The carotid artery is a paired large blood vessel that rises to the head along the anterolateral surface of the neck on the right and left. It originates in the chest cavity, branching from the aorta, the main artery of the human body that supplies blood to all internal organs. The division of the carotid artery into external and internal trunks (bifurcation) occurs in the area of the thyroid cartilage of the larynx, hyoid bone or under the lower jaw. The outer part provides blood supply to the face, neck and scalp, while the inner part supplies blood to the brain.
Features of the pathology
This pathological process cannot be called a disease. Trifurcation is a structural feature of the Circle of Willis. This unusual structure of the arteries occurs quite often, in more than 20% of people. The pathology is still not normal, since some branches of the divided arteries may deliver insufficient blood to the brain due to the development of an aneurysm.
This structure of the Circle of Willis is considered the norm for an embryo located inside the womb in the first half of its development. During the growth process, the structure of the blood vessels changes, and they take on their usual state. But in some cases, their fusion does not occur, they retain the same size, and trifurcation of the internal carotid artery develops.
With anterior trifurcation, the artery delivers only 50% of the blood to the brain, and the posterior trifurcation only 10%, which is the result of hypoplasia of the proximal segment. Most scientists in this field argue that the non-classical structure of the circle of Willis can cause the formation of an aneurysm in any of its parts.
Causes and types of trifurcation
At the base of the brain lies a vascular formation in the shape of a polygon, the functions of which include the redistribution of blood flow from different pools when a deficiency occurs in one or another branch of the cerebral blood supply. In honor of the English physician Thomas Willis, who discovered and described this formation more than three hundred years ago, it is called the Circle of Willis.
Normally, the vessels of the circle should form a closed system, but sometimes there is a splitting of the internal carotid arteries included in its composition into three smaller vessels, which is called trifurcation. She may be:
- anterior - divided into anterior, posterior and basilar trunks;
- posterior - divided into anterior, middle and posterior cerebral arteries.
This feature of the cerebral vascular system is characterized as atavism of intrauterine development. In the first half of the period of fetal formation, such branching is the norm, but as it develops, the vessels unite and enlarge. However, sometimes this does not happen; triple cleft of the carotid artery remains with the person for life. This feature is found in all inhabitants of the planet with a frequency of 14 to 25% of the total population.
Depending on which of the paired vessels is subject to trifurcation, it is called right- or left-sided. Trifurcation can be complete when the branching of the internal artery, present in the prenatal state, is completely preserved, and incomplete when the vessels connect to a certain level and then divide into three branches.
On the one hand, the phenomenon is not considered a pathology, but only one of the variants of the structure of the circle of Willis; on the other hand, both complete and partial posterior or anterior trifurcation of the internal carotid artery can create favorable conditions for the occurrence of various vascular diseases, or aggravate their course.
Structure of the Circle of Willis
The branching of the carotid artery consists of many vessels that are located in front of the base of the brain. Such a formation can be considered a reserve system that will work if the brain is insufficiently supplied with plasma, oxygen and nutrients. This special system is designed to compensate for problems with blood flow, since it is able to pump blood to the brain from other sources in the body. The usual structure of the Circle of Willis has a closed system of arteries that feed the brain structures.
During trifurcation, due to the uneven flow of blood through the vessels and arteries, some unpleasant phenomena may occur.
Such pathological conditions will have the following symptoms:
- Dizziness;
- Pain in the temples and back of the head;
- The manifestation of significant and pronounced symptoms of migraine.
If a patient with trifurcation develops an aneurysm, then symptoms may appear only when the vessels rupture. At this moment, the blood will flow into the subarachnoid area and the patient will begin to feel intense headaches. Unbearable pain is often accompanied by nausea and vomiting. The patient feels strong tension in the muscle structures in the back of the head and becomes sensitive to bright light.
Symptomatic picture
In youth, trifurcation of the carotid artery in itself does not affect human health in any way. The lack of blood flow in the ICA is compensated by the high patency of other arteries and good elasticity of the vessel walls. Symptoms associated with this feature of the structure of blood vessels most often begin to appear in old age, when, as pathological signs accumulate, the condition of the vascular system as a whole worsens and it becomes unstable. But if clefting is accompanied by other abnormalities, it can make itself felt in a young person.
