tides
Hot flashes are a sudden feeling of heat in the face, neck, chest and arms, which is accompanied by fever, sweating and a feeling of shortness of breath.
The skin may become red or covered with red spots. Often this may be accompanied by dizziness, nausea and tachycardia (rapid heartbeat). Tides are usually short-lived. Lasts from 30 seconds to 2-3 minutes.
Nocturnal hyperhidrosis
Severe night sweats are, in principle, considered one of the manifestations of hot flashes that occur during sleep. Again, the problem is a deficiency of female sex hormones, which have a direct effect on the thermoregulation center located in the hypothalamus. This part of the brain receives false signals that the body is overheated. As a result, mechanisms for releasing excess heat are activated and sweating occurs. It should be noted that hyperhidrosis during sleep can be a symptom not only of menopause, but also of certain diseases.
Irregular menstruation
The gradual decline of the hormonal function of the ovaries leads to menstruation becoming shorter, irregular and scanty. The interval between menstruation increases and can range from 40 to 90 days, or even more. This period is called perimenopause. Over time, periods stop. If they do not make themselves felt for at least a year, it means menopause has arrived.
Vaginal dryness
With age, metabolic processes in our body slow down, elasticity and tissue moisture decrease, and intimate areas are most sensitive to these changes. The walls of the vagina become flabby, cracks form in them, and there is a tendency to prolapse and prolapse of the pelvic organs. One of the symptoms of these changes is the sensation of a foreign body in the vagina. With age, all these troubles only increase. Before 45 years of age, only 15-30% of women know them, and after 50 years of age - already 40%.
Insomnia
Sleep problems during menopause are quite common. The same female sex hormones are to blame for this. Lack of estrogen, which causes hot flashes and night sweats (which interferes with restful sleep), is also accompanied by impaired absorption and metabolism of magnesium, a mineral that is responsible for muscle relaxation. And the lack of another hormone - progesterone - leads to insomnia. After all, progesterone is a natural relaxant; it calms, pacifies and improves sleep.
Mood swings
Changes in hormonal levels lead to disruption of the psycho-emotional state. Menopause symptoms such as tearfulness, anxiety, restlessness, irritability, and even aggressiveness appear.
Decreased sexual desire
According to statistics, about 80% of women between the ages of 50 and 60 remain sexually active. However, it should be noted that decreased sexual desire is one of the common symptoms of menopause. There are both physiological and psychological reasons for this. A symptom of menopause such as vaginal dryness has already been mentioned.
Brittle nails, thinning hair
Like most menopause symptoms, hair loss is caused by hormonal imbalances in the body. This is a fairly common problem that affects 50-75% of menopausal women. But not only hair suffers from a lack of estrogen. During this difficult period for the female body, nails can peel, become brittle and dry.
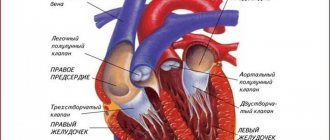
Heart problems
A natural decrease in the level of the female hormone estrogen can cause cardiovascular disease among menopausal women. The fact is that estrogen has a positive effect on the walls of blood vessels, helping to maintain flexibility and elasticity, which ensures free blood flow through the arteries.
Osteoporosis
One of the most dangerous symptoms of menopause. After menopause, overall bone mass decreases and bone tissue becomes porous. This leads to a risk of fractures, especially in the wrists, hips and spine.
Urinary incontinence
Bladder dysfunction is a fairly common symptom of menopause. A deficiency of female sex hormones can lead to weakening of the pelvic muscles responsible for bladder control, leading to unpleasant consequences such as urinary incontinence.
Weight gain
An increase in body weight often accompanies the approach of menopause. However, extra pounds are not always a direct symptom of menopause. Various factors play a role. For example, incorrect eating habits and love for fatty, high-calorie foods.
Muscle pain and headaches
A very common symptom of menopause is headache. It can be the result of changes in the tone of blood vessels (vasomotor disturbances), as well as weakness due to hot flashes, insomnia and stress. Another unpleasant symptom of menopause is muscle tension caused by impaired calcium metabolism in the body.
