- Healthy Heart Library
- Acute heart failure
Heart failure is a condition that occurs in acute or chronic form.
Accompanied by a weakening of the contractility of the myocardial muscles and the development of congestion in both the pulmonary and systemic circulation. It is not an independent disease, since it usually occurs as a complication of coronary heart disease, arterial hypertension, cardiomyopathy and valvular heart disease. Heart failure is not an independent diagnosis.
Causes
The first place among the causes of acute heart failure is occupied by myocardial infarction and coronary heart disease, accounting for more than 60% of cases . Cardiomyopathies and rheumatic heart defects share second and third place - 11 and 14% of cases.
For older patients, hypertension (4% of cases of heart failure) and type 2 diabetes mellitus in combination with arterial hypertension are dangerous. A small percentage of cases of acute heart failure (AHF) are associated with trauma and severe blood loss.
Risk factors for AHF
When the compensatory functions of the heart muscles decrease, certain factors can provoke acute heart failure. Most of them are treatable, which reduces the risks for the patient.
The risk group is:
- physical and emotional stress;
- arrhythmia, pulmonary embolism, hypertensive crisis, ischemic heart disease;
- pneumonia, ARVI, anemia, renal failure;
- treatment with cardiotoxic drugs that promote fluid retention, drugs (NSAIDs, estrogens, corticosteroids) that increase blood pressure (isadrine, ephedrine, adrenaline);
- progressive and pronounced increase in body weight, alcoholism;
- myocarditis, rheumatism, infective endocarditis;
- hyperthyroidism.
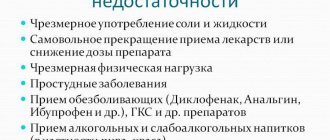
Violation of the treatment regimen for chronic heart failure can also contribute to the transition of the disease to the acute phase.
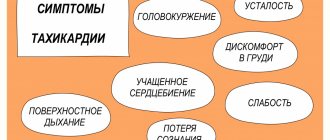
Symptoms of chronic heart failure
- One of the most characteristic symptoms of heart failure is shortness of breath . As the disease progresses, its intensity increases.
- Due to insufficient oxygen supply to the tissues, oxygen starvation develops, which is expressed in rapid fatigue , chronic fatigue .
- Stagnation of fluid in the lungs, associated with deterioration of hemodynamics in the pulmonary circulation, causes a wet cough .
- Enlargement of the ventricles leads to the fact that the heart needs to contract more often in order to push out the required amount of blood - the heart rate increases .
The chronic form is characterized by an increase in the manifestations of the disease. If at an early stage patients may not pay attention to them, then later the severity of symptoms increases and fatigue sets in faster. Even at rest, the patient feels significant shortness of breath, palpitations, at night his limbs swell, and in the morning he may experience pain in the heart area.
Development mechanism
Regardless of the disease that provoked acute heart failure, the mechanism of development of the pathological condition is approximately the same: the cardiac output and blood flow into the arterial system sharply decrease. The clinical picture is quite similar to acute vascular insufficiency.
The development of AHF begins with a pathological process that reduces the contractility of the muscles of one of the ventricles, or reduces the elasticity of the valves separating the atrium and ventricle. Weak muscle contraction pushes blood into the artery in a smaller volume, while some blood remains in the ventricle itself, and without complete contraction, the flow of new blood from the atrium also slows down.
In the case of chronic heart failure and mitral valve prolapse, the problem is solved due to compensatory mechanisms and the ability of the heart to adapt. In a situation of acute deficiency, the body does not have time to adapt, which increases the risk of death.
Functional classes of heart failure
- First . The patient is physically active and does not feel obvious signs of the disease.
- Second . The patient experiences well at rest, but physical activity causes symptoms of the disease to appear.
- Third . The patient is comfortable at rest, but much less physical activity is required for signs of the disease to appear.
- Fourth . Already at rest the patient feels discomfort, and with minimal exertion the symptoms increase sharply.