Trifurcation of the left or right internal carotid artery causes uneven blood flow to the brain. Hypoplasia (underdevelopment) of vascular branches leads to the fact that the intensity of blood flow through them varies significantly. With anterior trifurcation, the anterior cerebral artery accounts for 50% of the total volume of blood flowing through this artery, and the basilar trunk accounts for only 10%. Against the background of hypoxia of certain areas of the brain, the following symptoms may develop:
- Headache - usually in the temples and back of the head.
- Attacks of dizziness and nausea.
- Migraine with pronounced aura.
When complete posterior trifurcation of the right or left internal carotid artery accompanies a vascular aneurysm in the cerebral region, against the background of uneven blood pressure in different branches, the risk of its rupture and hemorrhage in the subarachnoid cerebral zone increases. In this case, the level of pain increases sharply, severe vomiting may begin, and the reaction to bright light worsens. Another symptom of a ruptured cerebral aneurysm is spasmodic tension in the back muscles of the neck and back of the head. In such a situation, it is necessary to call an ambulance as quickly as possible.
Failure to provide medical care in a timely manner leads to the development of severe complications that cause disability, and in the most difficult cases it can result in death.
Diagnostics
Some people are not even aware of their special structure of the internal carotid artery. In most cases, anterior trifurcation of the ICA is discovered by chance when a person decides to conduct a brain examination in connection with completely different diseases. Magnetic resonance imaging helps to identify this feature. If necessary, contrast angiography is used to obtain a clearer and clearer vascular picture.
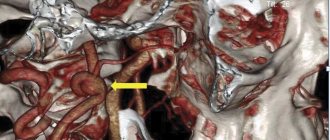
In the resulting 3D-TOF images, trifurcation can be clearly identified. Clinical symptoms are determined by the absence of the right vertebral artery in the image and the origin of the anterior cerebral vessels from the right internal carotid artery. Such patients subsequently need consultation with a neurologist, who will prescribe a specialized course of therapy.
Variations in the development of cerebral arteries and epilepsy
The prevailing ideas about the mechanisms of development of cerebral ischemia imply the occurrence of a discrepancy between the available blood supply and the needs of brain tissue. The most important achievements in the field of clinical angioneurology include the modern concept of heterogeneity of ischemic stroke, which is based on the idea of the diversity of causes and mechanisms of development of acute focal ischemic brain damage. The amount of reversible and irreversible brain damage largely depends on the state of the hemodynamic, collateral, perfusion and metabolic reserves of the brain. Pathological tortuosity of the main arteries of the head - a hereditarily determined functional inferiority of connective tissue - occurs in at least 10% of the population. Among the main forms of lesions of intracranial arteries, kinks and loop formations, aneurysmal dilatations of arteries, and arteriovenous aneurysms are distinguished. Excessive tortuosity of blood vessels contributes to the formation of blood clots in them. In 71% of patients with arterial occlusion, a tortuous course of vessels was noted. Underdevelopment of the cerebral arteries in the form of hypoplasia or stenosis of the posterior inferior cerebellar artery and/or basilar artery, rarely the inferior anterior cerebellar artery and tortuosity of the vertebral artery are causes of hearing loss and deafness. Weak cerebral artery anastomoses cause cerebral ischemia after cervical discectomy. In Parkinson's and Alzheimer's diseases, neuroimaging and pathological studies have detected cerebrovascular lesions in 20-30% of cases, and vascular disease of the brain may be the basis of dementia. Structural changes in cerebral vessels, a decrease in blood flow velocity and the presence of 30% stenosis in the middle cerebral artery can be prerequisites for the development of stroke in patients with sleep apnea syndrome.
In case of Kimmerle anomaly, it is necessary to take into account the presence of congenital changes in the vertebral arteries. Dysplastic disorders in the area of the craniovertebral junction are 2 times more often noted with pathological tortuosity of the vertebral arteries, to a lesser extent due to hypoplasia of the vertebral arteries. Up to 51.9% of patients with Chiari malformation and syringomyelia have structural features of the cerebral arterial circle. Tortuosity, asymmetry and hypoplasia of the vertebral arteries with signs of impaired blood flow are characteristic of vertebrobasilar insufficiency due to cervical dorsopathy and were noted in 76.6% of cases with central vestibulocochlear syndrome.
