Published: 07/23/2021 14:15:00 Updated: 07/23/2021
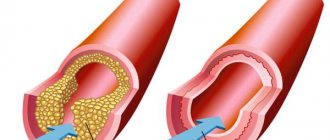
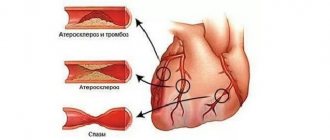
Atherosclerosis is a systemic disease that primarily affects the arteries. Cholesterol is deposited in the walls of blood vessels, resulting in the formation of plaques that interfere with normal blood flow. Internal organs experience a lack of oxygen and nutrients, and with the slow progression of the pathology, their work is gradually disrupted. In the case of acute thrombosis with complete blockage of blood flow, severe complications may develop - myocardial infarction, stroke, gangrene of the lower extremities and other dangerous pathologies.
Reasons for appearance
The appearance of atherosclerosis is associated with metabolic disorders in the body, lipid imbalance and excess cholesterol in the blood.
Mechanical damage to the vessel wall also plays an important role, contributing to atherosclerotic deposits and plaque formation at the site of injury. The risk of developing atherosclerosis is higher in men over 45 years of age, women over 55 years of age or with early menopause, as well as among people with familial hypercholesterolemia and family history, whose relatives already suffer from this disease.
Other factors contribute to it:
- unbalanced diet with an abundance of fatty foods;
- excess body weight;
- smoking;
- alcohol abuse;
- sedentary lifestyle;
- cardiovascular diseases – ischemic heart disease, arterial hypertension;
- endocrine pathologies, in particular diabetes.
Main risk factors
- smoking (the most dangerous factor),
- hyperlipoproteinemia (total cholesterol > 5 mmol/l, LDL > 3 mmol/l, Lp(a) > 50 mg/dl), - an increase in the amount of cholesterol and its fractions in the blood,
- arterial hypertension (high blood pressure) (systolic blood pressure > 140 mm Hg; diastolic blood pressure > 90 mm Hg),
- diabetes mellitus, obesity,
- sedentary lifestyle,
- emotional stress,
- drinking large amounts of alcohol,
- poor nutrition, hereditary predisposition, postmenopause, hyperfibrinogenemia (increased levels of fibrin (a protein involved in coagulation) in the blood),
- Homocysteinemia is a hereditary disease leading to an increase in homocysteine protein in the blood.
Classification of the disease
The formation of atherosclerotic plaques can occur in individual vessels or affect most of them. Depending on the organ in which blood flow is reduced and the affected artery, the following forms of the disease are distinguished:
- Heart shape. Ischemic atherosclerosis with damage to coronary vessels and valves.
- Kidney form. The renal arteries are affected.
- Brain (cerebral) form. The disease spreads to intracranial vessels.
- Intestinal form. The mesenteric arteries are affected.
- Atherosclerosis of the aorta. Its abdominal region is most often affected.
- Atherosclerosis of the arteries of the lower extremities, mainly femoral.
- Atherosclerosis of brachiocephalic vessels. These include the right carotid, vertebral and subclavian arteries.
What is atherosclerosis and why does it occur?
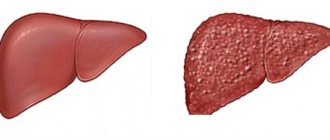
Atherosclerosis is a vascular disease that occurs in most people with age. As a rule, older people suffer from it. The disease is manifested by the deposition of various cholesterol plaques on the walls of the arteries.
The causes of plaque formation are smoking, alcohol abuse and fatty foods. The development of atherosclerosis is also influenced by physical inactivity: when people, due to their profession, are forced to sit at the computer for a long time, for example. Those who walk little, constantly use the elevator to climb even several floors, and generally lead a sedentary lifestyle are at risk.
Symptoms of atherosclerosis
For years and even decades, the disease can occur without clinical manifestations.
