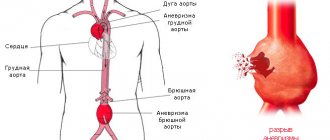
Aneurysms of the extracranial ICA are a rare pathology. They account for 1-2% of all lesions of the extracranial parts of the carotid arteries [1-4] and 0.8-4% of aneurysms of other peripheral vessels [5, 6]. In a study by the Texas Heart Institute, among 7394 patients with aortic and peripheral artery aneurysms who were operated on at this center from 1960 to 1995, 67 (0.9%) patients were diagnosed with ICA aneurysm [7]. A.V. Gavrilenko et al. [2], analyzing the experience of surgical treatment of 1836 patients, identified aneurysms of the extracranial parts of the ICA in 31 (1.7%) patients.
The main reasons for the formation of carotid artery aneurysms, according to most authors [8-10], are atherosclerosis, fibromuscular dysplasia and traumatic damage to the arteries. The presence of an aneurysm of this location primarily threatens the development of ischemic cerebrovascular accidents (ICDs) in the form of TIA and ischemic stroke due to distal embolism from the aneurysm cavity. Arterio-arterial embolism in this pathology is a consequence of turbulence of blood flow in the aneurysm cavity with the washing out of thrombotic masses from the aneurysmal sac. In addition, as in cases with aneurysms of other locations, thrombosis is possible [1, 11]. When studying the natural history of carotid aneurysms in 124 patients described before 1936, N. Winnslow found that the mortality rate from thrombosis, distal embolism and rupture in this pathology was 71%. According to R. Busuttil et al. [12], episodes of ischemic cerebrovascular accidents were observed in 50% of patients. Other authors [13, 14] reported that their frequency is 43-74%, with TIAs occurring 2 times more often.
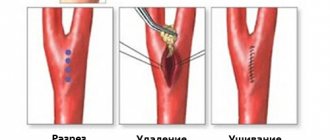
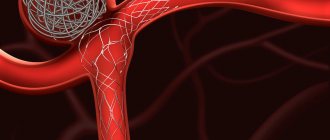
Considering the risk of stroke and the high mortality rate associated with this pathology, various methods of surgical interventions have been proposed. The main goal of surgical treatment is to prevent thromboembolism. Since the first operation performed by A. Cooper [7] in 1805, vessel ligation has been the only method of surgical treatment. These interventions were accompanied by the development of a major stroke or death in 20-40% of cases [14, 15]. Currently, in most cases, resection of the ICA aneurysm is performed with replacement of the latter or the formation of an end-to-end anastomosis [1, 2, 4, 11, 14-16]. Carrying out reconstructive surgery can reduce the development of stroke and mortality to 4-10% [3, 9]. The greatest difficulties arise during operations for aneurysms of the distal parts of the ICA. According to a number of authors [17, 18], distally located extracranial aneurysms are formed due to pathological deformation of the carotid arteries due to an extreme form of vascular wall dysplasia. In many cases, they are complicated by the presence of thrombotic masses in the cavity of the aneurysmal sac. The literature [1, 11, 17, 18] describes isolated cases of open surgical interventions for this type of lesion, but with a more proximal location of the aneurysm. The development of endovascular surgery in recent years has expanded the capabilities of surgeons in choosing options for surgical treatment of ICA aneurysms. However, so far in the literature [19-22] there are only isolated or small in number of observations descriptions of endoprosthetics for this pathology. The use of stent grafts in the carotid arteries is associated with the risk of intimal dissection and arterial thrombosis, and in cases of severe tortuosity of the artery is not always technically feasible. At the same time, in recent years, reports have appeared on the successful use of high-flow extraanatomical ECA-MCA bypass (in English literature - High-flow EC-IC bypass) in the treatment of complex aneurysms of the intracranial ICA [23]. Having some experience in this type of operations, we applied this technique in the treatment of distally located aneurysms of the extracranial part of the ICA.
The article presents the experience of successful surgical treatment of distally located aneurysms of the extracranial part of the ICA, combined with pathological tortuosity of the artery.
Material and methods
In 2015, in the Department of Vascular Neurosurgery of the Federal Center for Neurosurgery of Novosibirsk, 3 surgical interventions were performed on patients diagnosed with “Pathological tortuosity of the ICA with the formation of a saccular aneurysm of the distal C1 segment.” All patients were aged 62-63 years. All of them had a history of cerebrovascular accident in the MCA region on the affected side of the ICA: in 2 cases - ischemic stroke, in 1 - repeated TIAs. The patients underwent osteoplastic craniotomy, creation of a high-flow extra-anatomical shunt between the ECA and M2 segment of the MCA, and proximal ligation of the C1 segment of the ICA.
