Symptoms
There are many types of vasculitis known. They all have their own characteristics and symptoms. The most common types of this disease:
1. Periarteritis nodosa (small and medium arteries). The disease threatens stroke and mental disorders. More often diagnosed in men. Characterized by:
- muscle pain;
- elevated temperature;
- losing weight;
- abdominal pain;
- vomiting and nausea.
2. Wegener's granulomatosis (vessels of the respiratory system and then the kidneys).
Symptoms:
- sinus pain;
- nasal discharge with pus and blood;
- ulcers on the nasal mucosa;
- destruction of the nasal septum, change in the shape of the nose;
- cough (sometimes with blood);
- chest pain;
- renal failure.
3. Giant cell temporal arteritis (large vessels, most often the head). It mainly affects people of retirement age. Symptoms:
- undulating fever;
- weakness;
- weight loss;
- severe pain in the head of a pulsating nature, aggravated by chewing;
- swelling in the temple area.
4. Tokayasu disease (large arteries and aorta). Signs:
- numbness, pain in the arms and legs;
- pain in the back, stomach, etc.;
- fainting;
- blurred vision.
Vasculitis in children
Vasculitis in children is a rather rare phenomenon, but all varieties have characteristic features that are characteristic only of childhood.
Kawasaki syndrome
A systemic form of the disease in children under 7 years of age with damage to the heart vessels, lymph nodes, and respiratory tract mucosa. The clinical picture is characterized by a rapid, acute onset with a temperature of 38 to 41 degrees and the following symptoms (in order of gradual appearance):
- debilitating fever;
- skin lesions with a scarlet-like rash with erythematous plaques;
- damage to the mucous membranes of the respiratory tract, nose, eyes;
- thickening and redness of the skin on the soles and palms of the hands;
- enlarged lymph nodes in the neck;
- crimson tongue color;
- peeling of the skin around the nails, on the phalanges of the fingers;
- damage to the cardiovascular system in the acute phase, aneurysm.
Kawasaki syndrome can be cured with timely diagnosis, the consequences are eliminated after 5-8 years.
Hemorrhagic vasculitis
While hemorrhagic vasculitis in adults can be caused by pathologies during pregnancy, diabetic nephropathy, liver cirrhosis, malignant neoplasms, the cause of this form of the disease in children is most often upper respiratory tract infections, measles, paratyphoid fever, drug or food allergies.
Hemorrhagic vasculitis in children is divided into the following forms: cutaneous, cutaneous-articular, abdominal, renal and cutaneous-renal. Each of them has specific symptoms:
- skin form - severe swelling against the background of cold urticaria, purpura, rash localized on the feet, legs gradually spreading to the hips, pain in the joints;
- abdominal form: severe with severe abdominal pain localized near the navel;
- renal form - the presence of proteins and globulins in the urine.
Hemorrhagic vasculitis is dangerous due to complications, relapses and a tendency to generalization - spreading to the vessels of internal organs.
Prevention
Unfortunately, it is impossible to protect yourself one hundred percent from the appearance of vasculitis. Preventive measures include maintaining immunity, a healthy lifestyle, and paying attention to health.
If a person has already been diagnosed with vasculitis, we must not forget that the disease can return, so you need to carefully monitor your well-being.
Medical specialists in St. Petersburg remind: the sooner treatment is started, the less negative impact the disease will have on the body. If symptoms appear, consult a doctor immediately. Registration by phone is carried out around the clock.
Symptoms and manifestations
The initial stage of vasculitis has no obvious symptoms and it happens that the disease is not immediately recognized. Although symptoms vary, there are a few common symptoms:
- inflammatory changes in the skin;
- swelling, rash, hemorrhage, necrosis;
- The lesion appears symmetrically on both legs;
- The rashes look like red spots, nodules, erosions, ulcers;
- The initial manifestation is predominantly in the legs.
Vasculitis is characterized by the presence of purpura. This is a reddened area of skin raised above the surface of the skin that can be felt with your fingers.
In addition, the person experiences pain in the joints and muscles, general weakness, itching and burning of the affected areas of the skin, and has a fever of more than 38 degrees.
For vessels of different sizes, the symptoms of the disease are slightly different:
These symptoms only allow us to determine the general clinical picture. To make a definite diagnosis, it is necessary to identify symptoms characteristic of this subtype of vasculitis.
Treatment
To get rid of vascular inflammation, they require medications. In each case, therapy is selected individually after establishing the exact form of the disease.
Traditional methods
Classic treatment involves taking medications such as:
- Non-hormonal anti-inflammatory drugs (Naproxen, Indomethacin), which relieve inflammation and pain, but are contraindicated for stomach ulcers, kidney and liver diseases, and during pregnancy;
- glucocorticoid drugs, such as prednisolone, to suppress an immune system that has become aggressive towards its own body;
- Cytostatics (“Cyclophosphamide”), slowing down cell division;
- antihistamines (Suprastin) for the nodular erythematous form of the disease;
- Foods containing vitamin C and calcium to help keep blood vessels tight and prevent breakage.