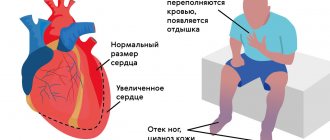
Subsequently, signs of poor blood supply to various organs are observed. With atherosclerosis of the heart, the patient is bothered by “squeezing” pain behind the sternum during physical activity - angina pectoris, arrhythmia, a feeling of palpitations accompanied by shortness of breath, and the development of myocardial infarction is possible.
In case of damage to the abdominal vessels, there may be attacks of pain in the upper and middle parts of the abdomen, which are accompanied by increased gas formation and constipation.
Atherosclerosis of the cerebral arteries manifests itself in dizziness and short-term episodes of loss of consciousness, and tinnitus. As the disease progresses, a stroke may develop with its neurological symptoms - dizziness, headache, lack of coordination and disorientation, numbness or weakness of the muscles of the face, arms or legs of one side of the body, sudden speech disturbances, visual disturbances, prolonged unconsciousness.
Vascular thrombosis of the lower extremities can lead to numbness and discoloration of the skin of the legs, a crawling sensation, and muscle pain when walking - “intermittent claudication.” Subsequently, the skin becomes thin and dry, peels, nails thicken, difficult-to-heal trophic ulcers form, and frequent cramps appear.
The main symptom of renal artery disease is an uncontrolled increase in blood pressure, leading to drug-resistant hypertension.
How the heart is supplied with blood
The heart muscle works constantly and needs good blood supply.
To satisfy its needs, two coronary arteries approach it, originating from the aorta. The right vessel is responsible for the blood flow of the posterobasal region, septum and right ventricle. The rest of the myocardium receives oxygen and nutrition from the left artery, which branches into the anterior interventricular branch (LAD) and the circumflex. Venous blood is collected through the coronary veins into the sinus, which is located in the right ventricle. If there are plaques in the lumen of the arteries, then the heart experiences an increased need for oxygen, which increases during physical activity. Without receiving what it needs, the muscle begins to die. Angina pectoris, cardiosclerosis and necrosis develop.
Diagnosis of atherosclerosis
The diagnosis is based primarily on the results of laboratory tests and data from instrumental research methods.
A conversation with a patient only allows us to identify risk factors for the development of diseases and, together with an examination, as well as consultation with other specialists, suggest which organs have already been affected by the disease. Diagnosis of atherosclerosis necessarily includes:
- Blood chemistry.
- Ultrasound of the heart and blood vessels.
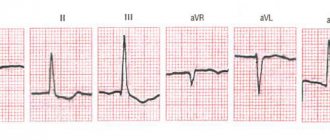
- Electrocardiography.
A high predisposition to the development of the disease is indicated by changes such as an increase in the concentration of total cholesterol, triglycerides, low- and very low-density lipoproteins, and a decrease in the amount of high-density lipoproteins.
Innovative risk factors for atherosclerosis include C-reactive protein (CRP), apolipoproteins A1 (apoA1) and B-100 (apoB), some polymorphisms of endothelial synthase genes (NOS3G894T, NOS3T(-786)C) and blood coagulation factors FV and FII. To obtain accurate results of a blood test for atherosclerosis, three days before the test you should give up fatty, cholesterol-rich foods, and 8-10 hours before, eat nothing at all and drink a lot of liquid. 30 minutes before the test, you should avoid strong emotional stress, stress, and do not smoke.
Echocardiography clearly shows signs of atherosclerosis of the heart valves and aorta. According to indications, ultrasound scanning of the brachiocephalic, transcranial, and arterial vessels of the lower extremities is also performed.
Reflects disturbances in heart rhythm and electrical conductivity of the organ. Exercise testing may be performed to detect exertional angina.
The standard list of laboratory tests also includes a general clinical blood test and a general urinalysis.
Additionally, for the purpose of differential diagnosis, blood tests for the level of fibrinogen, homocysteine, antibodies to cardiolipin (IgG and IgM), and lupus anticoagulant may be recommended. To visualize atherosclerotic plaques, according to indications, angiography is used - an X-ray examination with the introduction of a contrast agent. In case of preparation for surgery on the heart vessels, coronary angiography is performed.