Classification
In addition to acute and chronic heart failure, there are:
- Left ventricular AHF, which occurs in 60-71% of cases, with timely medical care, about 70% of patients survive.
- Right ventricular AHF, responsible for 20-25% of cases, timely medical and pre-medical care ensures survival of 85% of patients.
- Biventricular, or bilateral AHF, which is diagnosed in 10% of patients and has an almost 100% probability of death. In rare cases, exit from the acute phase guarantees the patient's death within 2-3 years, even with full pharmacological support.
The rehabilitation period for any form of acute heart failure lasts at least six months, and surviving patients require lifelong medication.
Precursors and symptoms of AHF
The sudden development of acute heart failure is a fairly rare occurrence, usually associated with stress or injury. In other cases, even with heart attacks and strokes, there are a number of signs that, if not prevent AHF, then reduce the risk of death of the patient.
The time for reaction can be from several hours to two weeks, but in any case, the appearance of precursors of AHF cannot be ignored.
Seeing a doctor requires:
- unexpected increase in fatigue and a sharp decrease in performance;
- tachycardia and other unexpected heart rhythm disturbances;
- panic attacks;
- shortness of breath without exercise;
- severe swelling in the evenings, which almost completely disappears in the morning.
If we are talking about the rapid development of the condition, we already talk about symptoms of acute heart failure:
Right ventricular AHF always develops rapidly and is accompanied by:
- cyanosis of the skin;
- mild shortness of breath;
- pain in the right side;
- pressing and pulling sensations, burning behind the sternum;
- arrhythmia and tachycardia;
- swelling of the neck veins.
It takes from 5 minutes to 2 hours to resuscitate a patient with right ventricular AHF, so it is important to call an ambulance at the first sign.
Left ventricular AHF is characterized by three main features: cardiogenic shock, asthma and pulmonary edema. Other signs are also characteristic:
- intense shortness of breath even at rest;
- anxiety to panic attacks;
- a sharp drop in blood pressure to critical levels;
- pallor of the skin and cyanosis of the mucous membranes, cyanosis of the fingers and nasolabial triangle;
- sweating and hyperhidrosis;
- wheezing in the lungs and cough with a small amount of sputum;
- confusion, fainting, coma;
- dysuria.
In most cases, manifestations of left ventricular AHF are systemic and occur almost simultaneously. It happens that the symptoms suddenly go away and the patient’s condition stabilizes before the ambulance arrives - in this case, hospitalization is still necessary to prevent a sudden recurrence of the episode with more severe consequences.
ACUTE HEART FAILURE Diagnosis and treatment at the prehospital stage
What are the main causes of AHF? What is the classification of OSN based on? What is the treatment algorithm at the prehospital stage?
Acute heart failure (AHF), which is a consequence of impaired myocardial contractility and a decrease in systolic and cardiac output, is manifested by extremely severe clinical syndromes: cardiogenic shock, pulmonary edema, acute cor pulmonale.
Main causes and pathogenesis
A decrease in myocardial contractility occurs either as a result of its overload, or due to a decrease in the functioning mass of the myocardium, a decrease in the contractile ability of myocytes, or a decrease in the compliance of chamber walls. These conditions develop in the following cases:
- in case of disturbance of diastolic and/or systolic function of the myocardium during infarction (the most common cause), inflammatory or dystrophic diseases of the myocardium, as well as tachy- and bradyarrhythmias;
- with the sudden occurrence of myocardial overload due to a rapid significant increase in resistance in the outflow tract (in the aorta - hypertensive crisis in patients with compromised myocardium; in the pulmonary artery - thromboembolism of the branches of the pulmonary artery, a prolonged attack of bronchial asthma with the development of acute emphysema, etc.) or due to stress volume (an increase in the mass of circulating blood, for example, with massive fluid infusions - a variant of the hyperkinetic type of hemodynamics);
- in case of acute disturbances of intracardiac hemodynamics due to rupture of the interventricular septum or the development of aortic, mitral or tricuspid insufficiency (septal infarction, infarction or avulsion of the papillary muscle, perforation of the valve leaflets in bacterial endocarditis, rupture of the chordae, trauma);
- with increasing load (physical or psycho-emotional stress, increased inflow in a horizontal position, etc.) on the decompensated myocardium in patients with chronic congestive heart failure.