In addition to tablets, external preparations are prescribed - topical ointments (Iruksol, Solcoseryl). Affected areas may be blurry and solid green. To reduce lumps, use dry heat; to reduce joint pain, use applications with Dimexide.
Physiotherapeutic procedures will be useful - ultraviolet blood irradiation, plasmapheresis, oxygen therapy.
Traditional therapy
Also, folk remedies have a positive effect in the treatment of vasculitis. To avoid negative consequences, consult your doctor before using them.
For use in therapy:
- Decoctions of tricolor violet, collection of nettle leaves, ergot, elderberry, yarrow, Japanese poplar berries;
- homemade ointments from a mixture of birch buds and intestinal fat, pine resin, which can be applied to sore spots;
- Elderberry infusion, lemon-alcohol tincture.
Treatment with plant decoctions containing vitamins is useful. Leaves of black currant, St. John's wort and centipedes are used.
To improve blood circulation in the legs, exercises such as “bicycle”, “scissors”, “birch”, and lifting weights on the tips of the fingers are recommended.
Which doctor treats, how is the disease diagnosed?
Having discovered the first symptoms indicating this disease, a person is interested in what the doctor is treating for it.
If you have a rash on the skin of your legs and other symptoms of vasculitis, consult your doctor. To make the correct diagnosis, he will refer specialists for consultations - a dermatologist, rheumatologist, neurologist, allergist, hematologist and others.
The attending physician prescribes additional tests:
- Clinical and biochemical analysis of blood, urine;
- ECG, X-ray, ultrasound;
- biopsy;
- immunological analysis.
Most often, when the disease is first detected, the final diagnosis is made by a rheumatologist, who, if necessary, refers the patient to a specialist. Based on the results of the study, the specialist prescribes treatment aimed at eliminating the causes of vasculitis.
After completion of treatment, the patient must be under medical supervision for two years to avoid relapse.
Causes of the disease
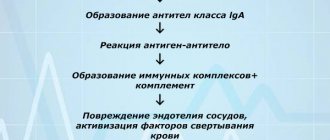
To date, the reasons that provoke the development of this pathology have not been fully studied. The main provoking factor is a failure of the body's immune system. This may be an infectious disease, especially a viral one.
As inflammation progresses, it increasingly affects the blood vessels, impairing the blood supply to the organ, leading to hemorrhage, necrosis, as cells die in the absence of adequate nutrition.
The following factors can provoke changes in the blood vessels of the lower extremities:
- frequent colds without proper treatment;
- hereditary predisposition;
- thyroiditis;
- diseases that have become chronic;
- untreated or advanced arthritis;
- tendency to allergies.
Constant stress, hypothermia, injuries, and uncontrolled use of certain medications have a negative impact.
Sometimes bruises appear on the skin along with the rash.
Experts believe that they are caused by autoimmune disorders, and in other cases, vasculitis provokes hereditary diseases and ailments caused by failure of internal organs.
Bruises occur due to increased fragility of capillaries, which are easily damaged by light pressure on the skin. If they are symmetrical (in the ankle, knee area), then hemorrhagic vasculitis is diagnosed.
2. Why is vasculitis dangerous?
The danger of vasculitis lies in the possibility of developing serious complications. In particularly severe cases, when part of a blood vessel stretches and dilates, the likelihood of an aneurysm
– bulging section of the walls. The danger of this pathological process lies in the rupture of the aneurysm, which can cause many irreversible consequences: from circulatory disorders to death.
In the case of the opposite behavior of blood vessels during vasculitis, when inflammation contributes to their narrowing, there is a possibility of cessation of blood supply to individual organs and tissues. If alternative blood vessels cannot provide the required amount of blood to them, necrosis of the affected tissues or organs may occur.
Visit our Rheumatology page
Complications
Since the vascular network interweaves all organ systems, performing trophic (nutritional) and respiratory functions for them, vascular necrosis has an extremely negative effect on the organs themselves: due to malnutrition, their ischemia develops, which leads to a decrease in the function of one or another structure.
The following main consequences of vasculitis are usually identified:
- Kidney damage and the formation of chronic renal failure, up to the development of anuria;
- Ischemic heart damage, development or worsening of coronary heart disease, development of aneurysms and valve defects;
- Lesions of the gastrointestinal tract: necrosis and intussusception, the formation of intestinal obstruction;
- Risk of developing hemorrhagic stroke.
3. Symptoms of the disease
The unpredictable nature of the occurrence of vasculitis makes its symptomatic picture very vague and diverse. And yet it is possible to identify the relationship between the signs of vasculitis and its location. For example, if skin damage occurs with vasculitis, then its symptom will be a specific rash. If there is a disruption in the blood supply to any part of the nerve, then a sign of this pathological process will be muscle weakness and loss of sensitivity. A stroke indicates a violation of the blood supply to the brain, and a heart attack indicates a violation of the blood supply to the heart.
Among the general symptoms of vasculitis, characteristic of all types of this disease, are the following:
- lack of appetite;
- weakness;
- increased body temperature;
- increased fatigue;
- pallor.
Therefore, it is very important to immediately consult a doctor if you notice any unclear symptoms of vasculitis.
About our clinic Chistye Prudy metro station Medintercom page!