The “gold standard” for diagnosing pathological changes in the arteries of the brain and parenchymal organs is spiral computed tomography with contrast.
Often such patients are recommended to consult an ophthalmologist. Fundus ophthalmoscopy reveals signs of atherosclerotic damage to small retinal vessels.
Forms
The classification of the form of the disease is determined by the severity of pathological changes:
- Non-stenotic. The lumen of the coronary arteries is closed by less than 50%. Hemodynamics are difficult.
- Stenosing. Narrowing of the vascular lumen by more than half. The blood supply to the heart is significantly impaired.
- Occlusion. Complete blockage of the vessel.
A hardened growth on the intima can damage the vessel. This will trigger the formation of a blood clot that blocks the artery
Treatment
Treatment of atherosclerosis begins with correction of diet and lifestyle changes.
All patients are recommended to lose weight, moderate physical activity, and quit smoking and alcohol. Often the cause of atherosclerosis is a nutritional factor, so diet plays a very important role. To reduce the concentration of cholesterol in the blood, it is important to avoid meat broths, fatty, salty, smoked foods, semi-finished products, spicy, spicy, fried foods, and limit the consumption of table salt.
Prohibited products include:
- sugar;
- confectionery, sweets;
- mayonnaise, tomato and other store-bought sauces;
- bakery products made from wheat flour;
- offal;
- sweet carbonated drinks;
- industrially produced juices and nectars;
- cocoa;
- canned meat and fish;
- dried fruits high in sugars;
- strong coffee and tea.
It is recommended to eat split meals five times a day, including a sufficient amount of fiber, protein (lean meats and fish, low-fat cottage cheese), fresh vegetables (except potatoes), fruits, and dairy products.
Drug therapy is aimed at:
- decreased cholesterol synthesis (statins, fibrates);
- decreased absorption of fats from food (cholesterol absorption inhibitors, bile acid sequestrants);
- prevention of thromboembolic complications (antiplatelet agents);
- relief of symptoms of atherosclerosis (painkillers, antispasmodics).
To determine indications for surgical treatment, the degree of disruption of blood flow in the vessel is determined.
An overlap of its lumen of less than 50% is considered hemodynamically insignificant; with stenosis of 50-70%, only drug therapy is usually carried out. Correction of arterial obstruction surgically must be performed in the third stage of atherosclerosis and narrowing of the lumen by more than 70%. There are two main types of surgical intervention:
- Balloon angioplasty. A balloon is inflated inside the affected vessel, while the atherosclerotic plaque is flattened and evenly distributed along the artery wall. At the end of the manipulation, the device is removed.
- Arterial stenting. During the operation, a thin lattice cylinder is inserted and opened in the area of narrowing. It also presses against the plaque, but remains in the lumen of the vessel, gradually growing into its endothelium.
Publications in the media
Atherosclerosis of the coronary arteries with their hemodynamically significant stenosis leads to the emergence of various clinical variants of coronary heart disease (see Coronary heart disease) • In addition to atherosclerosis (more than 90% of cases of coronary artery disease), coronary artery disease can be caused by arteritis, collagenosis, thrombosis and embolism, anomalies in the development of coronary vessels and etc.
Frequency - see Coronary heart disease.
The etiology in most cases is unknown • The main role, apparently, belongs to various disorders of lipid metabolism (see Hyperlipidemia), detected in almost all patients with coronary artery disease • In some cases, atheromatosis is accompanied by diffuse distal sclerosis of the coronary arteries without local lipid infiltration of their wall (X- syndrome).