Memory problems
Mature women often complain of memory lapses and inability to concentrate. This is a fairly common symptom of menopause and is also associated with decreased estrogen levels. According to statistics, two thirds of menopausal women suffer from such “whims” of memory. All problems disappear as soon as hormonal fluctuations smooth out.
Allergy
It has been proven that women of menopausal age are especially susceptible to the development of allergic reactions and are more likely than others to experience exacerbation of existing allergies. The endocrine and immune systems are closely related, and the immune system can respond to hormonal changes with the appearance of new allergic reactions (most often, allergic rhinitis, asthma and dermatitis).
You can find out about the onset of menopause using a blood test.
- Blood test for follicle-stimulating hormone (FSH) . This hormone is produced by the pituitary gland and is responsible for the production of female sex hormones. With the onset of menopause, FSH continues to be released, but the ovaries no longer respond by producing estrogen in response. So an increase in FSH levels indicates menopause.
- Blood test for estradiol , which is the main estrogen during reproductive age. Accordingly, the cessation of ovarian function, which is characteristic of menopause, leads to a decrease in the level of estrogen in the blood.
- Blood test for luteinizing hormone (LH) . This hormone stimulates the final maturation of the follicle, its rupture and ovulation. During menopause, the level of luteinizing hormone in the blood is elevated.
If hot flashes, dizziness, emotional instability and other signs of menopause significantly reduce the quality of life and interfere with usual activities, the woman should consult a doctor. A gynecologist-endocrinologist will assess her condition and select hormone replacement therapy taking into account the characteristics of the body.
What to take for hot flashes during menopause?
Most often, doctors prescribe menopausal hormone therapy (MHT) to patients. Normalizing hormonal levels by taking such drugs not only reduces sweating, but also improves psycho-emotional state, helps cope with mood swings, increases performance and optimizes concentration.
However, it must be taken into account that drugs that compensate for the lack of estrogen can activate the launch of developing oncological diseases - in particular, breast, endometrial or ovarian cancer and aggravate chronic diseases and the risk of thrombosis. Therefore, treatment with hormonal drugs should occur exclusively according to the regimen drawn up by the doctor.
In recent years, it has become possible to replace the use of traditional tablet medications with the use of hormonal patches, gel forms, and intrauterine complexes.
They are considered less dangerous in terms of the possibility of venous thrombosis.
Diagnosis of menopausal syndrome
To correctly assess the patient’s condition, consultations with an obstetrician-gynecologist, gynecologist-endocrinologist, gynecologist-mammologist, neurologist, ardiologist, etc. are needed.
If the physiological menopause passes smoothly, gradually, and does not cause noticeable disturbances, it does not need treatment and may only require psychotherapeutic correction.
Diagnosis of the pathological course of menopause is based on changes that appear at the age of approaching or approaching menopause. Concomitant diseases are aggravated, they complicate the diagnosis of menopausal syndrome during menopause, and aggravate its course and cause the development of atypical forms.
To diagnose the complicated course of menopause, the blood levels of follicle-stimulating and luteinizing hormones and estrogens are examined. To clarify the functional state of the ovaries, a histological analysis of scrapings of the endometrium of the uterus and cytological studies of vaginal smears over time are performed, and a graph of basal temperature is plotted.
Research needs to be done:
- Ultrasound of the pelvic organs;
- Ultrasound of the mammary glands and mammography;
- cytological analysis of smears from the cervix and cervical canal;
- biochemical study of blood test parameters and coagulation factors (coagulogram).
- Ultrasound of the liver
Hot flashes during menopause: treatment without hormones
Expert opinion
Many women cannot take hormonal medications due to certain health conditions. For example, if there is a risk of breast cancer, a tendency to form venous blood clots, cerebrovascular accident (stroke) and heart attack, hormone replacement therapy is not recommended, since the potential risks from it may be higher than the benefits.
Obstetrician-gynecologist of the highest category Oksana Anatolyevna Gartleb
To mitigate the intensity of menopause symptoms, not only hormone replacement therapy, but also other drugs are used. Instead of hormones, you can use the following:
Drugs that normalize blood pressure
During menopause, changes in the water-salt balance occur, resulting in fluid retention in the body and an increase in blood volume. This leads to increased blood pressure during hot flashes. Taking medications that lower blood pressure helps reduce sweating and the feeling of heat during such conditions.