Treatment of vasculitis
Treatment is aimed at eliminating symptoms and controlling the disease. Therapy takes quite a long time.
With secondary vasculitis, treatment is aimed at eliminating the underlying disease. In such cases, after recovery, the signs of the disease disappear on their own and no medical intervention is required.
Treatment of primary vasculitis is more problematic. It can be carried out both at home and in a hospital, but always under the supervision of a doctor. Treatment includes corticosteroids and immunosuppressants. The doctor may also prescribe other medications depending on the affected organs and the person’s general condition. To reduce the side effects of drugs, the patient is recommended to take vitamin D and calcium. Therapeutic gymnastics, physiotherapy and psychological support of others bring benefits.
Vasculitis
Vasculitis (angiitis, arteritis, rheumatism of blood vessels) is a general term for various forms of vascular inflammation. A disease with a potentially dangerous course that can affect almost any organ system. Vasculitis is considered a rheumatic disease because it often causes joint or muscle pain and sometimes joint swelling. There are primary vasculitis and secondary vasculitis.
Causes - how does vasculitis occur?
The immune system is designed to protect the body from viruses and bacteria. Immune cells determine whether the foreign agent is an endogenous cell, bacteria or virus. What all rheumatic diseases have in common is that, due to misidentification, the body's own structures are mistaken for bacteria and are attacked by the immune system.
Such abnormal reactions can cause an attack on the walls of blood vessels. Since every human organ is supplied with blood vessels, it can be damaged as a result of such inflammation.
Symptoms of vasculitis
In most cases, vasculitis does not occur suddenly, but appears slowly. Since the organs do not receive enough “nutrients,” the disease first makes itself known as a common infection. Signs of vasculitis may include:
- muscle and joint pain, rarely swelling of the joints
- redness of the eyes
- visual disturbances
- headache
- bloody runny nose or sudden hearing loss
- numbness (eg in the feet)
- discomfort in the gastrointestinal tract
- skin changes (red spots, nodules, ulcers)
- hemoptysis
- bloody urine
The first general symptoms may be:
- fatigue
- weight loss
- heat
- night sweats
Many symptoms may have other causes. However, as a rule, a specialist can suspect vasculitis if several signs appear in different organs.
Types of vasculitis
Vasculitis is classified based on the size of the blood vessels involved:
small vessel vasculitis
- when microscopic blood vessels become inflamed - capillaries, arterioles and venules, which are not visible to the naked eye.
large vessel vasculitis
- inflammation of large blood vessels, such as the main artery (aorta), carotid artery, or temporal artery, is called
There are a number of different clinical pictures that are precisely defined by rheumatologists. A typical small vessel vasculitis is granulomatosis with polyangiitis (Wegener's granulomatosis). A typical large vessel vasculitis is giant cell arteritis (temporal arteritis).
Forms of vasculitis
Doctors distinguish between primary and secondary vasculitis. Secondary vasculitis
follows another underlying disease (for example, rheumatism or viral infections) or the use of certain medications.
Primary vasculitis
manifests itself as an independent disease. The causes of vasculitis are largely unknown, which is why some doctors refer to it as idiopathic vasculitis.
Depending on which blood vessels (small or large) are affected, different clinical pictures develop.
Diagnostics
If necessary, consultations with a vascular surgeon, therapist, ophthalmologist, neurologist, otolaryngologist, etc. are scheduled.
Lab tests
- general blood test (usually an increase in ESR is noticed);
- biochemical blood test (protein fractions, etc.);
- immunological tests (gamma globulin, C-reactive protein, rheumatoid factor, ANCA, etc.)
- Autoantibody testing indicates the presence of an autoimmune disease and its type
Hardware diagnostics
- angiography - examination of blood vessels using X-ray contrast agents);
- biopsy - the doctor takes a tissue sample from affected parts of the body (eg, lung, temporal artery, kidneys) to confirm the diagnosis of a specific vasculitis. Samples from the skin, mucous membrane or kidneys are taken under local anesthesia and sent for histological examination.
- Computed tomography and magnetic resonance imaging with the introduction of a contrast agent can exclude other causes of the described symptoms, such as cancer, bleeding or vascular changes.
- Color duplex sonography makes it possible to visualize blood flow, narrowing or bulging of blood vessels.
Treatment
The prognosis in the treatment of vasculitis depends primarily on the type of vascular inflammation. Early and targeted therapy has a positive effect on the course of the disease. Vasculitis is usually not completely cured, but symptoms can be relieved with proper therapy.
When treating vasculitis, drugs that affect the immune system are used.
When treating secondary vascular inflammation, the underlying disease is treated first. Certain triggers are eliminated and should be avoided afterwards (such as certain medications or dietary supplements).
Antihistamines and nonsteroidal anti-inflammatory drugs (NSAIDs) help against common symptoms of vasculitis, such as pain or excessive inflammatory reactions.
In addition to drug treatment, experts also recommend that patients with vasculitis engage in regular exercise (such as swimming), a healthy diet (high-quality vegetable oils, small amounts of meat, protein-rich foods adapted for kidney function), and avoidance of nicotine.