Classification
Depending on the type of hemodynamics, which ventricle of the heart is affected, as well as on some features of the pathogenesis, the following clinical variants of AHF are distinguished.
- With a congestive type of hemodynamics: • right ventricular (venous congestion in the systemic circulation); • left ventricular (cardiac asthma, pulmonary edema).
- With hypokinetic1 type of hemodynamics (small output syndrome - cardiogenic shock): • arrhythmic shock; • reflex shock; • true shock.
Since myocardial infarction is one of the most common causes of AHF, the table provides a classification of acute heart failure in this disease.
Possible complications
Any of the variants of AHF is a life-threatening condition. Acute congestive right ventricular failure, not accompanied by small output syndrome, in itself is not as dangerous as diseases leading to right ventricular failure.
Clinical picture
- Acute congestive right ventricular failure is manifested by venous congestion in the systemic circulation with increased systemic venous pressure, swelling of the veins (most noticeable in the neck), enlarged liver, and tachycardia. Edema may appear in the lower parts of the body (with prolonged horizontal position - on the back or side). Clinically, it differs from chronic right ventricular failure by intense pain in the liver area, aggravated by palpation. Signs of dilatation and overload of the right heart are determined (expansion of the borders of the heart to the right, systolic murmur over the xiphoid process and protodiastolic gallop rhythm, emphasis of the second tone on the pulmonary artery and corresponding ECG changes). A decrease in left ventricular filling pressure due to right ventricular failure can lead to a drop in left ventricular minute volume and the development of arterial hypotension, up to a picture of cardiogenic shock.
With pericardial tamponade and constrictive pericarditis, the pattern of large circle congestion is not associated with insufficiency of myocardial contractile function, and treatment is aimed at restoring diastolic filling of the heart.
Biventricular failure, a variant where congestive right ventricular failure is combined with left ventricular failure, is not discussed in this section, since the treatment of this condition is not much different from the treatment of severe acute left ventricular failure.
- Acute congestive left ventricular failure clinically manifests itself as paroxysmal shortness of breath, painful suffocation and orthopnea, occurring more often at night; sometimes - Cheyne-Stokes breathing, cough (initially dry, and then with sputum, which does not bring relief), later - foamy sputum, often pink in color, pallor, acrocyanosis, hyperhidrosis and is accompanied by excitement, fear of death. In case of acute congestion, moist rales may not be heard at first, or a meager amount of fine bubbling rales is detected over the lower parts of the lungs; swelling of the mucous membrane of small bronchi can manifest itself as a moderate picture of bronchial obstruction with prolongation of exhalation, dry wheezing and signs of pulmonary emphysema. A differential diagnostic sign that allows one to differentiate this condition from bronchial asthma can be the dissociation between the severity of the patient’s condition and (in the absence of pronounced expiratory dyspnea, as well as “silent zones”) the paucity of the auscultatory picture. Loud, varied moist rales over all the lungs, which can be heard at a distance (bubbling breathing), are characteristic of a detailed picture of alveolar edema. Possible acute expansion of the heart to the left, the appearance of a systolic murmur at the apex of the heart, a proto-diastolic gallop rhythm, as well as an emphasis on the second tone on the pulmonary artery and other signs of load on the right heart, up to the picture of right ventricular failure. Blood pressure can be normal, high or low, tachycardia is typical.
The picture of acute congestion in the pulmonary circulation, which develops with stenosis of the left atrioventricular orifice, essentially represents left atrial failure, but is traditionally considered together with left ventricular failure.
- Cardiogenic shock is a clinical syndrome characterized by arterial hypotension and signs of a sharp deterioration in microcirculation and tissue perfusion, including blood supply to the brain and kidneys (lethargy or agitation, drop in urine output, cold skin covered with sticky sweat, pallor, marbled skin pattern); sinus tachycardia is compensatory in nature.