Sedatives and antidepressants
These medications, given in small doses, help reduce the stress caused by hot flashes. In addition, taking antidepressants and sedatives in some cases reduces the frequency and intensity of hot flashes by normalizing the condition of blood vessels.
Expert opinion
Remember that antidepressants can be quite harsh on your health and may cause some side effects. Therefore, their prescription and selection of the appropriate dosage should be handled exclusively by a specialized specialist.
Obstetrician-gynecologist of the highest category Oksana Anatolyevna Gartleb
Vitamin and mineral complexes, dietary supplements
During menopause, it is recommended to take complexes rich in retinol, tocopherol, ascorbic acid, B vitamins, vitamin D, calcium, magnesium, boron.
Dietary supplements based on phytoestrogens. Phytohormones include coconut oil, chamomile, calendula, ginseng root, grapes, dates, pomegranates, red clover, alfalfa, flax, licorice, etc.
Causes of menopause
This condition is considered physiological and occurs due to natural age-related changes.
The fact is that, unlike male sperm, the number of eggs that mature in a woman’s ovaries is limited and is determined at birth. With each menstrual cycle there are fewer and fewer of them. When there are no eggs left, pregnancy becomes impossible, and the body “turns off” the functions responsible for conceiving and carrying a child. In addition, the ovaries stop producing estrogen, which is responsible for egg implantation and prepares the uterine vessels for feeding the fetus. Due to hormonal changes that occur during menopause, the thickness of the endometrium (the inner mucous layer of the uterus) becomes smaller, as a result of which a woman loses the ability to bear a pregnancy.
This physiological process may speed up. Risk factors for early menopause include an unhealthy lifestyle, intense physical activity, chronic stress, chronic endocrine diseases (diabetes mellitus, hypothyroidism), unfavorable environment, hereditary predisposition, rare sex life, excess weight, poor nutrition and diets.
Menopause in men (andropause) is characterized by a decrease in the production of the male sex hormone - testosterone. The age of its onset also occurs at 45-50 years, and the duration ranges from 2 to 5 years. Childbearing function, like that of women, fades away.
Hot flashes during menopause: treatment with folk remedies
Not only traditional medicines, but also traditional medicine methods help to cope with fever and sweating during menopause. They should not be considered as the main means of therapy, but they can act as effective additional means.
Various herbs are used to combat the unpleasant symptoms of menopause. You can prepare decoctions and infusions from them, for example:
- Hawthorn fruits and flowers. Rinse 5 g of prepared raw materials, place in a thermos and pour a glass of boiling water. Leave for an hour. Take half a glass 2 times a day before meals. The infusion not only reduces the frequency and intensity of hot flashes, but also improves heart function and vascular condition.
- Red clover. Red clover belongs to the category of phytoestrogens, so this plant is actively used to reduce hot flashes. To prepare the infusion you need to take 2 tbsp. dry crushed red clover herb, place in a thermos and pour a glass of boiling water, leave to infuse for 10 hours. Take the resulting infusion before meals, 50 ml.
- Sage. It is useful to take a decoction. To prepare it, you need to take 1 tbsp. dry sage, pour 1.5 tbsp. boiling water and simmer for 5 minutes over low heat. Then cool the broth, strain and drink as tea throughout the day.
- Red brush root (rhodiola tetrapartite). Before taking products based on red brush, you should consult your doctor, as this plant is contraindicated for women suffering from hypertension. Pour the dried crushed root (1 tbsp) into a glass of water and boil for a quarter of an hour. Cool the broth, strain and take 100 ml before meals three times a day.
- Borovaya uterus.
This plant helps to compensate for the lack of estrogen, as it belongs to the category of phytohormones.To prepare a decoction of boron uterus, you need to take a tablespoon of the dry plant, pour a glass of boiling water over it and simmer over low heat for 5 minutes. Then strain, cool the broth and drink 100 ml before meals three times a day.