The arterial bed of the brain is also affected in such systemic diseases of the body as rheumatoid arthritis, polyarteritis nodosa, Takayasu's disease, Henoch-Schönlein disease. When performing dental procedures in patients with Sturge-Weber disease or Recklinghausen disease, as typical neurofibromatosis, the development of threatening bleeding is possible. Primary damage to the cerebral arteries in the form of vasculitis and endarteritis underlies the development of neurosyphilis and leads to secondary damage to the nervous tissue and the occurrence of infarctions in the brain. Cerebral vasculitis and herpetic cerebral vasculitis can develop against the background of herpetic infection. With ischemic strokes, in 70% of cases in the brain tissue, along with changes caused by acute cerebrovascular accident, focal lesions are observed, similar to changes in meningoencephalitis caused by herpes zoster and herpes simplex.
Changes in the structure of the cerebral arteries must be taken into account when assessing cancer metastases, as well as in 40% of patients with severe traumatic brain injury when identifying traumatic subarachnoid hemorrhages and concomitant angiographic vasospasm.
In the course of carrying out research to study the relationship between variants of human cerebral arteries and cerebrovascular disorders within the framework of acute cerebrovascular accidents and chronic cerebral ischemia, we have developed observations about the relationship between variants of the structure and topography of human cerebral arteries with a number of other nosological units. In this regard, we present the results of our own research on the development of cerebral arteries in humans with various types of epilepsy.
We analyzed the state of the arterial bed of the brain in 748 outpatient and inpatient patients from 22 years to 81 years old, who were examined and treated in the neurological and neurosurgical departments of OKB No. 2 named after. Professor I.N. Alamdarov, Astrakhan in the period 1983-1998, the neurological departments of City Hospital No. 3 and City Hospital No. 4 of Tambov, the neurosurgical department of the Tambov Regional Hospital, the rehabilitation and health complex of the family “B. Lipovitsa", neurological offices and in day hospitals of City Hospital No. 4, Nodal Clinic at the station. Tambov JSC "Russian Railways" and the Central House of Children's Hospital "Tambovmedservice" LLC, as well as in the outpatient clinic "Home Doctor" (Tambov) during 1998-2009.
All patients underwent a comprehensive clinical and instrumental study, including data from a clinical examination by a neurologist, therapist and ophthalmologist, standard laboratory data, electrocardiography, fluorography or plain radiography of the chest organs. According to indications, consultations and examinations were carried out with a neurosurgeon, gynecologist, otolaryngologist, cardiologist, endocrinologist and psychotherapist; a study of the cognitive sphere using a brief mental status assessment scale or a mini-mental status study, transcranial Doppler sonography, electroencephalography. All patients underwent magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA).
According to the data obtained, variants of the structure and topography of the arterial circle of the cerebrum were verified in only 27 cases (61.4% of observations) out of 44 patients with epilepsy or encephalopathies with leading epileptiform syndromes. Among the analyzed group of patients with various types of epilepsy, the following variants of the structure and topography of the arterial circle of the cerebrum were identified: 1) bending of both anterior cerebral arteries in 1 (3.7%) patient; 2) hypoplasia of the left vertebral artery in 2 (7.4%) patients; 3) posterior trifurcation of both internal carotid arteries and anterior trifurcation of the left internal carotid artery, hypoplasia of the basilar artery in 3 (11.1%) patients; 4) anterior trifurcation of the left internal carotid artery, hypoplasia of the basilar artery in 6 (22.2%) patients (Fig. 1); 5) hypoplasia of the right vertebral artery, aplasia of the posterior communicating artery on the right in 4 (14.8%) patients; 6) hypoplasia of the right vertebral artery, hypoplasia of the basilar artery in 5 (18.5%) patients (Fig. 2); 7) anterior trifurcation of the left internal carotid artery, hypoplasia of the posterior communicating artery, hypoplasia of the right posterior cerebral artery in 3 (11.1%) patients; tortuosity of both vertebral arteries in 2 (7.4%) patients; 9) hypoplasia and tortuosity of both vertebral arteries in 1 (3.7%) patient. Below are quite indicative clinical observations from the totality of our own studies.