A decrease in cardiac output with a clinical picture of cardiogenic shock can be observed in a number of pathological conditions not associated with insufficiency of myocardial contractile function - with acute obstruction of the atrioventricular orifice by an atrial myxoma or a spherical thrombus/ball prosthesis thrombus, with pericardial tamponade, with massive pulmonary embolism. These conditions are often combined with the clinical picture of acute right ventricular failure. Pericardial tamponade and atrioventricular orifice obstruction require immediate surgical intervention; drug therapy in these cases can only worsen the situation. In addition, the picture of shock during myocardial infarction is sometimes imitated by dissecting aortic aneurysm; in this case, differential diagnosis is necessary, since this condition requires a fundamentally different therapeutic approach.
There are three main clinical variants of cardiogenic shock:
- arrhythmic shock develops as a result of a drop in cardiac output due to tachycardia/tachyarrhythmia or bradycardia/bradyarrhythmia; after stopping the rhythm disturbance, adequate hemodynamics are quickly restored;
- reflex shock (pain collapse) develops as a reaction to pain and/or sinus bradycardia resulting from a reflex increase in vagal tone and is characterized by a rapid response to therapy, primarily painkillers; observed with relatively small infarct sizes (often in the posterior wall), while there are no signs of congestive heart failure and deterioration of tissue perfusion; pulse pressure usually exceeds a critical level;
- true cardiogenic shock develops when the lesion volume exceeds 40-50% of the myocardial mass (more often with anterolateral and repeated infarctions, in people over 60 years of age, against the background of arterial hypertension and diabetes mellitus), is characterized by a detailed picture of shock, resistant to therapy, often combined with congestive left ventricular failure; depending on the selected diagnostic criteria, the mortality rate ranges from 80-100%.
In some cases, especially when it comes to myocardial infarction in patients receiving diuretics, the developing shock is hypovolemic in nature, and adequate hemodynamics are relatively easily restored due to replenishment of the circulating volume.
Diagnostic criteria
One of the most consistent signs of acute heart failure is sinus tachycardia (in the absence of sinus node weakness, complete AV block, or reflex sinus bradycardia); characterized by expansion of the borders of the heart to the left or right and the appearance of a third sound at the apex or above the xiphoid process.
- In acute congestive right ventricular failure, the following are of diagnostic value: swelling of the neck veins and liver;
- Kussmaul's sign (swelling of the jugular veins on inspiration);
- intense pain in the right hypochondrium;
- ECG signs of acute overload of the right ventricle (type SI-QIII, increasing R wave in leads V1,2 and formation of a deep S wave in leads V4-6, depression of STI, II, a VL and elevation of STIII, a VF, as well as in leads V1, 2; possible formation of right bundle branch block, negative T waves in leads III, aVF, V1-4) and signs of right atrium overload (high pointed waves PII, III).
- shortness of breath of varying severity, up to suffocation;
- a drop in systolic blood pressure of less than 90-80 mm Hg. Art. (or 30 mmHg below the “working” level in people with arterial hypertension);
| Figure 1. Algorithm for relieving pulmonary edema at the prehospital stage |
| Figure 2. Algorithm for relieving cardiogenic shock at the prehospital stage |
Treatment of acute heart failure
In any variant of AHF, in the presence of arrhythmias, it is necessary to restore an adequate heart rhythm.
If the cause of AHF is myocardial infarction, then one of the most effective methods of combating decompensation will be the rapid restoration of coronary blood flow through the affected artery, which can be achieved at the prehospital stage using systemic thrombolysis.
Inhalation of humidified oxygen through a nasal catheter at a rate of 6-8 l/min is indicated.
- Treatment of acute congestive right ventricular failure consists of correcting the conditions that caused it - pulmonary embolism, status asthmaticus, etc. This condition does not require independent therapy.
The combination of acute congestive right ventricular and congestive left ventricular failure serves as an indication for therapy in accordance with the principles of treatment of the latter.