- Dry rosemary. To prepare the decoction, take 1 tbsp. raw materials, pour a glass of boiling water and boil for a quarter of an hour. Then strain, cool and take the resulting product before meals three times a day.
Menopause in a woman without hot flashes
Treatment of menopausal syndrome
The goal of treating the pathology of menopause is to reduce its manifestations and symptoms.
Antidepressants reduce the frequency of hot flashes during the pathological course of menopause.
To prevent osteoporosis during menopause, non-hormonal bisphosphonates are used; they reduce bone loss and the risk of fractures.
To reduce the manifestation of urogenital manifestations, local (vaginal) administration of estrogen in the form of cream or tablets is used.
The most effective method of treating menopausal syndrome during menopause is hormonal therapy individually prescribed by a doctor.
Hormone therapy as a treatment for menopause pathology is contraindicated in patients suffering from:
- endometrial, ovarian, breast cancer;
- coagulopathy (blood clotting disorder);
- liver dysfunction;
- thromboembolism, thrombophlebitis;
- uterine bleeding of unknown cause;
- renal failure.
In case of psycho-emotional manifestations, consultations with specialists in psychology are required every six months in order to monitor the condition and, if necessary, correct the emotional background.
Menopause without hot flashes: reality or dream?
Unfortunately, most women experience the unpleasant symptoms of menopause firsthand. However, each of them has a choice: to come to terms with the manifestations of this condition or to alleviate it by taking the right medications.
One of the best remedies for hot flashes during menopause is Klimafemin.
This drug was developed by specialists from the pharmaceutical company VERTEX and has the necessary documents and certificates. The product is distinguished by a balanced composition, which includes natural components: phytoestrogen genistein, coenzyme Q10, grape seed extract and vitamin E. As a result of the use of “Climafemin”, the frequency and intensity of hot flashes decreases, sweating decreases, and the emotional background improves. Sources:
- Menopausal syndrome. Smetnik V.P., Tkachenko N.M., Glezer G.A. and others // M. - 1988. - P. 286.
- Depressive disorders in peri- and postmenopausal women. Yureneva S.V., Kamenetskaya T.Ya. // Journal of gynecology. - 2007. - 9(2). pp. 5-12.
- Mental disorders in women during menopause. Tyuvina N.A. // M.: Kronpress. - 1996. - P. 237.
- https://cyberleninka.ru/article/n/myagkiy-klimaks
- https://cyberleninka.ru/article/n/ispolzovanie-bad-dlya-korrektsii-klinicheskih-proyavleniy-perimeno…
- https://cyberleninka.ru/article/n/sovremennye-podhody-k-diagnostike-prognozirovaniyu-techeniya-i-lec…
Duration of tides
The duration of a fever attack is difficult to determine; it is individual for each woman. For some people, hot flashes may last a very short time and soon stop completely, while for others they may continue to occur for the rest of their lives. In any case, the longer they occur, the weaker they become.
The decrease in estradiol levels is recorded mainly one to two years before menopause (the last menstrual period in life, usually around age 50) and continues into early postmenopause. In postmenopause, the period after the last menstruation, they occur in 70-80% of women of this age, and in more than half they last for more than 2-3 years.
Numerous habits or substances can contribute to hot flashes, so it is recommended:
- limit hot drinks, spicy foods, alcohol and caffeine;
- do not wear tight or synthetic clothing;
- no smoking;
- avoid stressful situations;
- Do not stay in excessively warm rooms.
Popular questions
Hello!
Constant hot flashes tormented me. I started drinking Gynocomfort Klimafemin. It helped right away. But it turned out that it was not available in any pharmacy! It was difficult to buy only one package. Has this product been discontinued? Hello! Gynocomfort climafemin continues to be produced. You can purchase it in pharmacies that sell other VERTEX products.
Hello, I have up to 10 hot flashes per day, more at night. A year ago I took the drug Femoston 2 for three months, it helped, everything was fine for six months, but it all started again. Is it possible to correct this condition without hormonal drugs?
Hello! The Ginocomfort line of drugs includes the drug Climafemin. It contains antioxidants and phytoestrogens, which will correct the vegetative manifestations of menopause. If there is no effect after 1 month of use, you should consult your doctor again.