Pathophysiology • The heart requires 0.1–0.2 ml of oxygen per 1 g of weight per minute. Such intense gas exchange is possible due to the high perfusion pressure in the coronary arteries arising directly from the aortic ostium, the high inflow volume of 5% of the bcc, and the increased extraction of oxygen by the myocardium (more than 75% at rest and almost 100% at maximum load) • With stenosis of the coronary arteries of less than 70–75% of their lumen, disturbances in myocardial perfusion occur only during exercise, and at rest the decrease in perfusion does not exceed 5% of normal values • Even with complete occlusion of one of the main coronary arteries, the level of perfusion of the “compromised” myocardial zone is reduced by only 50 % due to collateral circulation • With hemodynamically significant stenoses of several coronary arteries, the dependence of impaired myocardial perfusion at rest on the degree of stenosis is almost linear, therefore multi-vessel damage is always associated with a worse prognosis • As a rule, even in the area of the previous infarction, a certain amount of viable myocardium remains (see . Heart disease is ischemic), therefore revascularization interventions improve the contractile function of the heart even in the area of infarction • When assessing the degree of damage to the coronary bed by atherosclerosis and choosing tactics, the following classification is used.
Classification of atherosclerosis of the coronary arteries (Petrosyan-Zingerman) • Anatomical type of blood supply to the heart •• Predominantly left (about 10%) •• Predominantly right (85–90%) •• Balanced (about 5%) • Localization of the lesion •• Trunk of the left coronary artery (CA) •• Anterior interventricular branch •• Circumflex branch •• Diagonal branch •• Right CA •• Blunt edge branch •• Other arteries • Extension of lesion •• Local stenosis •• Diffuse stenosis • Localization of stenoses •• Proximal segment of artery •• Middle segment of the artery •• Distal segment of the artery • Degree of luminal stenosis •• Without stenosis •• Moderate (less than 50%) •• Severe (less than 75%) •• Severe (from 75% to subtotal stenosis) •• Occlusion • Collateral blood flow • • Anastomoses between the anterior interventricular and circumflex branches •• Anastomoses between the circumflex branch and the right coronary artery •• Anastomoses of the circle of Viessen-Tebezia •• Other anastomoses.
Clinical picture and diagnosis.
• Complaints and objective examination - see Coronary heart disease.
• Instrumental methods •• ECG, chest x-ray, echocardiography, radioisotope study, stress tests - see Ischemic heart disease •• Intravascular ultrasound of the coronary arteries ••• Indications: •••• stenting of narrow coronary arteries; •••• restenosis after stent implantation; •••• unsatisfactory results of percutaneous transluminal coronary angioplasty; •••• questionable stenoses, especially of the trunk of the left coronary artery; •••• stenosis and implantation of stents in the mouths of arteries; •••• the need to assess the extent of stenosis and vessel diameter before endovascular interventions; •••• additional indications are under development ••• Methodology •••• Determine the cross-sectional areas of the coronary artery, the degree of stenosis, the transverse area of the residual lumen in the area of maximum stenosis, the length and eccentricity index of the plaque •••• If three-dimensional reconstruction is possible determine the volume of the plaque and its structure throughout •••• A study in color Doppler mapping mode is carried out when there are difficulties in interpreting the area of the lumen of the vessel that arise in the area of lipid plaques with a thin cap, and during coronary artery stenting, when measurements of the coronary artery lumen in the area of implantation can be significant influence further tactics •• Ultrasound of coronary bypass grafts ••• Indications •••• Transthoracic ultrasound of pedicle coronary bypass grafts is performed for all patients in the immediate period after coronary bypass surgery •••• Intravascular ultrasound of coronary bypass grafts is performed for endovascular correction of coronary bypass graft stenoses in the postoperative period •••• Additional indications are under development ••• Technique •••• Transthoracic ultrasound of pedicled mammarocoronary bypass grafts, pedicled coronary artery bypass grafts from the gastroepiploic artery, as well as intravascular ultrasound of coronary bypass grafts are feasible in almost all patients ••• • Transesophageal and transthoracic ultrasound of autovenous coronary artery bypass