When acute congestive right ventricular failure and small output syndrome (cardiogenic shock) are combined, the basis of therapy is inotropic agents from the group of pressor amines.
- Treatment of acute congestive left ventricular failure.
- Treatment of acute congestive heart failure begins with the administration of sublingual nitroglycerin in a dose of 0.5-1 mg (1-2 tablets) and giving the patient an elevated position (in case of an unexpressed picture of congestion - an elevated head end, in case of advanced pulmonary edema - a sitting position with legs down) ; these measures are not performed in cases of severe arterial hypotension.
- A universal pharmacological agent for acute congestive heart failure is furosemide, due to venous vasodilation already 5-15 minutes after administration, causing hemodynamic unloading of the myocardium, which increases over time due to the diuretic effect that develops later. Furosemide is administered intravenously as a bolus and is not diluted; the dose of the drug ranges from 20 mg for minimal signs of congestion to 200 mg for extremely severe pulmonary edema.
- The more pronounced the tachypnea and psychomotor agitation, the more indicated is the addition of a narcotic analgesic to therapy (morphine, which, in addition to venous vasodilation and reducing preload on the myocardium, already 5-10 minutes after administration reduces the work of the respiratory muscles, suppressing the respiratory center, which provides an additional reduction load on the heart. A certain role is also played by its ability to reduce psychomotor agitation and sympathoadrenal activity; the drug is administered intravenously in fractional doses of 2-5 mg (for which 1 ml of a 1% solution is taken, diluted with isotonic sodium chloride solution, bringing the dose to 20 ml and administered 4-10 ml) with repeated administration if necessary after 10-15 minutes Contraindications are respiratory rhythm disturbances (Cheyne-Stokes breathing), depression of the respiratory center, acute obstruction of the respiratory tract, chronic pulmonary heart disease, cerebral edema, poisoning with depressant substances breath.
- Severe congestion in the pulmonary circulation in the absence of arterial hypotension or any degree of acute congestive left ventricular failure during myocardial infarction, as well as pulmonary edema against the background of a hypertensive crisis without cerebral symptoms, are an indication for intravenous drip administration of nitroglycerin or isosorbide dinitrate. The use of nitrate drugs requires careful monitoring of blood pressure and heart rate. Nitroglycerin or isosorbide dinitrate is prescribed at an initial dose of 25 mcg/min, followed by an increase every 3-5 minutes by 10 mcg/min until the desired effect is achieved or side effects appear, in particular a decrease in blood pressure to 90 mm Hg. Art. For intravenous infusion, every 10 mg of the drug is dissolved in 100 ml of 0.9% sodium chloride solution, so one drop of the resulting solution contains 5 mcg of the drug. Contraindications to the use of nitrates are arterial hypotension and hypovolemia, pericardial constriction and cardiac tamponade, pulmonary artery obstruction, and inadequate cerebral perfusion.
- Modern methods of drug treatment have minimized the importance of bloodletting and the application of venous tourniquets to the extremities, however, if adequate drug therapy is impossible, these methods of hemodynamic unloading not only can, but should be used, especially with rapidly progressing pulmonary edema (bloodletting in a volume of 300- 500 ml).
- In case of acute congestive left ventricular failure, combined with cardiogenic shock, or with a decrease in blood pressure during therapy that has not given a positive effect, non-glycoside inotropic agents are additionally prescribed - intravenous drip administration of dobutamine (5-15 mcg/kg/min), dopamine (5- 25 mcg/kg/min), norepinephrine (0.5-16 mcg/min) or a combination thereof.
- A means of combating foaming during pulmonary edema are “defoamers” - substances that ensure the destruction of foam by reducing surface tension. The simplest of these means is alcohol vapor, which is poured into a humidifier, passing oxygen through it, supplied to the patient through a nasal catheter or breathing mask at an initial rate of 2-3 l/min, and after a few minutes - at a rate of 6-8 l/min.
- Persistent signs of pulmonary edema with stabilization of hemodynamics may indicate an increase in membrane permeability, which requires the administration of glucocorticoids to reduce permeability (4-12 mg of dexamethasone).