Hot flashes, insomnia, what to do? I take Klimanalin, it doesn’t help.
Hello! Vivid vegetative manifestations in the menopause are caused not only by hormonal changes, but also by a possible combination of thyroid pathology - hypothyroidism, vertebrobasilar insufficiency. Therefore, it is advisable: consultation with an endocrinologist or neurologist. OMT ultrasound, flora smear, cytology, which will allow prescribing menopausal hormone therapy in the absence of contraindications. At this stage, pending examination results, you can add Gynocomfort climafemin to treatment. The drug contains phytoestrogens and antioxidants, which has a beneficial effect on well-being and eliminates the symptoms of menopause. The drug is taken 1 t once a day for 3 months.
I am 49 years old and suffered from frequent hot flashes. How to prevent them?
Hello!
These are manifestations of menopausal syndrome associated with the extinction of ovarian function. At this stage, I recommend using a herbal-based drug that allows you to stop bursts of vegetative reactions - Ginocomfort Klimafemin 1 t once a day for 3 months. During this time, conduct an examination: ultrasound OMT, they say. glands, flora smear, oncocytology, oak, lipid spectrum, FSH, TSH levels. Consult a therapist and other related specialists if you have chronic diseases that would be a contraindication for prescribing menopausal hormone therapy. This will help the obstetrician-gynecologist correctly select further treatment. For an accurate diagnosis, contact a specialist
Interpretation of results
Although "double the risk" sounds scary, the overall increase in heart risk in women associated with hot flashes remained relatively low.
So what should women take away from this discovery? Dr. Rexrode recommends taking heart health seriously and using menopause as a time to reassess your risks. She recommends the following important steps:
Identify your risk factors.
Dr. Rexrode noted that it is always important to review risk factors for cardiovascular disease in midlife. The likelihood of a heart attack or stroke increases in women during and after menopause. Although researchers have found a link between hot flashes and heart risks, it is too early to do anything with this information. Instead, women should continue to focus on established risk factors for cardiovascular disease, such as high cholesterol, high blood pressure and diabetes.
Let's look at some risk factors for women only.
Dr. Rexrode. identified the following two factors:
- early menopause (before 40 years)
- an episode of preeclampsia (a potentially life-threatening complication of pregnancy accompanied by high blood pressure and protein in the urine).
If you're not at high risk for heart disease, but you have one or both of these factors, it may increase your risk level, she says. “Additional risk factors include other pregnancy complications, gestational diabetes and hot flashes.” If additional evidence becomes available, it may be added to this list.
Hot flashes are common during menopause, but frequent or persistent episodes may be a sign of a higher risk of heart attack or stroke.
Scientists are paying more attention to women-specific risk factors for heart disease, and in the coming years, more will be known about how these factors can affect your health.
The main problems for women during menopause
One of the most striking problems of this period is the violation of intimate life. A woman’s desire naturally decreases, discomfort appears during sex, and the amount of natural lubrication decreases. But this is not a reason to give up intimate life altogether!
It is important to discuss the problem with your doctor and select special products - lubricants (for example, with a warming effect) that will relieve discomfort. It is also necessary to replenish the balance of hormones, which we will discuss later in the article.
In some cases, uterine bleeding that is not menstrual is possible. In this case, it is necessary to consult a gynecologist as soon as possible to avoid the development of pathologies.
Also, during menopause in women, calcium is actively washed out of the bones, which causes the development of osteoporosis - fragility of bone tissue. Modern diagnostics make it possible to detect the development of osteoporosis in a timely manner. And prevention will be stable moderate physical activity, a nutritious and varied diet.
How to relieve menopause symptoms
A healthy lifestyle, balanced nutrition, taking vitamins and physical activity will help smooth out the symptoms of menopause and improve your emotional background. Regular sex life will help maintain prostate health. But if the symptoms of menopause worsen a man's quality of life, he may be advised to take testosterone.
If you want to preserve your men's health for as long as possible, contact Dr. AkNer, here you will be given a high-quality examination and all existing problems will be identified.
Urologist, andrologist Akopyan Nerses Grigorievich.
Back to list of articles