grafts appear to be futile •••• Transesophageal and transthoracic ultrasound of autoarterial coronary artery bypass grafts is under development •• Ultrasound of arteries and veins used as coronary artery bypass grafts ••• Performed in all patients before coronary artery bypass grafting ••• Determine the presence of the corresponding arteries, their diameter, length, their possible stenosis in case of damage by atherosclerosis or other pathological processes, anomalies in the development of arteries, volumetric blood flow in them ••• When using saphenous veins of the lower extremities as coronary bypasses, diagnose varicose veins ••• When using internal mammary arteries as shunts, ultrasound of the subclavian arteries is also performed ••• When ultrasound of the radial and ulnar arteries is performed, the Allen compression test is performed to determine the anatomical type of blood supply to the hand •• X-ray contrast selective coronary angiography ••• Indications: performed on all patients, initially admitted with a diagnosis of myocardial infarction, who have suffered acute coronary events, with clinical symptoms in patients with chronic forms of coronary artery disease, as well as with positive results of stress testing ••• Methodology •••• Typically, radiopaque selective coronary angiography is performed from a transfemoral approach, but with severe atherosclerosis of the femoral arteries, it can be performed from other approaches •••• In most cardiological centers, catheterization of the coronary arteries is carried out using the Judkins controlled catheter technique •••• The study reveals the indicators indicated in the heading Classification of atherosclerosis of the coronary arteries •••• When planning endovascular treatment, except assessment of the localization and degree of stenosis of the coronary artery, the presence, severity of calcification and angioarchitecture of the coronary arteries (in particular, tortuosity of the artery, lateral branches, etc.) are important in the area of possible transcatheter correction •••• When planning coronary bypass surgery, information about the structural and morphological features is obtained coronary artery distal to the stenosis, where a coronary bypass can be applied, as well as the functioning of collateral circulation in the area of impaired myocardial vascularization.
TREATMENT
Drug therapy - see Coronary heart disease.
Surgery.
• Indications: in general, the indications are determined by the anatomical type of coronary atherosclerosis, left ventricular function and, to a much lesser extent, the clinical picture of the disease.
• General indications for endovascular treatment •• One- or two-vessel coronary artery disease with stenosis or occlusion of type A or B according to the classification given below •• The introduction of new methods of endovascular treatment (stenting, laser revascularization) allows interventions in some cases with type stenosis WITH.
• Angiographic characteristics of stenoses by type •• Type A (minimal complex) ••• Local (less than 10 mm) ••• Concentric ••• Easily passable ••• Non-curved segment (<45°) ••• Incomplete occlusion ••• No major branches in the area of stenosis ••• No thrombosis ••• Smooth contour ••• Little or no calcification •• Type B (medium complex) ••• Tubular (10–20 mm) ••• Eccentric ••• Slight tortuosity proximal segment ••• Slightly curved segment (45–90°) ••• Total occlusion less than 3 months ••• Stenosis at the bifurcation, requiring the use of two guidewires ••• Thrombosis ••• Irregular contour ••• Moderate or severe calcification •• Type C (severe complex) ••• Diffuse (more than 20 mm) ••• Eccentric ••• Marked tortuosity of the proximal segment ••• Very curved segment (>90°) ••• Total occlusion, existing for more than 3 months, with developed collaterals ••• Impossibility of bypassing all major branches in the area of stenosis ••• Thrombosis ••• Irregular contour ••• Severe calcification.
• Contraindications to endovascular treatment •• Absolute: end-stage circulatory failure •• Relative ••• Type C stenoses ••• Poor short-term prognosis for life due to concomitant diseases (for example, malignant neoplasms with distant metastasis) ••• Diffuse distal sclerosis coronary arteries (X-syndrome).
• Specific complications of endovascular treatment •• Perioperative MI due to dissection, intimal volvulus, spasm or thrombosis of the coronary artery •• Restenosis due to progression of atherosclerosis, arteritis or hyperplastic reaction in the area of stent implantation •• False aneurysms at the access site •• Adverse reactions associated with use contrast media.