- In the absence of contraindications, in order to correct microcirculatory disorders, especially with long-term intractable pulmonary edema, the administration of sodium heparin is indicated - 5 thousand IU intravenously as a bolus, then drip at a rate of 800 - 1000 IU/hour.
- Treatment of cardiogenic shock involves increasing cardiac output, which is achieved in a variety of ways, the significance of which varies depending on the clinical type of shock.
- In the absence of signs of congestive heart failure (shortness of breath, moist rales in the posterior lower parts of the lungs), the patient must be placed in a horizontal position.
- Regardless of the clinical picture, it is necessary to provide complete analgesia.
- Stopping rhythm disturbances is the most important measure to normalize cardiac output, even if adequate hemodynamics are not observed after restoration of normosystole. Bradycardia, which may indicate increased vagal tone, requires immediate intravenous administration of 0.3-1 ml of 0.1% atropine solution.
- If the clinical picture of shock is extensive and there are no signs of congestive heart failure, therapy should begin with the administration of plasma expanders in a total dose of up to 400 ml under the control of blood pressure, heart rate, respiratory rate and auscultation of the lungs. If there is an indication that immediately before the onset of acute cardiac damage with the development of shock, there were large losses of fluid and electrolytes (long-term use of large doses of diuretics, uncontrollable vomiting, profuse diarrhea, etc.), then an isotonic solution is used to combat hypovolemia sodium chloride; the drug is administered in an amount of up to 200 ml over 10 minutes, repeated administration is also indicated.
- The combination of cardiogenic shock with congestive heart failure or the lack of effect from the entire complex of therapeutic measures is an indication for the use of inotropic agents from the group of pressor amines, which, in order to avoid local circulatory disorders accompanied by the development of tissue necrosis, should be injected into the central vein: dopamine in a dose of up to 2, 5 mg affects only dopamine receptors of the renal arteries, at a dose of 2.5-5 mcg/kg/min the drug has a vasodilating effect, at a dose of 5-15 mcg/kg/min it has vasodilating and positive inotropic (and chronotropic) effects, and in dose 15-25 mcg/kg/min - positive inotropic (and chronotropic), as well as peripheral vasoconstrictive effects; 400 mg of the drug is dissolved in 400 ml of a 5% glucose solution, while 1 ml of the resulting mixture contains 0.5 mg, and 1 drop - 25 mcg of dopamine. The initial dose is 3-5 mcg/kg/min with a gradual increase in the rate of administration until the effect is achieved, the maximum dose (25 mcg/kg/min, although the literature describes cases where the dose was up to 50 mcg/kg/min) or the development of complications (most often sinus tachycardia exceeding 140 beats per minute, or ventricular arrhythmias). Contraindications to its use are thyrotoxicosis, pheochromocytoma, cardiac arrhythmias, hypersensitivity to disulfide, previous use of MAO inhibitors; if the patient was taking tricyclic antidepressants before prescribing the drug, the dose should be reduced;
- the lack of effect from dopamine or the inability to use it due to tachycardia, arrhythmia or hypersensitivity is an indication for the addition or monotherapy with dobutamine, which, unlike dopamine, has a more pronounced vasodilatory effect and a less pronounced ability to cause an increase in heart rate and arrhythmia. 250 mg of the drug is diluted in 500 ml of a 5% glucose solution (1 ml of the mixture contains 0.5 mg, and 1 drop - 25 mcg of dobutamine); in monotherapy, it is prescribed at a dose of 2.5 mcg/kg/min, increasing every 15-30 minutes by 2.5 mcg/kg/min until an effect, side effect is obtained, or a dose of 15 mcg/kg/min is achieved, and with a combination of dobutamine with dopamine - in maximum tolerated doses; Contraindications to its use are idiopathic hypertrophic subaortic stenosis and stenosis of the aortic mouth. Dobutamine is not prescribed for systolic blood pressure <70 mmHg. Art.