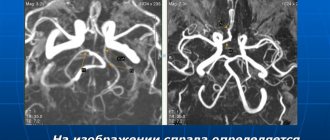
When deciding on the choice of surgical intervention method, in addition to general clinical examinations, data from duplex scanning of the brachycephalic arteries (DS BCA), transcranial Doppler ultrasound (TCDG), multislice computed tomographic angiography (MSCT angiography) and magnetic resonance imaging (MRI) of the brain were taken into account. According to the results of DS of the BCA, all patients revealed a disturbance in the course of the ICA in the form of pathological tortuosity of various shapes with a BSC from 150 to 230 cm/s. Aneurysmal dilatation according to ultrasound data was detected only in 1 case. More complete information was obtained from MSCT angiography of extra- and intracranial arteries, which in all cases revealed pathological tortuosity of the distal ICA of varying severity. In 2 cases, saccular aneurysms measuring 8 and 12 mm were detected at the level of the atlantoaxial joint, with partial thrombosis of the aneurysmal sac (Fig. 1). In 1 observation, an area of intimal tear with fusiform widening of the distal ICA was identified above the aneurysm.
Rice. 1. MSCT-3D angiography of the BCA. The arrow indicates a distally located ICA aneurysm in combination with pathological tortuosity of the artery.
The operations were performed under general anesthesia. At the first stage, the bifurcation of the common carotid artery (CCA) was identified using standard access. At the same time, the radial artery was collected. The average length of the shunt was 22.5 cm. The diameter in the proximal segment ranged from 2.5 to 3.4 mm, in the distal segment - from 2.1 to 3.1 mm. After craniotomy, the M2 segment of the MCA was isolated and temporary clips were applied to it. Then, a longitudinal arteriotomy of the M2 segment of the MCA was performed, and a distal anastomosis was formed with the distal radial artery in an end-to-side manner (Fig. 2). The clips were removed from the SMA. The average MCA clamping time ranged from 35 to 44 minutes. The shunt was performed in the subcutaneous preauricular tunnel or under the zygomatic arch into a wound on the neck.
Rice. 2. Formation of a distal anastomosis between the M2 segment of the MCA and the autoarterial shunt.
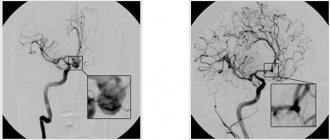
After clamping the ECA, a proximal end-to-side anastomosis was formed between the initial section of the ECA and the graft (Fig. 3). After removing the clamps, blood flow through the shunt and MCA was monitored using Dopplerography, flowmetry and indocyanine green video angiography (ICG-VA) with temporary clamping of the ICA in the area of the mouth (Fig. 4). While maintaining adequate blood flow through the intracranial arteries, ligation of the ICA at the ostium and suturing of surgical wounds were performed. On the 1st day after the intervention, all patients underwent control MSCT angiography of extra- and intracranial vessels (Fig. 5). In the immediate hours after surgery, the extracranial ICA thrombosed to the level of the origin of the ophthalmic artery without the development of neurological symptoms (Fig. 6).
Rice. 3. Formation of a proximal anastomosis between the ECA and the autoarterial shunt.
Rice. 4. Intraoperative control (ICG-VA). The arrow indicates the distal anastomosis.
Rice. 5. MSCT control of the distal anastomosis. The arrow indicates the distal anastomosis between the M2 segment of the MCA and the autoarterial shunt.
Rice. 6. MSCT control after surgery. There is a lack of contrast enhancement of the ICA in the extracranial region. The arrow indicates the high-flow extra-anatomical shunt NSA-SMA (High-flow EC-IC bypass).
No complications of surgical interventions were noted. The patients were discharged in satisfactory condition on the 8-10th day after surgery; they were recommended to undergo antiplatelet therapy. At follow-up examinations after 3, 6 and 9 months, all patients were in satisfactory condition, their neurological status was without negative dynamics. According to control DS BCA and MSCT angiography, shunt patency was maintained in all cases.
Treatment of aneurysms in pediatric patients
Cerebral aneurysms in children are rare and can be combined with various connective tissue pathologies (Marfan’s syndrome, Ehlers-Danlos’s syndrome) and various developmental anomalies of the circle of Willis. In children, aneurysms with complex anatomical characteristics are detected three times more often than in adults. Pseudotumorous and ischemic types of course in “children’s” aneurysms occur several times more often than in adults. Incidentally discovered aneurysms in children are rare. The principles of surgical treatment of aneurysms in children are generally the same as in adults. It should be noted that the compensatory capabilities of a child in the event of the development of any complications are greater than those of adults, so children can more easily tolerate the switching off of the arteries carrying the aneurysm. In this regard, deconstructive operations can be considered as the method of choice in cases of complex aneurysms when it is impossible to switch off the aneurysm while maintaining arterial patency.