Among the analyzed group of patients with various types of epilepsy, the following variants of the structure and topography of the arterial circle of the cerebrum were identified: 1) bending of both anterior cerebral arteries in 1 (3.7%) patient; 2) hypoplasia of the left vertebral artery in 2 (7.4%) patients; 3) posterior trifurcation of both internal carotid arteries and anterior trifurcation of the left internal carotid artery, hypoplasia of the basilar artery in 3 (11.1%) patients; 4) anterior trifurcation of the left internal carotid artery, hypoplasia of the basilar artery in 6 (22.2%) patients (Fig. 1); 5) hypoplasia of the right vertebral artery, aplasia of the posterior communicating artery on the right in 4 (14.8%) patients; 6) hypoplasia of the right vertebral artery, hypoplasia of the basilar artery in 5 (18.5%) patients (Fig. 2); 7) anterior trifurcation of the left internal carotid artery, hypoplasia of the posterior communicating artery, hypoplasia of the right posterior cerebral artery in 3 (11.1%) patients; tortuosity of both vertebral arteries in 2 (7.4%) patients; 9) hypoplasia and tortuosity of both vertebral arteries in 1 (3.7%) patient. Below are quite indicative clinical observations from the totality of our own studies.
Example 1. Patient N., 54 years old, is observed in the Nodal clinic at the station. Tambov JSC "Russian Railways" with a diagnosis of encephalopathy as unspecified (epileptic and dyscirculatory) with polymorphic paroxysms (like Todd's palsy) against the background of abnormalities in the structure of the cerebral arteries. Complaints of noise in the head, unsteadiness when walking, attacks of weakness in the right limbs and loss of consciousness. Neurologically: there are no meningeal signs in consciousness, cognitive functions are reduced, emotionally labile, pupils d = s, convergence is weakened, slight weakness of the facial muscles on the right, paresis of the right hand up to 4 points, no sensory disorders, tendon reflexes are increased d > s, staggering in the Romberg position , coordination tests are performed with DetS missing, eyelid tremor. Ophthalmologist: hypertensive angiosclerosis of the retinal vessels of both eyes. Therapist: stage II hypertension, severity of arterial hypertension II, risk category 3. BAC: cholesterol - 4.5 mmol/l, β-lipoproteins - 3.5 g/l, creatinine - 69 µmol/l, urea - 7, 9 mmol/l. Prothrombin - 88%, fibrinogen - 4.25 g/l. ECG: syn, rhythm 80 per minute, normal position of the EOS. MRI and MRA: shown in Figure 1. Outpatient treatment: piracetam, glycine, Cavinton, cinnarizine, aminalon, Enap, Prestarium, indopamine. She underwent a course of treatment in a day hospital: Mexidol, magnesium sulfate, Prestarium, indopamide, mildronate, enalapril. The complaints remain the same. Neurologically - there are no meningeal signs in consciousness, cognitive functions are reduced, cranial nerves without dynamics, paresis of the right hand up to 4.5 points, staggering in the Romberg test, coordination tests with intention on both sides. Consulted at the Tambov psychiatric hospital, where a diagnosis was made: consequences of organic damage to the central nervous system of complex origin with polymorphic paroxysms. EEG: pronounced cerebral changes in biological and bioelectrical activity, practically no α-activity. In all regions the polyri is less than 5 μm. There is no regionality, no activation reaction, no assimilation. Persistent disorganization of the activities of central structures. Interest in the left temporal region, where a focus of slow-wave irritation was identified. Low functional state of the cortex with high sensitivity to hypoxia, with a decrease in the threshold of excitability of the trunk. Single discharges of the posterior trunk sections. Vascular influences are pronounced. Follow-up: while taking Depakine-Chrono, complaints decreased significantly, no attacks were noted.
Example 2. Patient VN., 21 years old, is observed in the Nodal clinic at the station. Tambov JSC Russian Railways with a diagnosis of epilepsy with polymorphic cerebral paroxysms and cognitive impairment. Observed since childhood - complaints of attacks with loss of consciousness. After starting treatment at the age of 14 in the neurological department of the Tambov Regional Children's Hospital, he was registered with a diagnosis of epilepsy, partial seizures with secondary generalization. EEG (Psychiatry and Narcology, 04/17/02): no paroxysmal activity was detected, unstable α-rhythm. Dysfunction of the diencephalic region. Vascular influences with increased autonomic excitability (06/15/04): AMI is moderate, but persistent, with low-amplitude dysrhythmia. Regionality is unclear. The activation reaction is reduced, there is no assimilation. No gross slow-wave or paroxysmal activity was detected. Reduced reactivity of the cortex. High vegetative excitability. Vascular influences 02.22.05: compared to 06.15.04, positive dynamics. General cerebral changes are moderate and of a regulatory nature. Moderate dysfunction of the diencephalic region with increased activity. An unstable α-rhythm appeared, fragmented. The reactivity of the cortex has improved. The sensitivity of the cortex to RFS has increased somewhat, which leads to a decrease in the threshold of excitability of the posterior brainstem structures. There are no paroxysmal tendencies of the cortex. Increased autonomic excitability. MRI and MRA: shown in Figure 2. Neurologically: there are no meningeal signs in consciousness, cognitive functions are slightly reduced, emotionally labile, distal hyperhidrosis, tremor of the eyelids and outstretched fingers, pupils d = s, converges, weakness of facial muscles on the right, in the Romberg position lung staggering, performs coordination tests, paresis, no sensory disorders, tendon reflexes d = s, Babinski's symptom is weakly positive on both sides, Epileptologist: cognitive disorders due to epilepsy. He constantly receives finlepsin (attacks are associated with irregular use of the drug).