- in the absence of effect from the administration of dopamine and/or a decrease in systolic blood pressure to 60 mm Hg. Art. norepinephrine can be used with a gradual increase in dosage (maximum dose - 16 mcg/min). Contraindications to its use are thyrotoxicosis, pheochromocytoma, previous use of MAO inhibitors; If you have previously taken tricyclic antidepressants, the dose should be reduced.
Indications for hospitalization
After relief of hemodynamic disturbances, all patients with acute heart failure are subject to hospitalization in cardiac intensive care units. In the torpid course of AHF, hospitalization is carried out by specialized cardiology or resuscitation teams. Patients with cardiogenic shock should, whenever possible, be hospitalized in hospitals where there is a cardiac surgery department.
A. L. Vertkin, Doctor of Medical Sciences, Professor V. V. Gorodetsky, Candidate of Medical Sciences O. B. Talibov, Candidate of Medical Sciences
1 The clinical picture of cardiogenic shock can develop with a hypovolemic type of hemodynamics: against the background of active diuretic therapy preceding a heart attack, profuse diarrhea, etc.
Diagnostics
Doctors in specialized cardiology departments and resuscitators have too little time to carry out a full diagnosis, but in the process of stabilizing the patient’s condition they conduct the following studies:
- ECG for diagnosing heart rhythm disturbances.
- EchoCG to identify areas of organic damage.
- Chest X-ray.
- UAC urgent
- Determination of oxygen saturation in arterial blood to establish the level of hypoxia.
Having achieved complete stabilization of the patient’s condition, more in-depth studies are carried out:
- MRI and CT of the heart, cardiac structures, brain, adrenal glands.
- Angiography of large vessels
- Ultrasound to measure blood flow speed
- Radioisotope research
Invasive tests may be performed to clarify the diagnosis. Any load tests are strictly prohibited.
First aid algorithm
A patient with acute heart failure needs qualified care and a hospital with specialized equipment. however, the few actions that a person can take between the call and the arrival of an ambulance can significantly increase the likelihood of survival.
- Sit the patient so that there is support behind the back, place a bolster or pillow under the lower back. Lower and relax the limbs to restore normal nutrition to the myocardium and prevent a major infarction.
- Remove tight jewelry from the patient, untie the tie, unfasten the bra and belts.
- Provide fresh air flow - open windows or vents slightly
- Measure blood pressure and record readings. Give it to the arriving ambulance doctor.
- If symptoms of pulmonary edema appear, let the vapors of ethyl alcohol, vodka, any alcohol tincture, cognac or whiskey inhale - the alcohol vapors will slow down the development of edema.
- If anxiety develops, reassure the patient.
Important! Under no circumstances should you give the patient medications or perform chest compressions - this can significantly worsen the situation.
First aid for AHF
A patient with AHF must immediately receive emergency care, since cardiogenic shock may occur during a heart attack. At the same time, his skin turns pale, his blood pressure drops sharply, severe pain appears, and his pulse is practically not palpable. If you do not respond in time, swelling of the kidneys and lungs can quickly develop, which can lead to death.
In case of AHF, first aid is provided at the scene of the incident, while it is necessary to reduce the load and ensure the redistribution of blood flow by performing the following actions:
- Place the patient in a comfortable sitting position; to do this, lower his legs to the floor and raise his back.
- It is better to immerse your feet in a basin of hot water, reducing the flow of blood to the heart.
- Remove the patient from clothing and open the windows, ensuring maximum flow of fresh air.
- Call emergency doctors and report the symptoms of an attack.
- Apply a tourniquet in the groin area to each leg alternately (20 minutes), which will reduce the flow of blood into the myocardium.
- Provide the patient with emotional and physical peace; he is strictly forbidden to get up and walk.
If there are signs of AHF, you need to measure your blood pressure. If the upper reading is more than 90 mmHg, then 1 tablet of nitroglycerin should be placed under the patient’s tongue. After this, you need to monitor the pressure all the time. If necessary, you can give 1 more tablet after 7 minutes, but not more than 4 times.