• General indications for coronary artery bypass grafting •• Hemodynamically significant stenosis of the trunk of the left coronary artery •• Variant of the trunk lesion (stenosis of the anterior interventricular branch, circumflex branch, right coronary artery) •• Two-vessel and single-vessel lesion with hemodynamically significant proximal stenosis of the anterior interventricular branch •• Two-vessel lesion without proximal stenosis of the anterior interventricular branch with a decrease in the contractile function of the left ventricle, severe ischemia, tolerant to conservative treatment, and also when stenotic vessels supply blood to a large volume of viable myocardium •• MI during the course or relapse of MI, refractory to intensive conservative therapy •• MI accompanied by left ventricular insufficiency in the presence of coronary artery stenosis, providing blood supply to viable myocardium beyond the developed necrosis •• Coronary artery bypass grafting as a primary reperfusion strategy in the early stages (no later than 6–12 hours) MI with ST segment elevation •• One- or two-vessel lesion that caused the onset life-threatening ventricular arrhythmias, especially if the patient has undergone resuscitation for arrhythmic cardiac arrest or there is sustained ventricular tachycardia •• Failure of percutaneous transluminal coronary angioplasty with persistent ischemia threatening coronary artery occlusion involving a significant volume of myocardium in the risk area •• Foreign body in the coronary artery in a position that threatens cessation of blood flow •• Ischemia of viable myocardium, tolerant to drug and endovascular correction, outside the blood supply zone of a functioning mammarocoronary shunt to the anterior interventricular branch.
• Contraindications to coronary artery bypass grafting •• Absolute: end-stage circulatory failure •• Relative: diffuse distal sclerosis of the coronary arteries (X-syndrome); unfavorable short-term prognosis for life due to concomitant diseases (for example, malignant neoplasms with distant metastasis).
• Specific complications of coronary artery bypass surgery •• Perioperative MI •• Osteomyelitis of the sternum with flap isolation of both internal mammary arteries •• Ischemia of the hand after isolation of the radial artery with a predominantly radial type of blood supply to the hand.
Prognosis • Has a pronounced dependence on the anatomical variant of the lesion of the coronary arteries, left ventricular function, the presence of rhythm disturbances and concomitant pathology • Surgical treatment has little effect on the prognosis for life expectancy, with the exception of cases of three-vessel and stem lesions • Coronary artery bypass grafting has advantages over endovascular correction in in terms of quality of life, frequency of restenosis and the need for repeated interventions • Endovascular treatment has advantages over coronary artery bypass surgery in terms of the duration of hospital treatment, its cost (in Russia this is true only if intervention on one vessel is necessary).
Synonyms: Coronary heart disease, Coronary disease (heart).
Abbreviations • CA – coronary artery
ICD-10 • I25.1 Atherosclerotic heart disease
Complications
Atherosclerosis of the lower extremities is dangerous due to the development of gangrene, muscle atrophy, and thromboembolism of blood vessels of vital organs in the event of plaque rupture.
Cardiac complications with damage to the coronary vessels include myocardial infarction, focal dystrophy of the heart muscle, myocardiosclerosis, and coronary sclerosis.
With obstruction of the mesenteric arteries, ischemic colitis and intestinal gangrene are possible, and secondary arterial hypertension is possible in the renal arteries. Cerebral consequences include hemorrhagic and ischemic stroke, transient ischemic attacks, and atherosclerotic dementia.
An aortic aneurysm poses a danger to the patient's life, the rupture of which in most cases is fatal.
What is myocardial infarction?
Myocardial infarction is an acute form of coronary artery disease in which part of the heart muscle dies as a result of blockage of the coronary artery. Most often, myocardial infarction occurs as a result of the formation of a blood clot on the surface of an atherosclerotic plaque inside a coronary artery.
The mechanism of a heart attack is quite complex. One of the important factors is inflammation of the vascular wall in the area of the plaque. Oddly enough, blood clots most often form on small plaques, the covering of which cracks, which leads to thrombosis.
Prevention of atherosclerosis
For patients with a family history and age-related predisposition, a screening examination is recommended to determine the risk of developing cardiovascular pathology.
It aims to detect laboratory and genetic markers of the disease. Prevention of atherosclerosis includes weight control, proper nutrition, sufficient physical activity, giving up bad habits, and timely treatment of chronic diseases.
Author:
Pugonina Tatyana Alekseevna, Therapist