Thus, we consider it necessary to draw the following conclusions. 1. Variations in the structure and topography of the arterial circle of the cerebrum can be considered as predictors of epileptiform phenomena in brain structures. 2. For various cerebral paroxysms, it is obviously advisable to study the arterial circle of the cerebrum. 3. Variants of the structure and topography of the arterial circle of the cerebrum in each specific case should be considered from the point of view of minor developmental anomalies.
Treatment
If a posterior trifurcation or anterior internal carotid artery is detected, you should not fall into despair and look for ways to solve this problem. This special structure of the Circle of Willis does not require special therapy. The structure of these arterial vessels cannot cause serious pathologies, since they are an additional source of nutrients for the brain and increase blood circulation during thrombosis.
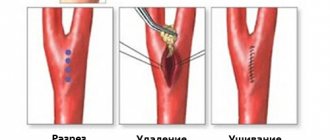
Treatment in a medical facility may only be required if complications develop, such as an aneurysm. To eliminate it, you will need surgical intervention, which consists of ligating the vessels at the site of complications. When opening an aneurysm, conservative treatment will be required, which is generally accepted for any pathology with cerebral hemorrhage.
Symptoms
The symptoms of pathological tortuosity of the carotid and vertebral arteries are varied. The most common symptoms are:
- so-called transient ischemic attacks (temporary interruptions in blood supply), accompanied by temporary paralysis of the upper limbs, speech impairment, temporary blindness;
- noise in the head, dizziness;
- migraine attacks;
- impaired coordination of movements, falls without loss of consciousness;
- short fainting spells.
Complications
Complications of trifurcation include the appearance of an aneurysm on any vessel. This pathology is determined immediately using an MRI or CT scanner. A feature of the formation of an aneurysm is the complete absence of signs of neurological diseases. No special treatment is provided in this case. Many concomitant diseases (hypertension, atherosclerosis, etc.) can also complicate the course of trifurcation.
Complications present with such a non-standard structure of blood vessels also include their increased length and the adoption of various unnatural shapes:
- Vascular pathology is very difficult to detect while they have soft bends at an obtuse angle. The clearly defined vessel has an ornate bend that can compress the main artery;
- Kinking. The direction of the artery forms an incomplete acute angle;
- Coiling. The artery takes the form of a loop, which significantly impairs blood flow. Symptoms of cerebral ischemia may also be present.
Features of the vessels, namely trifurcation of the left internal carotid artery, can lead to a narrowing of its lumen. This pathology occurs mainly in older people. Due to the formation of atherosclerotic plaques on the inner walls of the vessel, the lumen significantly narrows, which impairs blood circulation.
Such plaques are formed by fibrous tissue, cholesterol and calcium. When plaques become overgrown with platelets, complete blockage of arteries and vessels with a non-standard structure can occur.
The development of this complication can be prevented by using the following measures:
- Quitting bad habits (smoking and drinking alcoholic beverages);
- Regular exercise;
- Cholesterol-free diet;
- Body weight control.
If you detect a right posterior non-standard trifurcation of the internal carotid artery, you should not rush to search for specialists to eliminate this problem. This congenital feature of blood vessels is considered normal and does not require treatment. Regular periodic monitoring of their condition and diagnostics will be sufficient to avoid sudden complications.
Vessels
Anterior (Posterior) Atlanto Nuchal Membrane
Feb 06, 2021 Kokh V. A.
5900
Vessels
Arteries of the Head and Neck: Anatomy, Diagram, Atherosclerosis
Feb 06, 2021 Kokh V. A.
19218
Vessels