Patients suffering from heart disease or hypertension with severe swelling of the legs and shortness of breath should always carry a first aid kit with medications prescribed by the attending physician. Then, at the first signs of AHF, people around you will be able to provide emergency assistance.
Treatment
Surgical intervention for acute heart failure is ineffective and is indicated only in rare cases, therefore the scheme for stopping and treating the condition is completely dependent on medications.
Stabilization of the patient's condition
To relieve the acute phase of heart failure it is necessary:
- Stop the panic attack and anesthetize the patient with drotaverine and paracetamol. Narcotic painkillers are indicated only in the most extreme cases, as they increase the risk of death and require careful dosing.
- Restore contractility of both ventricles and cardiac activity in general. Dopamine drugs and cardiac glycosides are used. Prohibited for proven heart attack.
- Unload the heart to restore normal blood flow to the minimum acceptable level. It is possible to use diuretics, organic nitrates, beta blockers, as well as tranquilizers and phenobarbital in precisely calculated dosages.
As a rule, these measures allow you to stabilize the patient’s condition and restore cardiac activity.
Maintenance therapy
The following are used as maintenance therapy:
- Corticosteroids intravenously for up to 4 weeks.
- Bronchodilators.
- Angioprotectors.
- Antithrombic drugs that help restore the rheological properties of blood. The optimal choice is Fasostabil, which blocks the synthesis of thromboxane A2 and prevents the formation of venous blood clots.
Consequences of OSN
Acute heart failure is dangerous in itself, and also has a number of complications, often fatal:
- Cardiogenic shock. Mortality is close to 100%. Occurs when blood pressure drops critically. Even if the patient survives, the average life expectancy is about 2 years with constant monitoring by a cardiologist.
- Pulmonary edema with the possibility of asphyxia and inability to breathe independently. It occurs due to impaired gas exchange and venous outflow. With complete removal of fluid from the lungs and relief of all signs of intoxication, there is a chance of survival for the patient.
- Myocardial infarction increases the likelihood of death by 30-40%. Occurs due to acute disruption of blood supply to cardiac structures
- Stroke. Characteristic damage to cerebral structures due to malnutrition. Accompanied by the death of active neurons in the affected area.
Features of treatment of AHF
If help was provided to the patient in a timely manner and the attack was stopped, he is transported to the intensive care unit. Treatment of patients with heart failure is aimed at maintaining the general condition of the body, eliminating dyspnea and signs of an attack. For this purpose, the following is carried out:
- elimination of bronchospasm using intravenous injections of aminophylline;
- analgesic therapy that allows you to quickly and effectively relieve pain;
- oxygen therapy, which involves the use of inhalers and oxygen masks to bring air into the lungs;
- infusion treatment, including drip or jet administration of medications to neutralize pathology and its consequences.
To prevent overload on the heart muscle, doctors use drugs that lower blood pressure and normalize the heart rate. Symptoms of heart failure are eliminated by intravenous administration of glycosides, and to avoid the appearance of edema, the patient is prescribed diuretics.
If conservative treatment of a patient with AHF carried out in a hospital setting does not bring a positive result, surgery is performed. The patient is fitted with a pacemaker, which maintains normal blood supply to the myocardium and filling of the ventricles with blood.
Prevention
A patient who has suffered acute heart failure is almost always forced to take maintenance medications for life. No more than half of the patients exceed the five-year survival threshold; subsequently, life expectancy depends on the severity of the condition suffered, general health, and correct lifestyle.
To avoid acute heart failure and all the risks that accompany it, it is necessary to take preventive measures:
- lead a healthy lifestyle;
- to walk alot;
- coordinate your diet and diet with a specialist;
- exclude alcohol, tobacco, stimulants;
- Avoid stress as much as possible;
- Learn calming and relaxing breathing techniques.
Social activity in a positive way will be beneficial: hobbies, communication with friends and family, participation in exhibitions, performances, travel. An optimal balance between activity and quiet rest will also reduce the risks of developing heart failure.