Discussion
Many authors indicate that aneurysms of the extracranial ICA should be operated on regardless of the presence of symptoms [2, 17]. The greatest difficulties arise during surgical treatment of aneurysms of the distal parts of the ICA in combination with pathological tortuosity of the artery. In patients in our small series, aneurysms were located close to the entrance to the skull. Based on our own experience in performing endovascular and open surgical interventions for aneurysms of the extracranial part of the ICA [24], we considered it rational to abandon conventional operations and apply a different method of surgical treatment. When reviewing the literature, we did not find data on the operation of forming a high-flow extra-anatomical ECA-MCA bypass (High-flow EC-IC bypass) in patients with distally located ICA aneurysms in combination with pathological tortuosity. There are references to the use of this operation in the treatment of complex cerebral aneurysms [23, 25]. We extrapolated a well-established technique used in the treatment of complex intracranial aneurysms to a group of patients with distally located aneurysms of the extracranial ICA. We consider this operation to be less traumatic and safe for the patient, since it does not require complex access to the altered section of the artery, including the intersection of the sternocleidomastoid muscle, the posterior belly of the digastric muscle, resection of the styloid process, and displacement of the mandible. Modifications of access to the distal ICA described in the literature are also very traumatic. Thus, E. Rosset et al. [3] to access aneurysms located at the base of the skull, opening of the external auditory canal, resection of the styloid process, and resection of the mastoid process are used. U. Fish et al. [26] described access to the ICA siphon by subtotal petrosectomy, anterior advancement of the facial nerve, and obliteration of the middle ear cavity. However, there is a high incidence of complications, primarily damage to the cranial nerves. The surgical treatment method we used is not routine. This operation should be performed by surgeons with appropriate experience. Careful selection of patients with analysis of the possibilities of alternative treatment methods is also necessary. Our experience has shown that the volumetric blood flow through the shunt (up to 250 ml/min according to flowmetry data) sufficiently ensures adequate blood supply to the brain after surgery. The results of our operations, the absence of neurological and local complications, confirmed the correctness of the choice of surgical treatment for these patients.
Microsurgical treatment of asymptomatic aneurysms
Until recently, asymptomatic aneurysms were detected extremely rarely. In recent years, the widespread availability and availability of noninvasive neuroimaging techniques has led to a significant increase in the number of patients with incidentally discovered aneurysms. Over the past 10 years, the institute has operated on about 400 patients with asymptomatic aneurysms. The results of surgical treatment in this category of patients should be considered satisfactory. Taking into account these data, as well as the extremely high probability of an unfavorable outcome in case of rupture of an aneurysm, it can be argued that unruptured asymptomatic aneurysms in most cases require surgery. It should be noted that the patient must be fully informed about the nature of the disease, the upcoming operation and possible complications.
Causes of development of vertebral artery syndrome
There are several main reasons for the development of cervical-vertebral syndrome in humans, among which are:
- osteochondrosis and other degenerative-dystrophic disorders in segments of the cervical spine;
- congenital anomalies of the structure of the bone elements of the neck;
- consequences of injuries in the area of the vertebral artery;
- pathological conditions that negatively affect the state of the sympathetic arterial plexus;
- atherosclerotic lesions of the vertebral arteries and other pathologies of the vascular wall;
- tonic muscle spasms in the neck;
- defects in the structure of the cervical vessels.
Qualified treatment for vertebral artery syndrome of the cervical spine should be carried out regardless of the causes of the development of the painful condition. Its scope and basic methods largely depend on the nature of the disease. Therefore, when symptoms of pathology appear, you should not self-medicate them, but immediately seek help from specialists who have experience in such clinical situations.
Diagnostics
Before treating vertebral artery syndrome, the doctor refers the patient to undergo a full diagnosis of the condition of his body. For this disease, diagnostic measures include a number of important methods:
- X-rays in the neck area, which helps determine areas of vascular compression;
- angiographic examination of the vessels of the neck to determine their patency, the presence of areas of narrowing of the lumen, deformations, etc.;
- ultrasound examination of the neck and diagnosis of the condition of blood vessels, muscles, determination of the nature of blood flow, the presence of areas of atherosclerosis;
- MRI in the neck with a more in-depth study of all the nuances and disorders;
- biochemical blood test to determine cholesterol levels and the degree of development of atherosclerosis.
Symptoms
The following clinical symptoms are characteristic of vertebral artery syndrome:
- headaches, which in the case of vertebral artery syndrome are localized in the occipital zone with a transition to the front of the head and can appear after sharp turns of the neck or after sleep (Barré-Lieu syndrome);
- migraine pain of a basilar nature, which is often accompanied by loss of consciousness;
- sudden falls with throwing back of the head and loss of coordination;
- loss of normal stability and ability to maintain balance along with nausea, vomiting, dizziness, darkening of the eyes;
- development of transient ischemic attacks;
- short-term fainting states after sudden movements of the head;
- pain and feeling of “sand” in the eyes, dysfunction of the visual analyzer, loss of visual fields, etc.;
- hearing loss, tinnitus;
- hot flashes with excessive sweating;
- sometimes pain in the heart area.
Identifying the symptoms of vertebral artery syndrome is not a problem for an experienced specialist. Therefore, when the first signs of illness appear, you should not postpone a visit to the doctor, who will be able to conduct a high-quality diagnosis of the pathological condition and begin treatment on time.